Abstract
Background
Fish bones are the most common cause of accidental foreign body ingestion, especially in Asian and Mediterranean nations. In most cases, the fish bones pass through the alimentary tract without any complications and rarely require any intervention. Less than 5% of the patients with accidentally ingested fish bones develop complications. In this report, we present the first documented case of a fish bone induced bronchial artery pseudoaneurysm in an elderly male with underlying bronchiectasis; the latter recognized as a risk factor for developing bronchial artery hypertrophy.
Case presentation
We report a case of a fish bone induced bronchial artery pseudoaneurysm in a patient with underlying bronchiectasis. The vascular complication induced by the fish bone was identified only on intravenous contrast CT and would not have been identified on plain CT alone. The patient underwent bronchial artery embolization, following which the fish bone was dis-impacted endoscopically.
Conclusions
Intravenous post contrast chest CT may have an important role in the evaluation of accidental fish bone ingestion, especially in patients with underlying lung diseases, as vascular complications are most often overt on a non-contrast CT study.
Similar content being viewed by others
Background
Foreign body ingestion is a common clinical presentation in the emergency room (ER), and fish bones account for 84% of the accidentally ingested foreign bodies. A majority of the ingested fish bones pass out from the gastrointestinal tract (GIT) without any symptoms or the need for an intervention, and < 1% of the patients develop complications. Symptoms when present are non-specific [1] and include nausea/vomiting, drooling, dysphagia, and retrosternal or chest pain. Fish bones impacted for long durations can lead to potentially life-threatening complications such as esophageal perforation, mediastinal or neck abscess, and vascular or lung injuries [2]. Here, we report the first documented case of fish bone induced bronchial artery pseudoaneurysm in a patient with underlying bronchiectasis. We feel our article carries an important message to a multitude of specialists including ER physicians, gastroenterologists, cardiothoracic surgeons, as well as radiologists, who may come across such a similar situation in the future.
Case presentation
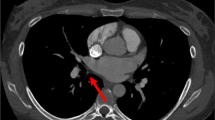
We present a case of a 61-year-old male with bronchiectasis and systemic hypertension on medication who presented to our hospital with complaints of retrosternal chest pain following accidental fish bone ingestion for 5 days. Two days earlier, he was evaluated at a local hospital for the same symptoms where he underwent a non-contrast CT of the neck and chest, which revealed the fish bone in the thoracic esophagus at the level of the bifurcation of the trachea and was advised emergency endoscopy for foreign body retrieval; however, the patient refused the procedure, and 2 days later presented to our hospital. As the previous CT images were not available for evaluation, a repeat non-contrast CT of the chest was done, which revealed cystic bronchiectasis in both lungs (Fig. 1) and a 20-mm long and 2-mm thick hyperdense fish bone (Fig. 2a, b) partly located in the lumen of the thoracic esophagus close to the level of the bifurcation of the trachea. More than 95% of the fish bone had penetrated the posterior wall of the esophagus and was now located retroesophageal. A contrast enhanced CT (CECT) study of the chest was performed following consultation with a multi-disciplinary team involving gastroenterology, gastrosurgery, and cardio-thoracic surgery. To our surprise, CECT (Fig. 3a, b) of the chest revealed a bronchial artery pseudoaneurysm (measuring 9.5 × 5.6 × 6.6 mm), seen arising from a hypertrophied right bronchial artery at ~ 5.8 mm from its origin protruding anteriorly and in intimate contact with the fish bone. We presume that the bronchial artery pseudoaneurysm must have resulted from the fish bone penetrating a hypertrophied bronchial artery; the latter being a recognized complication of long-standing bronchiectasis, although a pre-existing bronchial arterial pseudoaneurysm cannot be completely ruled out (as the patient had no prior chest CT images or reports for comparison). No active extravasation of intravenous contrast was seen on the post contrast images. As the consulting gastroenterologists and cardiothoracic surgeons felt that any attempt at removing the fish bone, either endoscopically or surgically could lead to potential life-threatening hemorrhage; an urgent interventional radiology consultation was taken prior to endoscopy, and bronchial artery embolization was done (Fig. 4). In the intensive care setting, an upper gastrointestinal endoscopy was done, and dis-impaction of the fish bone was carried out successfully. A cardiothoracic surgery consultation was done, and the patient was counselled regarding the possible need for surgery as well an endoscopic ultrasound evaluation. However, the patient refused further hospital admission and was discharged against medical advice.
