Abstract
Background
Recently, the living donor liver transplantation (LDLT) surgery is employed as the treatment of choice for end-stage chronic liver disease and hepatocellular carcinoma. The role of liver biopsy in donor’s selection protocol for adult living liver donors (LLDs) candidates is a point of controversy. Hepatic magnetic resonance elastography (MRE) is a promising technique particularly in grading of liver fibrosis that can be used for pre-transplantation evaluation of the LLDs candidates. The aim of the current study was to evaluate the diagnostic performance of hepatic MRE as a pre-transplantation imaging tool for LLDs candidates, prior to LDLT surgery.
Results
Thirty-seven eligible healthy LLDs candidates (28 males and 9 females; their ages ranged from 24 to 45 years) were the subject of the current study. A cut-off value ≥ 2.24 kilo Pascal (kPa) was assumed for discrimination between normal and abnormal hepatic tissues with high accuracy (99.24%). Also, a cut-off value ≥ 2.38 kPa for grading steatosis gave 98.44% accuracy, while a cut-off value ≥ 2.57 kPa for discriminating fibrosis stages yielded 98.80% accuracy.
Conclusion
MRE can be considered as a reliable non-invasive pre-transplant screening technique that has the potential to alternate the invasive liver biopsy technique in selection and validation of LLDs candidates for LDLT surgery.
Similar content being viewed by others
Background
Over the last few years, the living donor liver transplantation (LDLT) surgery is commonly employed as a curative therapeutic strategy and the treatment of choice for end-stage chronic liver disease and hepatocellular carcinoma, particularly in the developing countries [1]. Consequently, the urge for living liver donors (LLDs) transplants has significantly increased [2]. In order to evade the operative risks, pre-operative thoroughgoing accurate investigation of the living donors’ livers is crucial and has become an integral part of the transplant programme [3].
Although liver biopsy is considered as the diagnostic gold standard for hepatic fibrosis and steatosis, its role in donor’s selection protocol for adult LLDs is a point of controversy [3, 4]. Actually, it is limited by being an invasive technique associated with complications such as hemorrhage, infection, and sampling errors that may reduce its diagnostic accuracy, in addition to the accompanying medical costs and the added potential risks for the donors [5]. The inhomogeneous distribution of necro-inflammation and fibrosis of chronic liver diseases such as chronic hepatitis C often interferes with the accurate interpretation of a liver biopsy [6]. To overwhelm these limitations, numerous non-invasive imaging techniques have been suggested for the assessment of adult LLDs including ultrasonography (US), computed tomography (CT), and magnetic resonance imaging (MRI) techniques. However, the capability to diagnose fibrosis, steatosis, or steatohepatitis inflammation by these tools is still limited [7].
Over the last decade, stiffness imaging tools have gained attention in hepatic grade of fibrosis and steatosis, and differentiation between malignant and benign hepatic lesions [8, 9]. Magnetic resonance elastography (MRE) is a stiffness imaging modality based on the transmission of low-frequency longitudinal wavelengths that penetrate the organ and transformed into transversal wavelengths, called cuts or shears, which are propagated through the organs’ parenchymal tissue and measured, from the shear modulus, in kilo-Pascals (kPa) [10]. Moreover, hepatic MRE is a promising technique that has a great potential for clinical applications, particularly in grading of liver fibrosis, because of its capability to measure the stiffness from a larger volume of liver with high diagnostic accuracy [11, 12].
To safeguard the LLD candidates from the possible risks of invasive liver biopsy procedure, the study in hand was basically deigned to investigate the potential for replacing hazardous invasive biopsy of livers in LLDs candidates by a reliable non-invasive imaging tool. Therefore, we aimed to evaluate the diagnostic performance of MRE as a pre-transplantation imaging tool for LLDs candidates via discrimination between normal and abnormal hepatic tissue, prior to LDLT surgery. Additionally, we tried to propose optimal cut-off values of liver stiffness measurements by MRE compared to the histopathological results of liver biopsy.
Methods
Study participants and design
The current prospective observational study was carried out in the period from September 2017 to September 2018. Study participants were recruited from apparently normal volunteers or relatives of end-stage hepatic patients, who were scheduled for LDLT in our institutions. Among 114 consecutive LLDs candidates with no underlying hepatic disease, who were meticulously screened and investigated after giving their agreement to donate hepatic tissue, only 37 LLDs candidates (28 males and 9 females with their ages ranged from 24 to 45 years and mean age of 34.55 years) were ultimately eligible to be the subjects of the present study. They were all selected on the basis of clinical and conventional imaging data, as well as, laboratory results.
The study inclusion criteria were no focal hepatic lesion (on any used imaging tool including US, Doppler US, multi-detector CT, and conventional MRI), no prior history of any hepatic disease, no prior history of abdominal operations, average range of laboratory tests, normal viral serology, as well as, stable AST and ALT within the last 6 months and thereafter (serum levels of AST and ALT equal to or above 37 unit/L and 40 unit/L, respectively, were considered abnormal [13]).
