Abstract
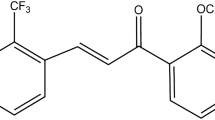
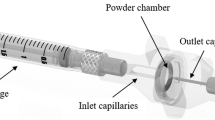
Inhalable lung surfactant-based carriers composed of synthetic phospholipids, dipalmitoylphosphatidylcholine (DPPC) and dipalmitoylphosphatidylglycerol (DPPG), along with paclitaxel (PTX), were designed and optimized as respirable dry powders using organic solution co-spray-drying particle engineering design. These materials can be used to deliver and treat a wide variety of pulmonary diseases with this current work focusing on lung cancer. In particular, this is the first time dry powder lung surfactant-based particles have been developed and characterized for this purpose. Comprehensive physicochemical characterization was carried out to analyze the particle morphology, surface structure, solid-state transitions, amorphous character, residual water content, and phospholipid bilayer structure. The particle chemical composition was confirmed using attenuated total reflectance-Fourier-transform infrared (ATR-FTIR) spectroscopy. PTX loading was high, as quantified using UV-VIS spectroscopy, and sustained PTX release was measured over weeks. In vitro cellular characterization on lung cancer cells demonstrated the enhanced chemotherapeutic cytotoxic activity of paclitaxel from co-spray-dried DPPC/DPPG (co-SD DPPC/DPPG) lung surfactant-based carrier particles and the cytotoxicity of the particles via pulmonary cell viability analysis, fluorescent microscopy imaging, and transepithelial electrical resistance (TEER) testing at air-interface conditions. In vitro aerosol performance using a Next Generation Impactor™ (NGI™) showed measurable powder deposition on all stages of the NGI and was relatively high on the lower stages (nanometer aerodynamic size). Aerosol dispersion analysis of these high-performing DPIs showed mass median diameters (MMADs) that ranged from 1.9 to 2.3 μm with excellent aerosol dispersion performance as exemplified by high values of emitted dose, fine particle fractions, and respirable fractions.

ᅟ










Similar content being viewed by others
References
American Cancer Society. Cancer Facts & Figures. In. Atlanta: American Cancer Society; 2013. p. 4–8.
Mansour HM, Rhee Y-S, Wu X. Nanomedicine in pulmonary delivery. Int J Nanomedicine. 2009;4:299–319.
Carvalho TC, Carbalho SR, McConville JT. Formulations for pulmonary administration of anticancer agents to treat lung malignancies. J Aerosol Med Pulm Drug Deliv. 2011;24(2):61–80.
Gagnadoux F, Hureaux J, Vecellio L, Urban T, Le Pape A, Valo I, et al. Aerosolized chemotherapy. J Aerosol Med Pulm Drug Deliv. 2008;21(1):61–9.
Sharma S, White D, Imondi A, Placke ME, Vail DM, Kris MG. Development of inhalation agents for oncologic use. J Clin Oncol. 2001;19(6):1839–47.
Gautam A. Targeted delivery of therapeutics by aerosol for cancer of the lung. Curr Cancer Drug Targets. 2003;3:57.
Haigentz MJ, Perez-Soler R. Chemopreventative therapeutics: inhalation therapies for lung cancer and bronchial premalignancy. Meth Mol Med. 2003;75:771–80.
Rubin BK. Mucus and mucins. Otolaryngol Clin N Am. 2010;43(1):27.
Laube BL, Janssens HM, de Jongh FHC, Devadason SG, Dhand R, Diot P, et al. What the pulmonary specialist should know about inhalation therapies. Eur Respir J. 2011;37:1308–31.
Weers JG, Bell J, Chan HK, Cipolla D, Dunbar C, Hickey AJ, et al. Pulmonary formulations: what remains to be done? J Aerosol Med Pulm Drug Deliv. 2010;23:S5–S23.
Labiris NR, Dolovich MB. Pulmonary drug delivery. Part II: The role of inhalant delivery devices and drug formulation in therapeutic effectiveness of aerosolized medications. Br J Clin Pharmacol. 2003;56:600–12.
Chow AHL, Tong HHY, Chattopadhyay P, Shekunov BY. Particle engineering for pulmonary drug delivery. Pharm Res. 2007;24(3):411–37.
Willis L, Hayes D, Mansour HM. Therapeutic liposomal dry powder inhalation aerosols for targeted lung delivery. Lung. 2012;190(3):251–62.
Eldar-Boock A, Miller K, Sanchis J, Lupu R, Vicent MJ, Satchi-Fainaro R. Integrin-assisted drug delivery of nano-scaled polymer therapeutics bearing paclitaxel. Biomaterials. 2011;32:3862–74.