Discussion
Accidental ingestion of fish bones is a common ER presentation especially across Asia and the Mediterranean where the ingestion of unfilleted fish occurs regularly [3, 4]. Fish bones when impacted in the esophagus are a medical emergency. In close to 80% of the cases, the fish bone gets expelled from the GIT, but about 10–20% will require an intervention such as an endoscopic removal, and nearly 4% of these cases can present with an esophageal perforation. An esophageal perforation can be further complicated by mediastinal infection, vascular injuries such as pseudoaneurysm or aorto-esophageal fistula, tracheo-esophageal fistula, pneumomediastinum, pneumothorax, pericarditis, and other conditions. In rare cases, a fish bone can also migrate to adjacent structures such as the thyroid and cause complications [5]. Vessels that have been documented in fish bone induced injuries are the aorta, subclavian artery, internal carotid artery, and the internal jugular vein. A fish bone can either injure the vessel wall either by secondary or direct puncture or from an adjacent inflammatory reaction leading to vascular rupture contained by adjacent soft tissue structures and inflammatory exudate (pseudoaneurysm). In most cases, the site of esophageal perforation is sealed off by a hematoma or a blood clot, leading to partial tamponade and prevention of further bleeding [5]. In adults, the most common site of fish bone impaction is the oropharynx/hypopharynx, followed by the oral cavity and the esophagus. Within the oropharynx, the most common sites include the tonsils, followed by the base of the tongue, vallecula, and the pyriform sinus. In the esophagus, a fish bone commonly gets impacted at the 3 sites of physiological narrowing, namely, the cricopharyngeal muscle at the level of C5/C6, at the level of the aortic arch and left mainstem bronchus, and the gastroesophageal junction near the diaphragm. Esophageal fish foreign bodies are usually seen in adults > 40 years of age and mostly attributed to weakening of the swallowing mechanism [1, 6].
Fish bones are often difficult to identify on a plain radiograph, with the majority appearing radiolucent. The reported sensitivity of a plain radiograph in identifying a fish bone is as low as 32%, with a false negative rate of 47% [6]. Therefore, a negative soft tissue radiograph does not exclude a fish bone foreign body [1, 6]. Multidetector computed tomography (MDCT) is the preferred imaging modality for evaluating patients with accidentally ingested foreign bodies, with a reported sensitivity and specificity of 90–100% and 93.7–100%, respectively [7]. Potential mimickers of foreign bodies in the neck on MDCT include tonsilloliths, hyoid bone, cricoid calcifications, and motion artifacts. Additional pitfalls include artifacts from radiodense materials, e.g., barium or silver nitrate or even fecal material in the bowel [1, 7] and slice thickness [8]. Some experts believe the use of contrast [oral/intravenous (i.v)] can hamper the identification of fish bones on MDCT. Oral contrast can conceal fish bones in the intestinal lumen, while extraluminal fish bones can mimic blood vessels on i.v contrast studies [8]. If there is a strong clinical suspicion for accidental fish bone ingestion and if the initial study is an i.v contrast examination that was negative, then the study needs to be reperformed without contrast. Factors that can improve their detection on MDCT include the use of thinner reconstructions (3 mm/1.5 mm) as well as using multiplanar reformatted images for evaluation [8]. We recommend i.v contrast MDCT studies in all patients with suspected foreign body ingestion who have underlying lung disease as in our case, to rule out unsuspected complications.