On the other hand, we excluded donors with unfavorable hepatic parenchymal, vascular, or biliary morphology as revealed by imaging studies preceding the LDLT, donors with moderate or severe steatosis (more than 30%) on pre-operative liver biopsy [14], individuals without liver biopsy, co-infection with chronic HBV, and/or HCV or any other liver disease that might influence hepatic parenchyma and the extent of liver stiffness such as congestive heart disease, liver failure, chronic renal disease, hemochromatosis, hepatolenticular degeneration, biliary obstructive disease, and fatty liver, in addition to subjects with ascites and subjects who received antiviral and/or interferon therapy throughout the study period were also excluded. Moreover, subjects with relative or absolute contraindications to MRI
An official approval to accomplish this work was attained from the local institutional research ethical committee. Also, an informed written consent was obtained from all study participants.
Clinical assessment
As a part of the pre-hepatic donation work-up in our institutions, all of the included eligible donors were subjected to meticulous history taking and the included donors were subjected to thorough clinical examination with estimation of the body mass index (BMI) and the appropriate laboratory investigations.
Imaging procedures
All included eligible donors were imaged by:
The standard hepatic MRI protocol
All study participants underwent evaluation by standard hepatic MRI protocol. They were fasting for at least 6 h prior to MRI examination. All MRI sequence images, including the MRE technique, were obtained by using 1.5 Tesla (Signa HDx; GE Healthcare, Milwaukee, WI, USA) with eight-channel torso phased-array body coil and respiratory triggering, as well as an additional MRE capability hardware to generate mechanical waves. The standard hepatic imaging protocol of our institutions with the used MRI sequences and parameters were summarized in Table 1.
The MRE technique
In all eligible donors and prior to the transplantation surgery, with an interval period ranged from 6 to 18 days with a mean of 8.75 days, liver stiffness was prospectively estimated by using a two-dimensional (2D) MRE protocol, which was achieved by using a commercially available MRE hardware (MR-Touch; GE Healthcare, Milwaukee, WI, USA) that added to the MRI machine. Additionally, dynamic MRI was performed, after finishing the MRE sequence images, via injection of 0.1 mmol/kg body weight of gadolinium diethylenetriamine penta-acetic acid (Gd-DTPA) (Omniscan; Amersham, Princeton, NJ) in the anti-cubital fossa after being flushed with 20 ml of sterile 0.9% saline solution.
To gain the MRE sequence images, the following parameters were utilized: repetition time/echo time (TR/TE) of 100/26.8 ms; flip angle (FA) of 30°; field of view (FOV) of 32 × 37 cm; matrix size of 320 × 264; slice thickness, 10 mm; and a 3-mm inter-slice gap. The confidence map image, on which the less reliable hepatic zones for stiffness estimation were shaded, crossed, and omitted, while the valid hepatic zones for stiffness measurement were delineated for placing the regions of interest (ROIs) so as to accurately estimate the hepatic stiffness. The technique of generating hepatic MRE images was illustrated in (Fig. 1a and b), which was quoted from many authors [10, 15, 16], while Fig, 1c demonstrates the MRE machine that used in the current study.
a–c Demonstrates illustrative images, which highlight the area of placing the MRE passive driver on the donor’s liver at the level of xiphisternum (a), as well as components and generated images of MRE technique (b), (Quoted from Stoopen-Romettia et al. [10], Venkatesh et al. [15], and Gallegos-Orozco et al. [16]). Furthermore, c image demonstrates the MRE machine, which was utilized in this study
After finalization of the data acquisition with the obtained information, they were automatically generated and displayed on the commercially available work station screen (GE AW workstation) in the form of 4 different appearance images; the reference image, which is a low-resolution gray-scale image that is used to select the areas of the hepatic parenchyma that could be measured, the colored wave image that showed the advance of the wavelengths into the liver tissue, the colored elastographic map image that demonstrates the liver stiffness in kilopascal (kPa), and a confidence image, which is attached to each elastographic map.
The generated MRE images were post-processed and prospectively interpreted with quantitative analysis of all obtained imaging data by a team of two experienced radiologists (RE and MA), with 8 and 7 years of experience in hepatic MRE imaging and techniques of liver stiffness imaging tools, respectively.
Multiple circular regions of interest (ROIs) were manually drawn and placed on the valid confident hepatic zones for stiffness estimation on the colored confidence maps, in which the valid stiffness areas were clearly demonstrated and demarcated on the elastogram and displayed according to the color scale of the color-coded map, ranging from blue to red; where blue color demonstrated the lowest stiffness and the red color revealed the highest stiffness. The mean of the ROIs with highest stiffness was calculated.
Liver biopsy and histopathological evaluation
All subjects underwent ultrasound-guided liver biopsy, which obtained from the same area evaluated by the MRE, within 1 week after the MRE. The liver biopsy was done by an experienced interventional radiologist (HO) with 7 years of experience in the field of interventional radiology. All the biopsy specimens were analyzed by a qualified pathologist to quantify the amount of fat contents, detect fibrosis or hidden inflammation.
