Abstract
Background
Gastrointestinal stromal tumours (GISTs) account for most mesenchymal gastrointestinal tumours, which in turn represent 1% of all gastrointestinal cancers. They mainly affect older adults, with a slight male preponderance. These lesions can be found along the digestive tract and most frequently in the stomach. Extragastrointestinal stromal tumours (EGISTs) are even rarer lesions, with few cases or series reported.
Case presentation
A 51-year-old woman was referred to our hospital due to progressive abdominal volume increase. Evaluation by multidetector computed tomography (MDCT) revealed a large intraperitoneal mixed tumour with few solid components, measuring up to 30 cm and compressing the surrounding structures, thought to be an ovarian tumour. Diagnostic laparotomy showed that the lesion was adherent to the greater gastric curvature and the vesical peritoneum. The lesion was removed without complications.
Conclusions
Imaging plays an essential role in the diagnosis of large intraperitoneal tumours. MDCT is the preferred technique to stage and to follow-up EGISTs.
Similar content being viewed by others
Background
Gastrointestinal stromal tumours (GISTs) are the most common non-epithelial gastric neoplasms and the most frequent mesenchymal tumour to affect the digestive tract [1,2,3,4]. These tumours are believed to arise from precursors of the interstitial cells of Cajal, regarded as the gastrointestinal “pacemaker” [5]. They can regulate gastrointestinal peristalsis providing autonomic innervation to the smooth muscle of the bowel wall through the myenteric plexus [6, 7]. Extragastrointestinal stromal tumours (EGISTs) are GISTs that are found outside the digestive tract, and only a few cases have been reported [8,9,10,11]. Approximately 95% of GISTs overexpress KIT (CD117), the immunohistochemistry signature of GISTs which is a receptor protein tyrosine kinase. However, only 80% of GISTs have KIT gene mutations that lead to gain of function of the KIT receptor [2]. Other biomarkers can be overexpressed, such as platelet-derived growth factor receptor alpha (PDGFRA).
Contrast-enhanced abdominal and pelvic multidetector computed tomography (MDCT) is the preferred imaging technique regarding staging, follow-up and assessment of tyrosine kinase inhibitors’ (TKI) immunotherapy responses [12, 13]. The MDCT protocol should include neutral oral contrast with the acquisition of a triphasic MDCT. The arterial phase is crucial to evaluate hepatic involvement since GISTs are hypervascular lesions, and some may not be visible in the portal venous phase [7].
Case presentation
We report the case of a 51-year-old woman referenced to our hospital with complaints of slowly enlarging abdominal volume for over a year. The patient also reported increased bowel movements in the weeks before the admission. She denied additional symptoms, including surfeit, pain, vomiting and dyspnoea. Clinical examination revealed a mobile abdominal and pelvic tumour, palpable up to 3 cm below the xiphoid process.
The patient did not have adequate gynaecological surveillance and took oral contraceptives for several years until the previous 7 months. There was no significant personal nor familial history reported. The laboratory results presented as follows: CA-125, 118 U/mL; CEA < 0.5 ng/mL; and CA 19-9, 6 U/mL.
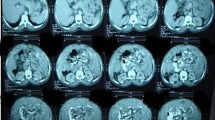
A pre- and post-contrast abdominal and pelvic MDCT on portal venous phase reported a large intraperitoneal mixed tumour with few solid components (Figs. 1, 2, 3, 4, 5, 6 and 7), mostly located in the upper abdomen (Figs. 2, 3 and 4). It measured up to 30 × 12 × 26 cm in longitudinal, anteroposterior and transversal axes, respectively. The tumour compressed the surrounding structures, particularly the kidneys and the small bowel, the latter located predominantly in the upper left abdominal quadrant (Figs. 2 and 3). Despite these findings, no dilatation of the urinary tract nor the digestive tract was noted. The vascular pedicle of the lesion was not accurately identified, although several enlarged vessels could be seen converging to the superior mesenteric vein and the vesical peritoneum (Figs. 2, 3, 5, 6 and 7).
