Abstract
Background
Subcapsular hematoma of the liver is a potentially life-threatening but extremely rare condition. It is often caused by a blunt trauma or other predisposing conditions such as a liver tumor, intra-tumor hemorrhage, surgery, preeclampsia, liver biopsy, and hemodialysis. Predisposing causes of liver hematoma include its large size and proximity to fixed structures. To date, there have been no reported cases of subcapsular liver hematoma caused by tight clothing such as corsets. Our case report is about an extremely rare case of subcapsular hematoma of the liver caused by wearing a tight faja corset in a young healthy female.
Case presentation
A forty-five-year-old Spanish female without any underlying health problems presented with sudden onset epigastric and right upper quadrant abdominal pain after wearing a faja corset the night prior to the hospital presentation. CT abdomen was noted for subcapsular hematoma of the liver. Her symptoms persisted and repeat CT abdomen showing worsening of the liver hematoma. Patient had interventional radiology (IR) guided drainage and was subsequently discharged home.
Conclusions
Subscapular liver hematomas need to be considered in patients presenting with acute onset abdominal pain after wearing certain tight clothing. The necessity of an early and accurate diagnosis is vital for management as hemodynamically stable patients can be managed conservatively. Our patient was managed with IR-guided aspiration drainage of the hematoma. Surgery can be considered a last resort in case of life-threatening hemodynamic instability, peritoneal signs, free abdominal fluid, and failure of arterial embolization. Our case highlights the importance of early recognition of traumatic subcapsular hematomas to prevent life-threatening complications.
Similar content being viewed by others
Background
Subcapsular hematoma of the liver is an extremely rare but potentially life-threatening condition. It is most commonly associated with blunt abdominal trauma, with the liver after spleen being the second most common abdominal organ injured during blunt trauma. Predisposing causes of liver hematoma include its large size and proximity to fixed structures. Other predisposing causes of liver hematoma include pregnancy, preeclampsia, hemodialysis, intra-tumor hemorrhage, surgery, and liver biopsy. To date, no cases have been reported of subscapular liver hematoma associated with tight clothing such as corsets. Here, we report the first case of a subcapsular hematoma of the liver in a young healthy female secondary to use of faja without any apparent anatomical lesion and in the absence of coagulopathy.
Case presentation
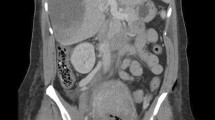
A forty-five-year-old Hispanic female without any significant past medical history was admitted to a community hospital with sudden onset of epigastric and right upper quadrant abdominal pain radiating to the back. She denied any nausea, vomiting, fever, or chills. Further history revealed that she wore a faja corset for a cultural event the night prior to hospital presentation. Patient did not report any other signs of trauma, fall, or history of abdominal surgery. She denied any trauma, fall, or history of abdominal surgery. Initial vitals were normal with temperature 36.8 °C, pulse 93, blood pressure 115/67, and saturation 98% on room air. Urine drug screen was negative. Beta-human chorionic gonadotropin (β-HCG) was negative. Laboratory workup was unremarkable with hemoglobin 12.3. Physical exam was noted for a hyposthenic body habitus. Abdominal exam findings were unremarkable except for some mild right upper quadrant tenderness and the liver was noted to be higher in the abdominal cavity. CT abdomen with contrast revealed a 5.5 × 4.2 × 14.2 cm subcapsular liver hematoma along the anterior aspect of the lateral left hepatic lobe (Figs. 1 and 2). It was also noted for an elongated cartilaginous tip of the xiphoid process (Fig. 3). Surgery team evaluated the patient and no intervention was recommended. She was subsequently discharged home. The next day, the patient presented again with worsening epigastric abdominal pain. Vitals were stable and hemoglobin was 10.0. CT abdomen with contrast showed worsening of subcapsular liver hematoma in the left hepatic lobe measuring 13.7 × 5.6 × 9.5 cm (Figs. 3 and 4). The liver otherwise showed normal enhancement without any fatty changes. Surgery recommended non-operative evacuation and patient subsequently underwent percutaneous IR-guided aspiration of enlarging liver hematoma to drain the fluid. Patient’s symptoms improved and repeat abdominal ultrasound showed decrease in size of liver hematoma. Patient was subsequently discharged home the following day (Fig. 5).
