Abstract
Background
Pedicle screw instrumentation is used widely in lumbar spine for stabilization to enhance arthrodesis and has been accepted in the thoracic spine in recent years. The purpose of this study was to assess the value of postoperative 320 multi-slice computed tomography (MSCT) in assessment of pedicle screw placement in patients with spinal fixation with clinical and surgical correlation.
Results
A total of 340 pedicular screws were inserted to 70 cases. 286 (84.12%) were in, 54 screws (15.88%) were violated, and revision surgeries were required for 5 displaced screws. On axial, coronal reconstruction and three-dimensional (3D) reformatted CT images 36, 47, and 54 displaced screws were detected, respectively. Both sensitivity and specificity for 3D reformatted images were 100%. For axial image, they were 97.6% and 89.4%, respectively, compared with surgical findings in 5 revised screws.
Conclusion
Multi-slice CT scan is a valuable and valid postoperative assessment tool of accuracy of spinal pedicle screw placement.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Fixation of the spinal pedicles with screws is becoming a broadly used procedure of hardware spinal instrumentation. Though the advancement of surgical technique, instrumentation design, and the use of intraoperative fluoroscopy, puncture of pedicle cortex takes place threatening the nearby neurovascular or extra vertebral structures [1].
The probability of iatrogenic injury must be reduced as the pedicle is surrounded with vital anatomic structures: the dural sac locates medially, the nerve roots locate superiorly and inferiorly, and the vascular structures locate anterolaterally. Additionally, the precision of placement of the pedicle screw is fundamental for the steadiness and efficacy of the surgical process [2].
Transpedicular screw procedure is accompanied with a prevalent series of complications comprising surgery at wrong-level, lesion of nerve root, dural tearing, injury to vascular structures, infections at surgical site, and screw displacement. Displacement of trans pedicular screw proportions fluctuating from 21.1% to 39.8% have been designated in the literatures [3, 4].
Although there are up-to-date procedures, the incident of pedicle screw displacement remains important in lumbar spine fixation [5]. Current challenges in study of pedicle instrumentation have been focused on declining the possibility of pedicle screws displacement [6].
Postoperative imaging is typically done to settle the true sitting and the integrity of instruments, to evaluate the progress of osseous union, to recognize suspected complications (e.g., hematoma or infection), and to discover disease progression or new disease [7]. The main imaging procedure is the conventional radiography. Though, CT is more helpful if there is doubt of breach or misplacement and when a conclusive diagnosis cannot be recognized [8].
The spinal assessment in patients with orthopedic metallic hardware is challenging. Even though the metal artifacts may restrict the efficiency of conventional computed tomography (CT), in the current years, the advancement of multichannel CT has made accessible novel procedures that can aid minimize these artifacts, which also permits quicker scanning times, resulting in reduced motion artifacts with thinner sections, where it is possible to create a scanned volume of isotropic voxels with equivalent image resolution in all planes, and the generation of a higher x-ray tube current may result in decrease of artifacts and better penetration of metal hardware. The acquisition of multi-planar reformatted image in the axial, coronal, sagittal and oblique planes and also three-dimensional volume-rendered images help in optimizing image interpretation [9].
Three-dimensional volume rendering (3D VR) procedures and image reconstruction by multi-planar reformation (MPR) frequently result in higher quality images that are clinically more useful than axial images alone [10].
Aim of the work
The aim of the work was to assess the value of postoperative 320 multi-slice computed tomography in the assessment of pedicle screw placement in patients with spinal fixation with clinical and surgical correlation.
Methods
During the period from January 2017 to June 2018, a cross-sectional study was carried out on 70 patients who were chosen by systemic random sampling technique and underwent spinal fusion surgery using pedicular screws in thoracic and/or lumbosacral spine to assess the value of postoperative 320 multi-slice computed tomography in the assessment of pedicle screw placement in patients with spinal fixation with clinical and surgical correlation. Ages of our patients ranged from 23 to 67 years; 39 (55.7%) of patients were males and 31(44.3%) were females. We excluded patients suffering from congenital and developmental anomalies of the spine, patients with previous surgeries on the involved spinal segments, and those with neurological or medical illnesses causing polyneuropathy and/or myopathy. The study was approved by the ethics committee of our institution. From all participants, written informed consents were taken.
All participants were assessed clinically and radiologically before and after surgery. All surgeries were done at our university hospital by experienced spine and neurosurgeons with the agreement of standardizing the instrumentation procedure. The used implants were made of titanium.