The liver fibrosis (F) was staged according to the METAVIR scoring system [11], which ranges from F0 to F4 (F0 = no fibrosis; F1 = portal fibrosis without septa; F2 = portal fibrosis with a few septa; F3 = numerous septa without cirrhosis; F4 = cirrhosis) with a METAVIR fibrosis stage of F2 or higher was considered to represent significant fibrosis. The liver steatosis (S) was graded based on the percentage of hepatocytes with macrovesicular fat: grade S0 (no steatosis up to less than 5%); grade S1 (mild steatosis, equal to or greater than 5% up to 33%), which can be sub-classified into grade S1a (steatosis, equal to or greater than 5% up to less than 20%) and S1b (steatosis equal to or greater than 20% up to 33%); grade S2 (moderate steatosis, 34% to 66%); and grade S3 (severe steatosis, greater than 66%) [17].
In each included eligible candidate, the obtained MRE data were recorded and compared to the results of liver biopsy and then categorized as normal or abnormal.
Statistical analysis
The SPSS for Windows version 18.0 software package (SPSS Inc, Chicago, IL) was used for statistical data analysis. The Fisher’s exact test and Tukey’s test were used to compare and correlate the given data. P value below 0.05 (P < 0.05) was considered statistically significant. The final histopathological diagnosis was considered as the reference standard. Moreover, to assess the diagnostic proficiency of MRE in pre-transplant assessment of LLDs candidates, the receiver operating characteristic (ROC) curves were plotted with the optimal cut-off values and corresponding areas under the curves (AUCs) were calculated to evaluate sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of MRE.
Results
The current prospective study included 37 consecutive eligible healthy LLD candidates. They were 28 (75.68%) males and 9 (24.32 %) females with their ages ranged from 24 to 45 years (mean; 34.55 ± 9.45 years) and their BMI ranged from 17.55 to 50.60 kg/m2 (mean ± SD; 34.05 ± 8.14 kg/m2). As shown in Table 2, most of the study participants had absolutely normal hepatic tissue without fibrosis or steatosis (26/37; 70.27%), with most of them were males (19/26; 73.08%), aged less than 35 years (23/26; 88.46%) and had BMI less than 25 kg/m2 that ranged from 17.55 to 24.96 kg/m2 with mean of 23.89 ± 4.17 kg/m2 (24/26; 92.31%) with significant statistical differences between LLDs with normal and abnormal hepatic tissues regarding age, gender, and BMI (P < 0.003, P < 0.02, and P < 0.001; respectively).
As demonstrated by Table 3, we observed that the liver stiffness values in LLDs were not significantly affected by age nor gender (P = 0.0687 and P = 0.60; respectively). On the other hand, liver stiffness was significantly higher in candidates with BMI ≥ 25 kg/m2 compared to those with BMI < 25 kg/m2 (P < 0.001).
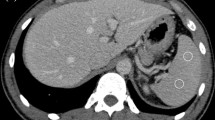
Absolutely normal hepatic parenchyma was observed in most of LLDs of the current study (26; 70.27%) and their mean liver stiffness measurement was 1.72 ± 0.30 kPa (Fig. 2).
a–g Demonstrates MRE sequence images of 28-year-old healthy normal LLD candidate with absolutely normal hepatic parenchyma and without neither steatosis nor fibrosis. The obtained MRE sequence images include the conventional anatomical reference image of MRE single slice (a) and the corresponding color-coded shear wave images (b, c), which were obtained by using vibration of 60 Hz, as well as the MRE inversion algorithm processed images including the color-coded elastogram with 0–8 kPa and 0–20 kPa (d, f, respectively), in addition to their associated confidence map images (e, g, respectively), in which the unsuitable portions for stiffness measurements were omitted (the shaded areas). The conventional anatomical reference image (a) reveals apparently normal hepatic tissue. The analysis of the corresponding color-coded shear wave images show narrow, regular, and shorter lengths of the obtained shear waves throughout the liver parenchyma, particularly in the right hepatic lobe (the arrows in b, c images). Also, the color-coded elastogram with 0–8 kPa and 0–20 kPa (d, f, respectively), as well as their associated color-coded confidence map images (e, g, respectively), demonstrate low hepatic stiffness, in which the valid portion for stiffness measurements were stained with blue (e) and purple (g) colors. According to the images’ corresponding color bars, these colors demonstrate the lowest stiffness. The mean estimated stiffness value of the liver, in the manually drawn ROIs, on the confidence maps (red and yellow rings on e and g images, respectively), was 1.90 kPa (average stiffness). The liver biopsy confirmed these findings
Mild steatosis was found in 6 (16.22%) LLDs. They were 4 (10.81%) candidates with grade S1a and their mean liver stiffness was 2.01 ± 0.11 kPa (Fig. 3), and 2 (5.41%) candidates with grade S1b and their mean liver stiffness was 2.40 ± 0.15 kPa (Fig. 4). Additionally, we detected fibrosis in 5 (13.51%) LLDs. They were 3 (8.11%) candidates with F1 stage of METAVIR score (their mean liver stiffness was 2.23 ± 0.40 kPa) (Fig. 5) and 2 (5.41%) candidates of with F2 stage of METAVIR score (their mean liver stiffness was 2.55 ± 0.25 kPa) (Fig. 6). Moreover, the liver stiffness measurements estimated by MRE were highly significantly related to the histopathological results of liver biopsy (P < 0.0003). Noteworthy, Tukey’s test highlighted the statistically significant differences in all comparisons of the MRE liver stiffness measurements among the studied LLDs (P < 0.05). All these data were illustrated in Table 4.