Gill KK, Nazzal S, Kaddoumi A. Paclitaxel-loaded PEG5000-DSPE micelles as pulmonary delivery platform: formulation characterization, tissue distribution, plasma pharmacokinetics and toxicological evaluation. Eur J Pharm Biopharm. 2011;79:276–84.
Alipour S, Montaseri H, Tafaqhodi M. Preparation and characterization of biodegradable paclitaxel loaded alginate microparticles for pulmonary delivery. Colloids Surf B: Biointerfaces. 2010;81(2):521–9.
Mansour HM, Rhee YS, Park CW, DeLuca PP. Lipid nanoparticulate drug delivery and nanomedicine. In: Moghis A, editor. Lipids in nanotechnology. Urbana: American Oil Chemists Society (AOCS) Press; 2011. p. 221–68.
Jobe AH. Pulmonary surfactant therapy. N Engl J Med. 1993;328(12):861–8.
Labiris NR, Dolovich MB. Pulmonary drug delivery. Part I: Physiological factors affecting therapeutic effectiveness of aerosolized medications. J Clin Pharmacol. 2003;56:588–99.
Forbes B, Ehrhardt C. Human respiratory epithelial cell culture for drug delivery applications. Eur J Pharm Biopharm. 2005;60(2):193–205.
Grainger CI, Greenwell LL, Lockley DJ, Martin GP, Forbes B. Culture of Calu-3 cells at the air interface provides a representative model of the airway epithelial barrier. Pharm Res. 2006;23(7):1482–90.
Meenach SA, Anderson KW, Hilt JZ, McGarry RC, Mansour HM. Characterization and aerosol dispersion performance of advanced spray-dried chemotherapeutic PEGylated phospholipid particles for dry powder inhalation delivery in lung cancer. Eur J Pharm Sci. 2013;49(4):699–711.
Meenach SA, Vogt FG, Anderson KW, Hilt JZ, McGarry RC, Mansour HM. Design, physicochemical characterization, and optimization of organic solution advanced spray-dried inhalable dipalmitoylphosphatidylcholine (DPPC) and dipalmitoylphosphatidylethanolamine poly(ethylene glycol) (DPPE-PEG) microparticles and nanoparticles for targeted respiratory nanomedicine delivery as dry powder inhalation aerosols. Int J Nanomedicine. 2013;8:275–93.
Park CW, Li X, Vogt FG, Hayes DJ, Zwischenberger JB, Park ES, et al. Advanced spray dried design, physicochemical characterization and aerosol dispersion performance of vancomycin and clarithromycin multifunctional controlled release particles for targeted respiratory delivery as dry powder inhalation aerosols. Int J Pharm. 2013;455(1–2):374–92.
O’Hara P, Hickey AJ. Respirable PLGA microspheres containing rifampicin for the treatment of tuberculosis: manufacture and characterization. Pharm Res. 2000;17(8):955–61.
Sung JC, Padilla DJ, Garcia-Contreras L, VerBerkmoes JL, Durbin D, Peloquin CA, et al. Formulation and pharmacokinetics of self-assembled rifampicin nanoparticle systems for pulmonary delivery. Pharm Res. 2009;26(8):1847–55.
Salama RO, Traini D, Chan H-K, Young PM. Preparation and characterisation of controlled release co-spray dried drug–polymer microparticles for inhalation 2: evaluation of in vitro release profiling methodologies for controlled release respiratory aerosols. Eur J Pharm Biopharm. 2008;70:145–52.
Son Y-J, McConville JT. Preparation of sustained release rifampicin microparticles for inhalation. J Pharm Pharmacol. 2012;64:1291–302.
Son Y-J, McConville JT. Development of a standardized dissolution test method for inhaled pharmaceutical formulations. Int J Pharm. 2009;382:15–22.
El-Sherbiny IM, McGill S, Smyth HDC. Swellable microparticles as carriers for sustained pulmonary drug delivery. J Pharm Sci. 2010;99(5):2343–56.
El-Sherbiny IM, Smyth HDC. Biodegradable nano-micro carrier systems for sustained pulmonary drug delivery: (I) self-assembled nanoparticles encapsulated in respirable/swellable semi-IPN microspheres. Int J Pharm. 2010;395:132–41.
El-Sherbiny IM, Smyth HDC. Controlled release pulmonary administration of curcumin using swellable biocompatible microparticles. Mol Pharm. 2012;9:269–80.
<601> Aerosols, nasal sprays, metered-dose inhalers, and dry powder inhalers monograph. In. USP 29-NF 24 The United States Pharmacopoeia and The National Formulary: The Official Compendia of Standards. Rockville, MD: The United States Pharmacopeial Convention, Inc.; 2006. p. 2617–2636.
Edwards DA, Ben-Jebria A, Langer R. Recent advances in pulmonary drug delivery using large, porous inhaled particles. J Appl Physiol. 1998;85(2):379–85.