Axial post-contrast MDCT image at the level of the upper abdomen, depicting the enlarged vessels (red arrows) converging to the superior mesenteric vein. Note all the surrounding structures (particularly the kidneys and the jejunum) compressed by the tumour (yellow arrows). Some intraperitoneal fluid (A) is also seen
Axial post-contrast MDCT image at the level of pelvis. Many small vessels are also depicted in the anterior reflection of the pelvic peritoneum (light blue arrow), which may indicate another vascular source from the tumour (yellow arrows). The uterus (U) is well delimitated from the tumour, and some ascitic fluid (A) is also seen
Even though the origin of this tumour was not clear, the most probable differential diagnoses included an ovarian neoplasm and an intraperitoneal desmoid. An ovarian tumour was the most likely diagnosis given the demographics and the morphological features, although the serum tumoral marker (CEA) was not elevated. Desmoid tumours are rare benign neoplasms most frequently found in women. They are well-circumscribed and enhancing masses that may be found in the mesentery, but are usually more homogeneous and predominantly solid.
The patient underwent subsequent diagnostic laparotomy, whose operative data reported a cystic and lobulated tumour with 30 cm. It was adherent to the greater curvature of the stomach and the vesical peritoneum. There were no abnormalities involving the uterus and the ovaries.
The intraoperative pathological evaluation reported a fusocellular tumour with no cytological features of malignancy. The final pathological assessment depicted a gastrointestinal stromal tumour (GIST) with extragastrointestinal location (presumably peritoneal), of mixed subtype.
Discussion
GISTs are a rare entity, responsible for 1% of primary gastrointestinal cancers [3, 8]. These lesions are slightly more prevalent in males, with a median age at diagnosis of 60–65 years, despite the wide range [13]. They can occur anywhere along the gastrointestinal tract, with the stomach being the most common site (60–70% of cases), followed by the small intestine and rarely elsewhere in the abdomen [1, 3]. Nevertheless, some cases with extraintestinal sites (EGISTs) and small case series have been reported, such as the case we are presenting [2, 5, 10, 11].
Most of the diagnoses are incidental, resulting from imaging assays or endoscopic evaluations performed for non-related reasons. The clinical staging most frequently relies on MDCT evaluation, using the TNM classification. It includes tumour size and location, lymph node, distant spreading and mitotic rate [13]. These are considered prognostic factors along with histological type and depth of invasion. The mitotic rate represents the most independent prognostic factor for GIST recurrence after surgery [7, 13]. All these factors contribute to a risk stratification that is well established—our patient’s GIST presented high-risk features. Large intraperitoneal lesions may pose substantial difficulties in identifying their origin. In our case, it led initially to a different diagnosis.
Our patient’s symptoms were caused by massive tumour volume and by bowel compression—a rare presentation related to GISTs. GISTs are more frequently associated with occult gastrointestinal bleeding (often resulting from pressure necrosis and consequent ulceration of the mucosa, which may even cause haematemesis or melena), early satiety, anorexia, nausea and vomiting [3, 7].
Surgery provided the definitive treatment, which intended to remove the lesion with preserved pseudocapsule and negative microscopic margins. Targeted therapy (tyrosine kinase inhibitors) also plays an essential role, not only for neoadjuvant purposes but also as an adjuvant treatment in high-risk patients, such as our example.
The patient was asymptomatic in the last medical appointment. Nevertheless, and against the recommendations, she refused the treatment with tyrosine kinase inhibitors due to their putative side effects.