a–d Demonstrates MRE sequence images of a 37-year-old apparently normal LLD candidate with mild hepatic steatosis of grade S1a and the estimated mean stiffness of the liver was 2.33 kPa. The obtained MRE sequence images include the conventional anatomical reference image of MRE single slice (a) and the corresponding shear wave images (b), as well as the color-coded confidence map images with 0–8 kPa and 0–20 kPa (c, d, respectively). The conventional anatomical reference image (a) reveals apparently normal hepatic tissue, while the analysis of the corresponding color-coded shear wave image (b) show slightly wide, and longer wave length of the liver, particularly in the right hepatic lobe (the arrows in b image). Moreover, the color-coded confidence maps with 0–8 kPa and 0–20 kPa (c and d, respectively), display mainly blue color with green foci (c), as well as, mainly purple color with blue foci (d). According to the corresponding color bars, these colors represent relatively increased tissue stiffness with the mean estimated stiffness values of the liver in the ROIs, on confidence maps (red and yellow rings on c and d images, respectively), was 2.30 kPa (stiffness of grade S1a steatosis). Moreover, the liver biopsy confirmed these findings
a–c Demonstrates MRE sequence images of 43-year-old apparently normal LLD candidate with 32% hepatic steatosis of grade S1b (≥ 20%) and the estimated mean stiffness of the liver was 2.33 kPa. The obtained MRE sequence images include; the shear wave image (a), as well as the color-coded confidence map images with 0–8 kPa and 0–20 kPa (b and c, respectively). The color-coded shear wave image (a) show wide, irregular, and longer wave length of the liver, particularly in the right hepatic lobe (the arrows in image a). Moreover, the color-coded confidence map with 0–8 kPa (b) demonstrates 2 greenish-yellow areas on a light blue background, while on the color-coded confidence map with 0–20 kPa (c), they exhibit light blue color on a light purple background. According to the associated color bars, these colors reflect the increased tissue stiffness with the mean estimated stiffness values of the liver in the ROIs, on confidence maps (red rings on b and c images) was 2.30 kPa (stiffness of grade S1b steatosis). Moreover, the liver biopsy confirmed these findings
a–e Demonstrates MRE sequence images of a 40-year-old LLD candidate with mild hepatic fibrosis of F1 stage, according to METAVIR score of fibrosis, and the estimated mean stiffness of the liver was 2.39 kPa. The obtained MRE sequence images include; the conventional anatomical reference image of MRE single slice (a) and the corresponding shear wave images (b), as well as the color-coded elastogram and associated confidence map with 0–8 kPa (c and d, respectively), in addition to the color-coded confidence map image with 0–0 kPa (e). The conventional anatomical reference image (a) reveals apparently normal hepatic tissue, while the analysis of the corresponding color-coded shear wave image (b) show thick, wide, irregular, and longer wave length throughout the liver, particularly in the right hepatic lobe (the arrows in image b). Moreover, the valid area for hepatic stiffness estimation in color-coded confidence map with 0–8 kPa (d) stained with light blue colour with associated area with light green color, while it displayed light blue colour with purple background on confidence map with 20 kPa (e). According to the corresponding color bars, these colors represent increased tissue stiffness with the mean estimated stiffness values of the liver in the ROIs, on confidence maps (red and yellow rings on c and d images, respectively) was 2.39 kPa (stiffness of stage F1 fibrosis). Moreover, the liver biopsy confirmed these findings
a–d Demonstrates MRE sequence images of a 45-year-old apparently normal LLD candidate with hepatic fibrosis of F2 stage, according to METAVIR score of fibrosis, and the estimated mean stiffness of the liver was 2.58 kPa. The obtained MRE sequence images include the conventional anatomical reference image of MRE single slice (a) and the corresponding shear wave images (b), as well as the color-coded confidence map images with 0–8 kPa and 0–20 kPa (c and d, respectively). The conventional anatomical reference image (a) reveals apparently normal hepatic tissue, while the analysis of the corresponding colour-coded shear wave image (b) show very thick, wide, and irregular, and longer wave length throughout the liver, particularly in the right hepatic lobe (the arrows in image b). Moreover, the valid area for hepatic stiffness estimation in color-coded confidence map with 0–8 kPa (c), mainly stained with yellow colour on a light greenish-blue background (d), while it displays light green color on a light blue background on confidence map with 20 kPa (e). According to the corresponding color bars, these colors represent increased tissue stiffness with the mean estimated stiffness values of the liver in the ROIs, on confidence maps (red and yellow rings on c and d images, respectively) was 2.58 kPa (stiffness of F2 stage of fibrosis). Moreover, the liver biopsy confirmed these findings
As shown in Table 5 and Fig. 7, the ROC curves were plotted to detected steatosis and fibrosis in the livers of the studied LLDs. In the present study, a cut-off value ≥ 2.24 kPa with 0.992 AUC was proposed for discrimination between absolutely normal hepatic tissue and abnormal hepatic tissue (with steatosis and/or fibrosis) with high specificity (100%), sensitivity (98.65%), and accuracy (99.24%). Additionally, by using cut-off values ≥ 2.35 kPa with 0.981 AUC (100% specificity, 96.83% sensitivity, and 98.10% accuracy) and ≥ 2.42 with 0.990 AUC (100% specificity, 97.51% sensitivity, and 99% accuracy), we accurately identified mild hepatic steatosis of grade ≥ S1 (with fat contents ≥ 5%), and detected mild hepatic fibrosis of ≥ F1 stage METAVIR score of fibrosis, respectively in the livers of the studied LLDs. Furthermore, based on liver stiffness estimated by MRE, we suggested a cut-off value ≥ 2.38 kPa for discrimination between steatosis < 20% and steatosis ≥ 20% with 0.984 AUC (100% specificity, 96.90% sensitivity, and 98.44% accuracy). Moreover, we suggested a cut-off value ≥ 2.57 kPa with 0.988 AUC (100% specificity, 97.22% sensitivity, and 98.80% accuracy), for discrimination between F1 stage of fibrosis and F2 or more stages of fibrosis.