Finlay W. The ARLA respiratory deposition calculator. 2010. Available from: http://www.mece.ualberta.ca/arla/impactor_mmad_calculator.html.
Wu X, Hayes DJ, Zwischenberger JB, Kuhn RJ, Mansour HM. Design and physicochemical characterization of advanced spray-dried tacrolimus multifunctional particles for inhalation. Drug Des Dev Ther. 2013;7:59–72.
Wu X, Zhang W, Hayes DJ, Mansour HM. Physicochemical characterization and aerosol dispersion performance of organic solution advanced spray-dried cyclosporine A multifunctional particles for dry powder inhalation aerosol delivery. Int J Nanomedicine. 2013;8:1269–83.
Mansour H, Wang DS, Chen CS, Zografi G. Comparison of bilayer and monolayer properties of phospholipid systems containing dipalmitoylphosphatidylglycerol and dipalmitoylphosphatidylinositol. Langmuir. 2001;17(21):6622–32.
Alves GP, Santana MHA. Phospholipid dry powders produced by spray drying processing: structural, thermodynamic and physical properties. Powder Technol. 2004;145:139–48.
Elmore S. Apoptosis: a review of programmed cell death. Toxicol Pathol. 2007;35(4):495–516.
Hitzman CJ, Elmquist WF, Wattenberg LW, Wiedmann TS. Development of a respirable, sustained release microcarrier of 5-fluorouracil I: in vitro assessment of liposomes, microspheres, and lipid coated nanoparticles. J Pharm Sci. 2006;95(5):1114–26.
Sung JC, Pulliam BL, Edwards DA. Nanoparticles for drug delivery to the lungs. Trends Biotechnol. 2007;25(12):563–70.
Azarmi S, Roa WH, Lobenberg R. Targeted delivery of nanoparticles for the treatment of lung diseases. Adv Drug Deliv Rev. 2008;60:863–75.
Hureaux J, Lagarce F, Gagnadoux F, Vecellio L, Clavreul A, Roger E, et al. Lipid nanocapsules: ready-to-use nanovectors for the aerosol delivery of paclitaxel. Eur J Pharm Biopharm. 2009;73(2):239–46.
Mansour HM, Zografi G. Relationships between equilibrium spreading pressure and phase equilibria of phospholipid bilayers and monolayers at the air-water interface. Langmuir. 2007;23:3809–19.
Vehring R, Foss WR, Lechuga-Ballesteros D. Particle formation in spray drying. J Aerosol Sci. 2007;38(7):728–46.
Hickey AJ, Mansour HM, Telko MJ, Xu Z, Smyth HDC, Mulder T, et al. Physical characterization of component particles included in dry powder inhalers. I. Strategy review and static characteristics. J Pharm Sci. 2007;96(5):1282–301.
Hickey AJ, Mansour HM, Telko MJ, Xu Z, Smyth HDC, Mulder T, et al. Physical characterization of component particles included in dry powder inhalers. II. Dynamic characteristics. J Pharm Sci. 2007;96(5):1302–19.
Hickey AJ, Mansour HM. Delivery of drugs by the pulmonary route. In: Florence AT, Siepmann J, editors. Modern pharmaceutics. New York: Taylor and Francis; 2009. p. 191–219.
Edwards DA. The macrotransport of aerosol particles in the lung: aerosol deposition phenomena. J Aerosol Sci. 1995;26(2):293–317.
Suarez S, Hickey AJ. Drug properties affecting aerosol behavior. Respir Care. 2000;45(6):652–66.
Acknowledgments
The authors gratefully acknowledge financial support from the National Institutes of Health (NIH)-National Cancer Institute (NCI) Grant Number R25CA153954 and an NIH-NCI Cancer Nanotechnology Training Center (CNTC) Postdoctoral Traineeship awarded to SAM. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NCI or the NIH. The authors thank Dr. Tonglei Li for XRPD and HSM access and Dr. J. Zach Hilt for ATR-FTIR access.
Conflict of Interest
No conflicts of interest exist.
Author information
Authors and Affiliations
Corresponding author
Additional information
Guest Editors: Professor Paul B. Myrdal and Dr. Steve W. Stein
Rights and permissions
About this article
Cite this article
Meenach, S.A., Anderson, K.W., Hilt, J.Z. et al. High-Performing Dry Powder Inhalers of Paclitaxel DPPC/DPPG Lung Surfactant-Mimic Multifunctional Particles in Lung Cancer: Physicochemical Characterization, In Vitro Aerosol Dispersion, and Cellular Studies. AAPS PharmSciTech 15, 1574–1587 (2014). https://doi.org/10.1208/s12249-014-0182-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1208/s12249-014-0182-z