Abstract
In this study, we formulated and evaluated the effects of tablet dimensions and drug load on the characteristics of atropine sulfate (AS) fast-disintegrating sublingual tablets (FDSTs). We aim to develop AS FDSTs as an alternative non-invasive and portable dosage form for the emergency treatment of organophosphate (OP) toxicity. AS autoinjector, AtroPen®, is the only self-administered dosage form available as an antidote for-out-of-hospital emergency use, but it is associated with several limitations and drawbacks. Seven FDST formulations of two tablet sizes, 150 mg (A) and 50 mg (B), and of several AS loads, 0 mg (A1, B1), 2 mg (A2, B2), 4 mg (B3), and 8 mg (B4a, B4b), were formulated and manufactured by direct compression. AS FDST characteristics were evaluated using USP and non-USP tests. Results were statistically compared at p < 0.05. All FDSTs passed the USP content uniformity and friability tests, disintegrated and released AS in ≤30 and 60 s. B1 and B2 were significantly harder than A1 and A2. Water uptake of A1 was significantly the highest. However, B1 and B2 had shorter disintegration and wetting times and higher amounts of AS dissolved than did A1 and A2 (p < 0.05). Increasing AS negatively affected FDST tensile strength (p < 0.05 for B4a) and water uptake (p < 0.05 for B3, B4a and B4b), however, without affecting AS dissolution. Formulation of AS up to 16% into smaller FDSTs was successful. Smaller FDSTs were harder and disintegrated more quickly. These AS FDSTS have the potential for further in vivo testing to evaluate their OP antidote potential.








Similar content being viewed by others
REFERENCES
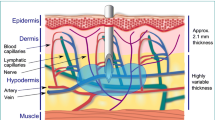
Nakajima K, Tagaya A, Otonari-Yamamoto M, Seki K, Araki K, Sano T, et al. Composition of the blood supply in the sublingual and submandibular spaces and its relationship to the lateral lingual foramen of the mandible. Oral Surg Oral Med Oral Pathol Oral Radiol. 2014;117(1):E32–8.
Zhang H, Zhang J, Streisand JB. Oral mucosal drug delivery: clinical pharmacokinetics and therapeutic applications. Clin Pharmacokinet. 2002;41(9):661–80.
Washington N, Washington CG, Wilson C. Drug delivery to the oral cavity or mouth. Physiological pharmaceutics: barriers to drug absorption. 2nd ed. London: Taylor and Francis; 2001. p. 37–58.
Wang Z, Chow MS. Overview and appraisal of the current concept and technologies for improvement of sublingual drug delivery. Ther Deliv. 2014;5(7):807–16.
Senel S, Rathbone MJ, Cansiz M, Pather I. Recent developments in buccal and sublingual delivery systems. Expert Opin Drug Deliv. 2012;9(6):615–28.
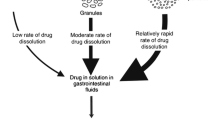
Nayak AK, Manna K. Current developments in orally disintegrating tablet technology. J Pharm Educ Res. 2011;2(1):21.
Rawas-Qalaji MM, Simons FER, Simons KJ. Sublingual epinephrine tablets versus intramuscular injection of epinephrine: dose equivalence for potential treatment of anaphylaxis. J Allergy Clin Immunol. 2006;117(2):398–403.
Rawas-Qalaji MM, Werdy S, Rachid O, Simons FE, Simons KJ. Sublingual diffusion of epinephrine microcrystals from rapidly disintegrating tablets for the potential first-aid treatment of anaphylaxis: in vitro and ex vivo study. AAPS PharmSciTech. 2015;16(5):1203–12.
Rawas-Qalaji M, Rachid O, Mendez BA, Losada A, Simons FE, Simons KJ. Adrenaline (epinephrine) microcrystal sublingual tablet formulation: enhanced absorption in a preclinical model. J Pharm Pharmacol. 2015;67(1):20–5.