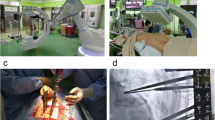
Surgical procedure
All surgeries were carried out under general anesthesia. The involved spinal level was identified by surface anatomical landmarks and radiologically using image intensifier. For all patients, a standard posterior approach was used. The site of screw entrance was recognized by anatomical landmarks pinpointing the joint of the spine of the transverse process with the matching facet.
The freehand method was used. This method depends principally on definite anatomical locations for screws placement. A metal pliable probe is implanted cautiously within the pedicle, continuing through the vertebral body. The four directions walls and floor of the pedicle are probed with the hook palpator. The screw is inserted through this way, and the trajectory of the screw was tested using anteroposterior and lateral projections with an intraoperative image intensifier. Postoperative complete neurological assessment was performed during the first 48 h, to recognize any neurological signs and symptoms like sever back pain, recent radicular symptoms, and neurological deficit.
Imaging assessment
All patients were scanned using 320 MSCT (Toshiba Aquilion One–JAPAN CT Scanner). Image acquisition was achieved in helical mode, in cranio–caudal direction with the patient supine. Imaging sequences comprised of 0.5 mm-thick sections (collimation 128 × 0.62 mm) at 2-mm intervals with a pitch of 0.6 and acquisition parameters of 120–140 kVp and 260–280 MA/s.
Image reconstruction
The raw data were used to reconstruct coronal and sagittal multi-planar reformation (MPR) with a field of view suitable for visualization of the spine. Reconstructions were done in bone and soft tissue windows. To acquire 3D images, a dedicated post processing workstation vitrea was used to get additional image processing as volume rendering (VR). Metal artifacts were cleaned in the reformatted 3D images so the screw was obviously visible and easily assessed.
Image interpretation
The acquired CT images were assessed for the involved level, the inserted screw and the incidence of complications. The screw positions within the pedicle were assessed according to the classification available in the literatures [11,12,13]. Screws were assessed for the following: (1) Errors in insertion relative to the angle of the pedicle. (2) The position inside the pedicle. The screw was stated as as follows: (in) if it was accurately sited inside the pedicle or (out) if it was incorrectly positioned and a portion of it breached through the cortex. Screw displacement was measured in millimeters by the scale on the CT image and categorized according to the distance that the edge of the screw thread extended outside the pedicle cortex and graded. (Grade 0): no apparent violation of the pedicle. (Grade I): <2 mm perforation of the pedicle with one screw thread out of the pedicle. (Grade II): between 2 and 4 mm or perforation of the pedicle with half of the diameter of the screw outside the pedicle. (Grade III): >4 mm or complete perforation of the pedicle [11]. [3] Presence of vertebral or end-plate penetrations. [4] Error in the direction of screw penetration which is named as medial, lateral, cranial or caudal. Correlation between the clinical data and CT findings was done. All patients were followed clinically and radiologically for a period of six months at least to report the incidence of any complications, neurological pain or deficit, and the need for revision surgery.
Statistical analysis
Data were analyzed by using Statistical Package for the Social Sciences (SPSS) version 19. Quantitive data were described as mean and standard deviation (SD). Nominal variables were presented as numbers and percentages. Chi-square test was used for cross tabulation of categorical data. P value ≤0.05 was considered statistically significant.
Results
We studied 70 consecutive patients; of them, 39 were males and 31 were females who experienced spinal surgical fixation, involving thoracic and lumbosacral spinal segments (from T9 to S1), and with a total of 340 inserted screws. The mean age was 48.43 ± 12.32 years with a range of 23 to 67 years. All patients presented with severe pain and/or neurological manifestations.
Degenerative disc herniation was the most common indication for spinal surgical fixation which was presented in 29 cases (41.43%), trauma in 25 cases (35.71%), and spondylolisthesis in 16 cases (22.86%) (Table 1).
The most commonly fixed vertebrae were L4 (82 screws), followed by L5 (74 screws), then L3 (40 screws), and S1 (28 screws). We found that out of a total 340 pedicular inserted screws, 54 screws (15.88%) were misplaced. The dorsal pedicles revealed the highest rate of screw violation as compared with the lumbo-sacral ones in relation to the total number of inserted screws in each region. The frequency of dorsal spine violation was 31.43% (22/70) compared to 11.85% (32/270) in lumbo-sacral region. The spinal levels with the highest incidence of cortical breach were T11 (40%) followed by T9 (30%) (Table 2).