a–e Demonstrates the ROC curve analysis of the diagnostic reliability of MRE technique in the pre-transplant evaluation of the studied LLDs candidates. The MRE was accurately discriminated between absolutely normal and abnormal hepatic tissues by using an optimal cut-off value of liver stiffness value ≥ 2.24 kPa with 0.992 AUC, 98.65% sensitivity, 100% specificity, and 99.24% accuracy (a). Moreover, MRE technique was accurately detected hepatic steatosis of grade ≥ S1a by utilizing a cut-off value of liver stiffness ≥ 2.35 kPa with 0.981 AUC, 96.83% sensitivity, 100% specificity, and 98.10% accuracy, while it detected hepatic steatosis of grade ≥ S1b at a cut-off value of liver stiffness ≥ 2.38 kPa with 0.984 AUC, 96.90% sensitivity, 100% specificity, and 98.44% accuracy (b and c, respectively). Additionally, MRE technique identified fibrosis of grade ≥ F1 by using an optimal cut-off value of liver stiffness ≥ 2.42 kPa with 0.990 AUC, 97.51% sensitivity, 100% specificity, and 99% accuracy, while it detected hepatic fibrosis of grade ≥ F2 by using an optimal cut-off value of liver stiffness ≥ 2.57 kPa with 0.988 AUC, 97.22% sensitivity, 100% specificity, and 98.80% accuracy (d and e, respectively)
Discussion
Liver transplantation is an imperative procedure for treatment of hepatic failure and early stages of hepatocellular carcinoma. The suitability of donors has been decided by the surgeons on the basis of prerequisite investigation data and liver biopsy results [2]. The livers of LLDs are investigated for the existence of steatosis or fibrosis, which excludes transplant candidacy and results in poor post-operative outcome [3]. Despite liver biopsy is traditionally considered as a diagnostic criterion standard, it is not carried out in all centres and has many limitations. It is costly, painful, and invasive procedure associated with sampling errors and potential complications. Also, it only examines a very small portion, which does not exceed 1/50,000 of the volume of the examined organ with intra- and inter-observer variability. These limitations reduce the relevance of liver biopsy and yield an urge for a non-invasive efficient tool [10, 18].
Recently, MRE technique, which estimates hepatic stiffness even in absence of fibrosis, is successfully employed as a non-invasive diagnostic tool. It is an optimal procedure for evaluation of liver parenchyma in adults LLDs prior to donation surgery [16, 19].
The study in hand was conducted on 37 consecutive eligible healthy LLDs candidates, whose suitability for liver donation was assessed on the basis of their livers’ stiffness measurements estimated by MRE. They were 28 (75.68%) males and 9 (24.32%) females with their ages ranged from 24 to 45 years (34.55 ± 9.45 years) and their BMI ranged from 17.55 to 50.60 kg/m2 (34.05 ± 8.14 kg/m2).
Based on the hepatic MRE findings, which were confirmed by the results of liver biopsy that obtained from the same area evaluated by the MRE, we found that most of the study participants were candidates with absolutely normal hepatic tissue (26/37; 70.27%); most of them were males (19/26; 73.08%), aged less than 35 years (23/26; 88.46%) and had BMI less than 25 kg/m2 (24/26; 92.31%). Additionally, we found 11 (29.73%) candidates with abnormal hepatic tissues; most of them were males (9/11; 81.82%) and aged ≥ 35 years (7/11), while near all of them (10/11; 90.91%) had body BMI ≥ 25 kg/m2. Moreover, our results revealed significant statistical differences between LLDs with normal and abnormal hepatic tissues regarding age, gender, and BMI (P < 0.003, P < 0.02, and P < 0.001, respectively). In a parallel manner, Gallegos-Orozco et al. [16] reported that 10 out of 11 (90.91%) LLDs with abnormal liver biopsy results were males with significantly higher BMI > 25 kg/m2 than that of candidates with normal liver biopsy results (P = 0.02). On the other hand, Yoon et al. [3] found that the BMI did not significantly differ between LLDs with normal hepatic biopsy results and those with simple steatosis. However, they observed that LLDs with normal hepatic biopsy results had significantly lower BMI than those with abnormal liver biopsy due to fibrosis or steatosis with inflammatory activity (P = 0.013 and P = 0.0001, respectively).