Rawas-Qalaji MM, Simons FER, Simons KJ. Epinephrine for the treatment of anaphylaxis: do all 40 mg sublingual epinephrine tablet formulations with similar in vitro characteristics have the same bioavailability? Biopharm Drug Dispos. 2006;27(9):427–35.
Brown JH, Laiken N. Muscarinic receptor agonists and antagonists. In: Brunton LL, editor. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill; 2010.
Iyer R, Iken B, Leon A. Developments in alternative treatments for organophosphate poisoning. Toxicol Lett. 2015;233(2):200–6.
Eddleston M, Buckley NA, Eyer P, Dawson AH. Management of acute organophosphorus pesticide poisoning. Lancet. 2008;371(9612):597–607.
Zhao J, Yu S. Quantitative structure-activity relationship of organophosphate compounds based on molecular interaction fields descriptors. Environ Toxicol Pharmacol. 2013;35(2):228–34.
Wiener SW, Hoffman RS. Nerve agents: a comprehensive review. J Intensive Care Med. 2004;19(1):22–37.
Delaplane KS. Pesticide usage in the United States: history, benefits, risks, and trends. North Carolina Cooperative Extension; 1996. Available from: http://ipm.ncsu.edu/safety/factsheets/pestuse.pdf.
Bronstein AC, Spyker DA, Cantilena Jr LR, et al. 2011 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 29th annual report. Clin Toxicol. 2012;50(10):911–1164.
Mowry JB, Spyker DA, Cantilena Jr LR, Bailey JE, Ford M. 2012 annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 30th annual report. Clin Toxicol. 2013;51(10):949–1229.
Mowry JB, Spyker DA, Cantilena Jr LR, Bailey JE, Ford M. 2013 annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 31st annual report. Clin Toxicol. 2014;52(10):1032–283.
Mowry JB, Spyker DA, Cantilena Jr LR, Bailey JE, Ford M. 2014 annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 32nd annual report. Clin Toxicol. 2015;53(10):962–1147.
Convention on the Prohibition of the Development, Production, Stockpiling and Use of Chemical Weapons and on their Destruction. Organisation for the Prohibition of Chemical Weapons; 2005. Available from: https://www.opcw.org/fileadmin/OPCW/CWC/CWC_en.pdf.
Sellstrom A, Crains S, Barbeschi M. Report on the alleged use of chemical weapons in the Ghouta area of Damascus on 21 August 2013. United Nations Mission to Investigate Allegations of the Use of Chemical Weapons in the Syrian Arab Republic; 2013. Available from: http://www.securitycouncilreport.org/atf/cf/%7B65BFCF9B-6D27-4E9C-8CD3-CF6E4FF96FF9%7D/s_2013_553.pdf.
Eddleston M, Dawson A, Karalliedde L, Dissanayake W, Hittarage A, Azher S, et al. Early management after self-poisoning with an organophosphorus or carbamate pesticide—a treatment protocol for junior doctors. Crit Care. 2004;8(6):R391–7.
Atropine [Internet]. Elsevier’s Gold Standard. 2015 [cited 2016 Jun. 15]. Available from: http://www.goldstandard.com/product/drug-reference-patient-education/clinical-pharmacology/.
Yamane GK. Accidental injection of a U.S. Air Force aviator by a pralidoxime chloride auto-injector: a case report. Aerosp Med Hum Perform. 1999;70(11):1110–2.
Silverberg M, Manoach S. Accidental self-administration of epinephrine with an auto-injector. Clin Toxicol (Phila). 2007;45(1):83–4.
Tsai G, Kim L, Nevis IF. Auto-injector needle length may be inadequate to deliver epinephrine intramuscularly in women with confirmed food allergy. Allergy, Asthma Clin Immunol. 2014;10(1):39.
Bentur Y, Layish I, Krivoy A. Civilian adult self injections of atropine-trimedoxime (TMB4) auto-injectors. Clin Toxicol. 2006;44(3):301–6.
Topal E, Bakirtas A, Yilmaz O, Karagol IHE, Arga M, Demirsoy MS, et al. When should we perform a repeat training on adrenaline auto-injector use for physician trainees? Allergol Immunopathol. 2014;42(5):472–5.