Out of the total 340 inserted screws, 36 (10.59%), 47 (13.82%), and 54 (15.88%) screws were established to be misplaced on axial, coronal reconstruction, and 3D reformatted images, respectively. The frequency of lateral screw violation was more detected than the medial one (Table 3, Figs. 1, 2, and 3). The coronal and 3D reformatted images had the advantage in assessing the screw violation in cranial and caudal directions as well as disc space penetration. End-plate perforation (Figs. 3 and 4) and anterior vertebral encroachment (Figs. 1, 3 and 4) were found in 5 and 11 lateral displaced screws, respectively, and were more recognizable in the reformatted than the axial images.
Internal fixation of L3, L4, and L5 vertebrae with rods and multiple screws. a–c Axial cuts are showing penetration of the anterior and lateral aspects of L4 and L5 vertebrae with two screws and lateral violation of the screw in the right pedicle (grade II). d Coronal reconstruction is showing the lateral location of the screws in L4 and L5 vertebrae. e, f 3D reconstruction sagittal cuts confirm the anterior penetration and lateral location of the screws in L4 and L5 vertebrae and their pedicles
Internal fixation of L4 and L5 vertebrae with plates and multiple screws. a, b Axial cuts are showing lateral violation of the screw in the left pedicle of L4 vertebrae (grade II) and medial deviation of the screw in the right pedicle (grade I). c–e 3D reconstruction sagittal cuts are showing grade I spondylolithesis at L4 and L5, with broken screws at level of L5 vertebra
Internal fixation of L4, L5, and S1 vertebrae with rods and multiple screws. a–c Axial cuts are showing lateral violation of the screw in the left pedicle of L4 vertebra (grade III) and anterior vertebral body penetration of L4, L5, and S1 vertebrae by the right and left screws, and there is widening of the furrow “tunnel” around the screws. d Coronal reconstruction is showing penetration of the upper vertebral end plate of L4 vertebra by the screws. e, f 3D reconstruction sagittal cuts confirm the anterior penetration of the anterior aspects of the vertebrae
a, b Axial cuts are showing penetration of the left screw to the anterior aspect of L4 vertebra and lateral violation of the screw in the left pedicle (grade I). c 3D sagittal reconstruction cut is showing anterior penetration of the L4 vertebra. d Coronal reconstruction is showing penetration of the lower vertebral end plate of S1 vertebra by the left-sided screw
Out of the 54 misplaced screws, lateral violation (Figs. 1, 2, and 3) was seen in 31 screws (57.41%), medial violation (Fig. 2) was present in 11 screws (20.37%), caudal displacement in 7 screws (12.96%), and cranial displacement in 5 screws (9.26%). The remaining 286 screws (84.12%) were correctly inserted (Fig. 5). Regarding the grades of screw displacement, 27 screws were classified as grade I (Fig. 2), 22 were grade II (Figs. 1 and 2), and 5 were grade III violation (Fig. 3).
a Sagittal scout view shows internal fixation of L3, L4, and L5 vertebrae with rods and multiple screws. b Axial cut showing proper position of the screw within the pedicles and in the vertebral bodies. c Coronal reconstruction is showing proper location of the screws within the vertebral bodies and in the pedicles, and disc cages are seen at levels of L4/5 and L5/S1. d 3D sagittal reconstruction image is showing correct placement of screws within the pedicles
Neurological deficits and radicular pain were detected in seven patients (10%). Five screws (1.47%) in three patients (4.29%) needed revision operations while the other four patients relatively improved with conservative treatment. Out of five screws that needed revision, two (40%) were of grade I with medial violation, one screw (20%) was of grade III with lateral violation (also it was broken; Fig. 2), and two (40%) were of Grade III with medial violation. In all revision operations, the misplaced screws were removed and replaced by correctly placed ones. No spinal cord, dural, vascular, or pulmonary injuries have been detected. Sensitivity of CT images in assessing screw malposition compared with operative findings in revised screws showed a sensitivity of 97.6% and 100% and a specificity of 89.4% and 100% for axial image and 3D reformatted image, respectively.
Discussion
In our study, postoperative CT images were acquired after a month of pedicle screw fixation surgery. The incidence rate of screw violation identified in previous studies ranged from 0% to 42% [12]. This wide variety was due to various reasons such as the indication for surgery, the involved spinal levels, the operative procedure, the intraoperative-assisted guidance, the surgical experience, and the tool of postoperative assessment [13]. In our study, these issues have been standardized as much as possible.