Noteworthy, we observed that the liver stiffness values were not significantly affected by age nor gender of the studied candidates (P = 0.0687 and P = 0.60; respectively). This is in agreement with Lee et al. [12] who found a non-significant difference in the values of liver stiffness neither between genders nor among different age groups (P > 0.001).
In harmony with the results obtained by Gallegos-Orozco et al. [16], we observed that the liver stiffness in candidates with BMI ≥ 25 kg/m2 was significantly higher than those with BMI < 25 kg/m2 (P < 0.001). On the contrary, Yoon et al. [3] observed a non-significant difference in BMI between donors with normal hepatic tissue and those with simple steatosis (P > 0.05), while they concluded that LLDs with normal hepatic tissue and average measurements of liver stiffness had BMI significantly lower than that in candidates with abnormal hepatic tissue of non-alcoholic fatty liver diseases including steatosis with inflammatory activity.
Quantitative evaluation of the potential LLDs for coexistence of hepatic steatosis, which influences the hepatic functional recovery, is crucial [20]. Moreover, hepatic fibrosis is not a homogenous process; generating the potential for sampling error in biopsy-based diagnosis. Noteworthy, the presence of liver fibrosis is usually associated with elevated hepatic parenchymal stiffness. However, increased liver stiffness is not necessarily indicating the presence of fibrosis [15].
In the current study, we correlated the liver stiffness values and the histopathological results of liver biopsy. A highly significant correlation was observed between the MRE values and liver biopsy results (P < 0.0003). The previous studies recorded the average values of liver stiffness in normal LLDs candidates to be ranged from 1.54 to 2.87 kPa with the mean liver stiffness measurements to be ranged from 2.052 to 2.44 kPa [12, 15, 16, 19], while, in the current study, the LLDs candidates with absolutely normal hepatic tissue yielded liver stiffness values ranged from 0.74 to 2.20 with the mean stiffness value of 1.72 ± 0.30 kPa [15, 21]. Furthermore, we compared the liver stiffness values between normal and abnormal hepatic tissues, the grades of steatosis to each other, METAVIR stages of fibrosis to each other, as well as steatosis with fibrosis. Intriguingly, our results revealed statistically significant differences in all comparisons (P < 0.05). Moreover, our results demonstrated that the MRE liver stiffness measurements in LLDs with absolutely normal hepatic parenchyma was significantly lower than those with abnormal hepatic tissue (P = 0.0001). Additionally, we noted that the increase in liver stiffness is highly significant between S1a and F2 (P < 0.001), S1b and F1 (P < 0.002), as well as S1b and F2 (with P < 0.001) much more than between S1a and S1b (P = 0.045), F1 and F2 (P = 0.016), as well as S1a and F1 (P = 0.026).
In accordance with our results, Gallegos-Orozco et al. [16] reported a significant increase in the liver stiffness in LLDs with hepatic steatosis ≥ 20% more than in candidates with hepatic steatosis < 20% (P < 0.0001). Additionally, Yoon et al. [3] concluded that liver stiffness measurements in LLDs with normal hepatic tissue was significantly lower than those with abnormal hepatic tissue due to existence of fibrosis (P = 0.0001). Also, they observed that the liver stiffness value in candidates with liver fibrosis was significantly higher than liver stiffness in candidates with simple steatosis (P = 0.001). However, they found non-significant difference in the values of liver stiffness between donors with hepatic fibrosis, as well as those with non-alcoholic steato-hepatitis and steatosis with inflammatory activity (P = 0.812 and P = 0.204, respectively). On the other hand, Yin et al. [22] reported non-significant differences in the liver stiffness values on comparing between F0 and F1, between F1 and F2, as well as between F0 and F2 stages of fibrosis.
The study in hand proposed a cut-off value of ≥ 2.24 kPa with 0.992 AUC to distinguish between absolutely normal hepatic tissue and abnormal hepatic tissue with steatosis and/or fibrosis with highest specificity, sensitivity and accuracy (100%, 98.65%, and 99.24%, respectively). On the other hand, Gallegos-Orozco et al. [16] proposed 2.6 kPa as an optimal cut-off value for discrimination between normal and abnormal hepatic tissues in LLDs candidates with AUC of 0.81, 0.72% sensitivity, and 0.85% specificity.
Interestingly, by using liver stiffness measurements estimated by means of MRE in the studied LLDs candidates, we accurately discriminated completely normal hepatic tissue from mild steatosis with detection of mild steatosis of grade ≥ S1 (with fat contents ≥ 5%) via using a cut-off value of ≥ 2.35 kPa with 0.981 AUC (100% specificity, 98.10% accuracy, and 96.83% sensitivity), while by utilizing a cut-off value ≥ 2.38 kPa with 0.984 AUC, we accurately discriminated non-substantial hepatic steatosis with fat contents < 20% from substantial steatosis with fat contents ≥ 20% with 100% specificity, 98.44% accuracy, and 96.90% sensitivity. On contrary, Gallegos-Orozco et al. [16] reported 2.82 kPa as an optimal cut-off value for identification of substantial hepatic steatosis of ≥ 20% with 88% sensitivity and 100% specificity.