Discussion
A subcapsular hematoma of the liver is an accumulation of blood between the liver parenchyma and Glisson’s capsule. It has a 75% mortality rate if it ruptures into the peritoneal cavity [1]. In 75% of patients, it is located around the right lobe of the liver and only 25% of patients have involvement of the left lobe of the liver. Symptoms manifest as abdominal pain, anemia, hypotension, fever, and peritonism. Risk factors include blunt trauma, iatrogenic injuries following endoscopic retrograde cholangiopancreatography, anticoagulation treatment, liver tumors, hepatic adenomatosis, peliosis hepatis, hemodialysis, preeclampsia, and the HELLP syndrome [2, 3].
Our case is unique without any of the above risk factors commonly associated with hepatic subcapsular hematoma. One possible mechanism of hepatic hematoma in our patient is that an increase in intraabdominal pressure associated with tight clothing compresses the xiphoid process and results in bony trauma. The necessity of an early and accurate diagnosis in subcapsular hepatic hematomas derives its importance as patients who are hemodynamically stable can be managed conservatively. These patients are stable with a limited, peripheral, and non-compressive hematoma. Our patient was initially managed conservatively and discharged home after an observation period of 24 h. She presented to the hospital the following day with worsening symptoms and enlarging size of hepatic hematoma.
CT abdomen is the imaging of choice for diagnosing subcapsular hematoma of the liver. On CT imaging, the acute hematoma looks like a lenticular, ellipsoid, perihepatic collection that is typically, hyperdense (40–60 HU) due to its high protein content [4]. Although rare, these hepatic hematomas have potential to rupture that can rapidly lead to hemodynamic instability and death [5]. Therefore, these need close monitoring in an acute care setting. Patients can be safely discharged home if hemodynamically stable after a close period of observation.
Subcapsular hematomas of the liver associated with hemodynamic compromise, significant drop in hemoglobin, and in the presence of rapid expansion in size should have a low threshold for radiological or surgical intervention. Our patient was readmitted with worsening abdominal pain in the presence of increase in size of the hematoma. She subsequently underwent IR-guided drainage procedure of the hematoma. If IR-guided drainage does not result in resolution of the hematoma, then an arterial embolization performed by interventional radiology should be attempted. Surgery should be considered a last resort in case of life-threatening hemodynamic instability, peritoneal signs, free abdominal fluid, and failure of arterial embolization.
Conclusions
Subscapular liver hematomas can be observed in patients presenting with an acute onset abdominal pain after wearing certain tight clothing such as corsets. The necessity of an early and accurate diagnosis is vital for management as hemodynamically stable patients can be managed conservatively. Surgical intervention is necessary for subscapular hematomas of the liver associated with hemodynamic instability. Traumatic liver subscapular hematomas can be observed in hemodynamically stable patients and it is a real challenge for surgeons.
Availability of data and materials
Not applicable
References
Orea JG, Gavino I, Cardenas JL, Cuanalo A, Brachet S (1984) Rupture of the liver and subcapsular hematoma caused by toxemia. A case successfully treated by left lobectomy. Ann Chir. 38:19–22
Behranwala KA, Tisdall M, Habib NH, Canelo R (2004) Spontaneous bilobar subcapsular hematoma of the liver while undergoing anticoagulation therapy: our experience and review of the literature. Int Surg. 89:212–216
Ulu EM, Uyusur A, Ekici Y, Hunca Ç, Coşkun M (2009) Multidetector CT findings of spontaneous rupture of hepatic adenoma in a patient with hepatic adenomatosis. Diagn Interv Radiol. 15:135–138
Badea R, Chiorean L, Mitre C, Botar-Jid C, Caraiani C (2013) Spontaneous retroperitoneal and subcapsular liver hematoma: the diagnostic contribution of CT, US and CEUS, Case report. Medical Ultrasonography. 15(2):157–160
González-López R, García-Cano E, Espinosa-González O, Cruz-Salgado Á, Montiel-Jarquin ÁJ, Hernández-Zamora V (2015) Surgical treatment for liver haematoma following endoscopic retrograde cholangiopancreatography; an unusual case. Cir Cir. 83:506–509
Acknowledgements
None
Disclosures
There is no relationship with any industry
Funding
The authors received no funding for the study.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript. SM: leading author, supervised, implemented study, and final review. AM: worked on introduction. MM: worked on conclusion. PS: working on clinical case and provided review/editing
Authors’ information
None
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was waived for this case report; not applicable
Consent for publication
Written consent to publish this information was obtained from the case subject.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Minhas, S., Minhas, A., Malik, M. et al. Large subcapsular hematoma of the liver due to faja corset: a rare case report. Egypt Liver Journal 10, 32 (2020). https://doi.org/10.1186/s43066-020-00041-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43066-020-00041-z