Kanto J, Pihlajamaki K. Oropharyngeal absorption of atropine. Int J Clin Pharmacol Ther. 1986;24(11):627–9.
Heisler M, Hamilton G, Abbott A, Chengalaram A, Koceja T, Gerkin R. Randomized double-blind trial of sublingual atropine vs. placebo for the management of death rattle. J Pain Symptom Manag. 2013;45(1):14–22.
General Chapters: <1216> Tablet Friability. United States Pharmacopia. 39th ed. Rockville: Pharmacopeial Convention, Inc; 2016. p. 1609.
USP Monographs: Atropine Sulfate Tablets. United States Pharmacopeia. 39th ed. Rockville: United States Pharmacopeial Convention, Inc; 2016. p. 2642–3.
General Chapters: <711> Dissolution. United States Pharmacopea. 39th ed. Rockville: Pharmacopeia Convention, Inc; 2016. p. 540–51.
Aodah A, Bafail R, Rawas-Qalaji M. Development and validation of a simple disintegration test for rapidly disintegrating tablets. Orlando: American Association of Pharmaceutical Scientists Annual Meeting and Exposition; 2015. p. R61382015.
Rawas-Qalaji MM, Simons FER, Simons KJ. Fast-disintegrating sublingual tablets: effect of epinephrine load on tablet characteristics. AAPS PharmSciTech. 2006;7(2):E72–8.
Rawas-Qalaji MM, Simons FER, Simons KJ. Fast-disintegrating sublingual epinephrine tablets: effect of tablet dimensions on tablet characteristics. Drug Dev Ind Pharm. 2007;33(5):523–30.
Rachid O, Rawas-Qalaji M, Simons FER, Simons KJ. Dissolution testing of sublingual tablets: a novel in vitro method. AAPS PharmSciTech. 2011;12(2):544–52.
General Chapters: <1217> Tablet Breaking Force. United States Pharmacopea. 39th ed. Rockville: United States Pharmacopeial Convention, Inc; 2016. p. 1610.
Simons KJ, Rachid OM, Rawas-Qalaji MA, Wein M, Simons FER. Outdated epinephrine autoinjectors: ejection volume integrity and epinephrine content and dose. J Allergy Clin Immunol. 2012;129(2):Ab180-Ab.
Bourbonnais S, McMorran M, Wang Y. Twinject auto-injector and device malfunctions. Can Adverse React Newsl. 2008;18(3):3. 1p.
Kehe CR, Lasseter KC, Miller NC, Wick KA, Shamblen EC, Ekholm BP, et al. Comparative absorption of atropine from a metered-dose inhaler and an intramuscular injection. Ther Drug Monit. 1992;14(2):132–4.
Corcoran T, Venkataramanan R, Hoffman R. Systemic delivery of atropine sulfate by the microdose dry-powder inhaler. J Aerosol Med Pulm Drug Deliv. 2013;26(1):46–55.
Che MM, Conti M, Chanda S, Boylan M, Sabnekar P, Rezk P, et al. Post-exposure treatment with nasal atropine methyl bromide protects against microinstillation inhalation exposure to sarin in guinea pigs. Toxicol Appl Pharmacol. 2009;239(3):251–7.
Rajpal S, Ali R, Bhatnagar A, Bhandari SK, Mittal G. Clinical and bioavailability studies of sublingually administered atropine sulfate. Am J Emerg Med. 2010;28(2):143–50.
Volz-Zang C, Waldhauser T, Schulte B, Palm D. Comparison of the effects of atropine in vivo and ex vivo (radioreceptor assay) after oral and intramuscular administration to man. Eur J Clin Pharmacol. 1995;49(1–2):45–9.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aodah, A., Bafail, R.S. & Rawas-Qalaji, M. Formulation and Evaluation of Fast-Disintegrating Sublingual Tablets of Atropine Sulfate: the Effect of Tablet Dimensions and Drug Load on Tablet Characteristics. AAPS PharmSciTech 18, 1624–1633 (2017). https://doi.org/10.1208/s12249-016-0631-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-016-0631-y