Relied upon the liver stiffness measurements, the previous studies [11, 15, 23] reported cut-off values ranged between 2.4 and 2.93 kPa with sensitivity 98% and specificity 99% for detection of hepatic fibrosis. In the present study, to detect mild hepatic fibrosis, we suggested a cut-off value ≥ 2.42 kPa, with 0.990 AUC, 100% specificity, 99% accuracy, and 97.51% sensitivity, for discrimination between completely normal hepatic tissue and mild fibrosis of ≥ F1 stage METAVIR score of fibrosis. Additionally, we proposed a cut-off value ≥ 2.57 kPa for discrimination between normal and non-significant hepatic fibrosis of F1 stage of METAVIR score and significant substantial hepatic fibrosis ≥ F2 stages of fibrosis with 0.988 AUC, 100% specificity, 98.80% accuracy, and 97.22% sensitivity. In contrast, Kim et al. [23], distinguished significant substantial liver fibrosis (≥ F2) from normal or mild fibrosis (F0–1) by using 3.05 kPa as an optimal cut-off value with 89.7% sensitivity and 87.1% specificity, while by using the same cut-off value (3.05 kPa), the results of Yin et al. [24] yielded 86% sensitivity and 85% specificity.
These variations in the cut-off values of liver stiffness measurements in LLDs candidates among different studies, including the current study, might be attributed to differences in the study design, selection criteria, and technical variations including dissimilarities between MRI systems, the used scanning parameters, and methods of interpretation, in addition to differences in the used statistical methods.
To the best of our knowledge, in our area, this is the first study to highlight the diagnostic performance of MRE as a pre-transplant non-invasive screening imaging modality for selection and validation of LLDs who can participate in the donation surgery. Furthermore, very limited researches emphasized the diagnostic utility of using liver stiffness values estimated by means of MRE technique with most of them were limited by their retrospective design and errors in the liver biopsy as a result of heterogeneity of the hepatic fibrosis process. We did our best to overcome the limitations of the previous studies, so the study in hand was designed to be a prospective observational study and in each study participant, we used the confidence image to measure liver stiffness and to obtain liver biopsy. Moreover, we tried to assume optimal cut-off values for detection of hepatic steatosis, in addition to differentiation between normal or non-significant steatosis (with fat contents < 20%) and substantial steatosis (with fat contents ≥ 20%). Also, we proposed optimal cut-off values for detection of non-significant mild hepatic fibrosis of stage ≥ F1 and for discrimination between normal or non-significant fibrosis and significant advanced stage of fibrosis (≥ F2).
Limitations
Although we thought that our prospective study might afford a beneficial focused idea about the MRE technique and illuminated its diagnostic reliability as a trustworthy non-invasive screening tool of LLDs candidates, which advocated for MRE to be an alternative screening technique to the invasive liver biopsy, our prospective observational study faced some difficulties. First limitation was the small number of the study population. Therefore, further extended studies on a larger number of subjects with expanded margins of inclusion criteria should be performed to establish the best possible diagnostic values. Second limitation was lack of studying other morbid conditions that might influence the hepatic visco-elasticity such as iron overload as the majority of the study candidates were having normal hepatic tissue and BMI. However, this limitation was beneficial to us for recognizing the normal values of liver stiffness by means of MRE as it was the first study in our area that considered and illustrated the reliability of such technique.
Conclusion
In conclusion, MRE technique is a state of art. It can be considered as a promising reliable efficient non-invasive pre-transplant screening technique that has the potential to alternate the invasive liver biopsy technique in selection and validation of LLDs candidates for LDLT surgery. Additionally, based on liver stiffness measurements yielded by MRE in LLDs candidates, we accurately discriminated between completely normal and abnormal hepatic tissue, mild non-significant hepatic steatosis and substantial hepatic steatosis (< 20% versus ≥ 20%), as well as mild non-significant fibrosis and substantial advanced fibrosis (≥ F2).
Availability of data and materials
The authors confirm that all data supporting the findings of the current study are available within the article. Also, all the data sets used and/or analyzed during the current study are available from the corresponding author on a reasonable request.