As per the American Society of Gastrointestinal Endoscopy, an impacted fish bone is considered an emergency that requires immediate removal [9]. If the fish bone is directly visible, it can be removed by forceps. However, a fibreoptic/rigid endoscopic retrieval will be required in those cases where the fish bone is located beyond the level of direct visualization [10]. Surgical intervention is generally reserved for those cases with perforation or for complications that cannot be resolved endoscopically or following several unsuccessful endoscopic retrieval attempts [10].
Conclusion
Although oral or i.v contrast is generally not recommended for assessing patients with accidentally ingested fish bones, we recommend an i.v contrast CT study in all patients with underlying lung diseases who present to the ER with complaints of foreign body ingestion, as vascular complications are most often overt on a non-contrast CT study.
Availability of data and materials
All data is available based on a reasonable request.
Abbreviations
- CT scan:
-
Computed tomography scan
- CECT:
-
Contrast enhanced computed tomography
- ER:
-
Emergency room
- GIT:
-
Gastrointestinal tract
- i.v:
-
Intravenous
- MDCT:
-
Multidetector computed tomography
References
Venkatesh SH, Venkatanarasimha Karaddi NK (2016) CT findings of accidental fish bone ingestion and its complications. Diagn Interv Radiol. 22(2):156–160
Wang A, Zhou Y, Huang Q (2019) A fish bone induced aortic arch pseudoaneurysm in a male patient: a case report. Medicine (Baltimore). 98(29):e16486
Dagan E, Yakirevich A, Migirov L, Wolf M (2011) The role of economics and weekend meals in impacted fish bone occurrence in central Israel. Isr Med Assoc J 13(01):48–50
Arulanandam S, Das De S, Kanagalingam J (2015) A prospective study of epidemiological risk factors for ingestion of fish bones in Singapore. Singapore Med J 56(06):329–332 quiz 333
Zuluaga CP, Aluja Jaramillo F, Velásquez Castaño SA, Rivera Bernal AL, Granada JC, Carrillo Bayona JA (2016) Aortic pseudoaneurysm secondary to mediastinitis due to esophageal perforation. Case Rep Radiol. 2016:7982641
Klein A, Ovnat-Tamir S, Marom T, Gluck O, Rabinovics N, Shemesh S (2019) Fish bone foreign body: the role of imaging. Int Arch Otorhinolaryngol. 23(1):110–115
Liew CJ, Poh AC, Tan TY (2013 Aug) Finding nemo: imaging findings, pitfalls, and complications of ingested fish bones in the alimentary canal. Emerg Radiol. 20(4):311–322
Goh BK, Tan YM, Lin SE, Chow PK, Cheah FK, Ooi LL, Wong WK (2006 Sep) CT in the preoperative diagnosis of fish bone perforation of the gastrointestinal tract. AJR Am J Roentgenol. 187(3):710–714
Ikenberry SO, Jue TL, Anderson MA (2011) et al; ASGE Standards of Practice Committee. Management of ingested foreign bodies and food impactions. Gastrointest Endosc 73(06):1085–1091
Ambe P, Weber SA, Schauer M, Knoefel WT (2012) Swallowed foreign bodies in adults. Dtsch Arztebl Int 109(50):869–875
Acknowledgements
None.
Funding
All the authors declare no funding or financial support.
Author information
Authors and Affiliations
Contributions
RPM contributed to the data acquisition, manuscript preparation, and approval of the final version of the study. VJ contributed to the oversight over the case report and manuscript preparation. AT contributed to data acquisition and approval of the final version of the study. MJ contributed to the revision of the manuscript and final edit, interpretation of imaging findings, and approval of the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was approved by the ethical board of the hospital in which the study was performed. The patient reported in this article had signed a written informed consent form. The study did not involve the use of animals. The manuscript has not been submitted to any other journal/site in part or in whole for consideration. It is solely submitted to this journal.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mathew, R.P., Jayaram, V., Toms, A. et al. Fish bone induced bronchial artery pseudoaneurysm in a patient with underlying bronchiectasis—a case report. Egypt J Radiol Nucl Med 51, 128 (2020). https://doi.org/10.1186/s43055-020-00253-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-020-00253-8