Conclusions
In patients with large intraperitoneal tumours, cross-sectional imaging evaluation is essential to characterise the lesion. In these cases, MDCT may give presumptive diagnoses, although one should always consider other rare entities with unique clinical presentations.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CD:
-
Cluster of differentiation
- CEA:
-
Carcinoembryonic antigen
- EGIST:
-
Extragastrointestinal stromal tumour
- GIST:
-
Gastrointestinal stromal tumour
- MDCT:
-
Multidetector computed tomography
- TKI:
-
Tyrosine kinase inhibitors
References
Fülöp E, Marcu S, Milutin D, Borda A (2008) Gastrointestinal stromal tumors: review on morphology, diagnosis and management. Rom. J. Morphol. Embryol. 50:319–326
Miettinen M, Lasota J (2001) Gastrointestinal stromal tumors--definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch 438:1–12
Kang HC, Menias CO, Gaballah AH et al (2013) Beyond the GIST: mesenchymal tumors of the stomach. RadioGraphics 33:1673–1690. https://doi.org/10.1148/rg.336135507
Miyahira CK, Bonfitto M, Farto JF de L, et al (2018) Extragastrointestinal stromal tumor: a differential diagnosis of compressive upper abdominal tumor. Case Rep Surg 2018:. https://doi.org/10.1155/2018/1052960
Sasmal PK, Sharma R, Patra S et al (2019) Malignant extra-gastrointestinal stromal tumor of the mesentery. Surg J 05:e65–e68. https://doi.org/10.1055/s-0039-1693040
Fletcher CDM, Berman JJ, Corless C et al (2002) Diagnosis of gastrointestinal stromal tumors: a consensus approach. Int J Surg Pathol 10:81–89. https://doi.org/10.1177/106689690201000201
Joensuu H, Hohenberger P, Corless CL (2010) Gastrointestinal stromal tumor. Mod Soft Tissue Pathol Tumors Non-Neoplastic Cond 382:491–507. https://doi.org/10.1017/CBO9780511781049.018
Miettinen M, Lasota J (2001) Gastrointestinal stromal tumors - definition, clinical, histological, immunohistochemical, and molecular genetic features and differential diagnosis. Virchows Arch 438:1–12. https://doi.org/10.1007/s004280000338
Ashoor AA, Barefah G (2020) Unusual presentation of a large GIST in an extraintestinal site: a challenging diagnosis dilemma. BMJ Case Rep. https://doi.org/10.1136/bcr-2019-229839
Reith JD, Goldblum JR, Lyles RH, Weiss SW (2000) Extragastrointestinal (soft tissue) stromal tumors: an analysis of 48 cases with emphasis on histologic predictors of outcome. Mod Pathol 13:577–585. https://doi.org/10.1038/modpathol.3880099
Hatipoğlu E (2018) Extragastrointestinal stromal tumor (EGIST): a 16-year experience of 13 cases diagnosed at a single center. Med Sci Monit 24:3301–3306. https://doi.org/10.12659/MSM.907654
Hong X, Choi H, Loyer EM et al (2006) Gastrointestinal stromal tumor: role of CT in diagnosis and in response evaluation and surveillance after treatment with imatinib. RadioGraphics 26:481–495. https://doi.org/10.1148/rg.262055097
Guidelines CP (2014) Gastrointestinal stromal tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 25:iii21–iii26. https://doi.org/10.1093/annonc/mdy095
Acknowledgements
Not applicable
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
POS wrote and edited the manuscript. MML was responsible for the pathological assessment. TMC made the critical revision of the manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was approved on 23 January 2020 by the ethical board of the Institution in which it was performed—Instituto Português de Oncologia de Lisboa Francisco Gentil (Lisbon, Portugal). The ethical committee did not present any reference number in the final appreciation that was sent by institutional email.
The patient included in this study gave written informed consent.
Consent for publication
The patient had signed written informed consent for research purposes, including the clinical details and the included images.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oliveira Santos, P., Cunha, T.M. & Lemos, M.M. An unusual presentation of an extragastrointestinal stromal tumour: a case report. Egypt J Radiol Nucl Med 51, 162 (2020). https://doi.org/10.1186/s43055-020-00297-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-020-00297-w