Abbreviations
- kPa:
-
Kilo Pascal
- LDLT:
-
Living donor liver transplantation
- LLDs:
-
living liver donors
- MRE:
-
Magnetic resonance elastography
References
Hu T, Silva A, Hu L et al (2010) Utilizing magnetic resonance elastography in the evaluation of liver donors. Proc Intl Soc Mag Reson Med 18:4655
Dorwal P, Gautam D, Sharma D et al (2015) Donor biopsy in living donor liver transplantation: is it still relevant in a developing country? Malaysian J Pathol 37(1):39–43
Yoon JH, Lee JM, Suh KS et al (2015) Combined use of MR fat quantification and MR elastography in living liver donors: Can it reduce the need for preoperative liver biopsy? Radiology 276(2):453–464
Dowman JK, Tomlinson JW, Newsome PN (2011) Systematic review: the diagnosis and staging of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis. Aliment Pharmacol Ther 33:525–540
Sumida Y, Nakajima A, Itoh Y (2014) Limitations of liver biopsy and non-invasive diagnostic tests for the diagnosis of non-alcoholic fatty liver disease/non-alcoholic steato-hepatitis. World J Gastroenterol 20:475–485
Kim BH, Lee JM, Lee YJ et al (2011) MR Elastography for non-invasive assessment of hepatic fibrosis: Experience from a tertiary center in Asia. J Magn Reson Imaging 34:1110–1116
Myers RP, Fong A, Shaheen AA (2008) Utilization rates, complications and costs of percutaneous liver biopsy: a population-based study including 4275 biopsies. Liver Int 28:705–712
Lupsor M, Badea R, Stefanescu H et al (2009) Performance of a new elastographic method (ARFI technology) compared to uni-dimensional transient elastography in the noninvasive assessment of chronic hepatitis C. Preliminary results. J Gastrointestin Liver Dis 18:303–310
Cho SH, Lee JY, Han JK et al (2010) Acoustic radiation force impulse elastography for the evaluation of focal solid hepatic lesions: preliminary findings. Ultrasound Med Biol 36:202–208
Stoopen-Romettia M, Encinas-Escobar ER, Ramirez-Carmona CR et al (2017) Diagnosis and quantification of fibrosis, steatosis, and hepatic siderosis through multi-parametric magnetic resonance imaging. Rev Gastroenterol Mex 82(1):32–45
Huwart L, Sempoux C, Vicaut E et al (2008) Magnetic resonance elastography for the non-invasive staging of liver fibrosis. Gastroenterology 135:32–40
Lee DH, Lee JM, Han JK et al (2013) MR elastography of healthy liver parenchyma: Normal value and reliability of the liver stiffness value measurement. J Magn Reson Imaging 38:1215–1223
Yoon JH, Lee JM, Woo HS et al (2013) Staging of hepatic fibrosis: Comparison of magnetic resonance elastography and shear wave elastography in the same individuals. Korean J Radiol 14(2):202–212
Shin M, Song S, Kim JM et al (2012) Donor morbidity including biliary complications in living-donor liver transplantation: single-center analysis of 827 cases. Transplantation 93:942–948
Venkatesh SK, Yin M, Ehman RL (2013) Magnetic resonance elastography of liver: Technique, analysis, and clinical applications. J Magn Reson Imaging 37:544–555
Gallegos-Orozco JF, Silva AC, Batheja MJ et al (2015) Magnetic resonance elastography can discriminate normal vs. abnormal liver biopsy in candidates for live liver donation. Abdom Imaging 40:795–802
Wu WP, Chou CT, Chen RC et al (2015) Non-invasive evaluation of hepatic fibrosis: the diagnostic performance of magnetic resonance elastography in patients with viral hepatitis B or C. PLoS ONE 10(10):e0140068. https://doi.org/10.1371/journal.pone.0140068
Poynard T, Lenaour G, Vaillant JC et al (2012) Liver biopsy analysis has a low level of performance for diagnosis of intermediate stages of fibrosis. Clin Gastroenterol Hepatol 10:657–663
Talwalkar JA, Yin M, Fidler JL et al (2008) Magnetic resonance imaging of hepatic fibrosis: Emerging clinical applications. Hepatology 47(1):332–342
Perez-Daga JA, Santoyo J, Suárez MA et al (2006) Influence of degree of hepatic steatosis on graft function and postoperative complications of liver transplantation. Transplant Proc 38:2468–2470
Rouviere O, Yin M, Dresner MA et al (2006) MR elastography of the liver: preliminary results. Radiology 240:440–448
Yin M, Glaser KJ, Talwalkar JA et al (2016) Hepatic MR elastography: Clinical performance in a series of 1377 consecutive examinations. Radiology 278(1):114–124
Kim D, Kim WR, Talwalkar JA et al (2013) Advanced fibrosis in non-alcoholic liver disease: Non-invasive assessment with MRelastography. Radiology 268:411–419
Yin M, Talwalkar JA, Glaser KJ et al (2007) Assessment of hepatic fibrosis with magnetic resonance elastography. Clin Gastroenterol Hepatol 5:1207–1213
Acknowledgements
None.
Funding
The authors declare that the current study had no funding from any resource.
Author information
Authors and Affiliations
Contributions
REM (the corresponding author) suggested the research idea, the study design, collected data in all stages of manuscript, ensured the original figures and data in the work, correlated the clinical data of the studied patients and matched it with the imaging findings, with significant contribution to design the methodology, statistical data analysis, as well as, prepared, drafted, and revised the manuscript. MAA shared in sample collection, correlated the clinical data of patients, and matched them with the radiological findings. HMO shared in sample collection. HEMS shared in the clinical evaluation of the study participants. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The current study was approved by the Ethical Research Committee (ERC) of Tanta University, Faculty of Medicine, and an official permission to carry out the present study (Approval Code: 33959/7/20) was obtained from the responsible authorities. All procedures performed in the current study, involving human participants, were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. Additionally, all potential hazards were explained to the participants and their families with all participants gave their written informed consent before the start of the study. For unconscious patient or patient with decreased conscious level, written informed consent was obtained by their legal guardian before the start of the study.
Consent for publication
All subjects included in the current research gave their written informed consent to publish the data contained within the study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mohamed, R.Eed., Amin, M.A., Omar, H.M. et al. Hepatic magnetic resonance elastography: can it be an alternative to invasive biopsy preceding living donor liver transplantation?. Egypt J Radiol Nucl Med 51, 206 (2020). https://doi.org/10.1186/s43055-020-00324-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-020-00324-w