In this study, the frequency of screw violation was 15.88% which was within the reported range of published studies. Laine et al. [14] reported 35.22% of screw violation, and Castro et al. [15] detected cortical penetration in 40% of their patients. Our frequency of screw violation was lower than that reported in these studies.
On the other side, our frequency was higher than that reported in other studies [16,17,18,19]. This difference may be explained by that many authors considered screw displacement of <2 mm was insignificant, and they did not include this group in the their final frequency. In our study, we included all grades of displacement even those with <2 mm in the total rate of screw displacement. Elyan et al. [20] and El Fiki et al. [21] reported screws displacement rates of 17.3% and 16.45%, respectively, which were similar to that found in our study.
Also, lower rates of screw displacement were reported in a meta-analysis conducted by Schizas et al. [22]. They reported a mean displacement rate of 8.7%. Lonstein et al. [23] also reported a displacement rate of 5.1% that has been related to the use of conventional plain radiographs as a postoperative assessment tool, with underestimation of displacement rate compared to CT scan [24].
Other studies used two dimensional (2D) axial CT images for postoperative assessment of pedicle screws. Adding 3D VR or coronal MPR procedures provided more detailed data in evaluating the placement of pedicle screws [15, 25, 26].
Multi-slice 3D reformatted image displayed the full length of the screw with absence of metallic artifacts and accurate assessment of the relation between the screw and neural structures [24]. In our study, axial images detected 36 (10.59%) out of the displaced screws seen at coronal reconstruction of 48 (14.12%) and 3D reformatted image of 54 (15.88%).
Our results agree with Schizas et al. [22] who compared axial CT images with coronal reconstruction and reported that the incidence of displacement was 23.3% for axial and 30% for coronal images. Also, in the study that was conducted by Celik et al. [27], the authors compared the axial images with 3D reformatted images, and they found lower incidence for axial (9%) compared to that of 3D reformatted images (13.1%). And, they explained that this difference is due to the fact that reformatted images evaluate cranial and caudal placement accuracy in addition to medial and lateral screw placement. Also, the presence of metallic artifacts in axial images affected the image interpretation.
In our study, the rate of screw displacement was higher in dorsal pedicles (31.4%) as compared with that in the lumbo-sacral ones (11.9%). This could be explained by the small size of pedicles in the dorsal spines and increasing variability in their anatomy [11, 21, 24, 28]. This was in accordance with previous studies [19, 21, 29, 30] that reported a higher rate of screw displacement in dorsal than lumbar spines. We revealed the highest incidence of screw displacement was at T11 (40%) followed by T9 (30%). This could be explained by the relatively small diameter of pedicles of dorsal spine to fit the screw.
In our study, the rate of lateral violation was (57.41%) more than the medial one (20.37%). Our results agree with many authors [5, 21, 29, 31] who reported a higher rate of lateral violation, and this is because the surgeons choose a more lateral track away from the more dense medial cortical wall of the pedicle and also to avoid spinal cord injury.
In this study, pedicle penetration was more frequently in lateral and medial walls and less in inferior (12.96%) and superior ones (9.26%). This was because of the pedicle anatomy [32]. These results were in accordance with that shown by previous studies [1, 19, 21, 33].
In our study, we reported neurologic sequels in seven of patients (10%). This was within the range reported in previous studies (0.2% to 11%) [21, 34]. While our results were less than that reported by Lotfnia et al. [31] (15.09%), the higher incidence in the later study might be due to the involvement of all patients with sensory or motor symptoms in spite of the existence or absence of neurological deficits.
Not all patients with displaced screws need revision surgery [21, 31]. This agreed with our results where only three patients out of seven need revision surgery with a revision rate of 1.47% among the inserted screws. Also, our results are in agreement with Parker et al. [29] who reported a 0.8% revision rate and completely agreed with El Fiki et al. [21]. No definitive dural, vascular, or pulmonary injuries were reported in our patients. These were in accordance with El Fiki et al. [21], Rodrigues et al. [30], and Reidy et al. [34].
Sensitivity of CT images in assessing screw position compared with operative findings in five revised screws revealed a sensitivity of 100% and 97.6% and a specificity of 100% and 89.4% for 3D reformatted image and axial image, respectively. These results were in accordance with El Fiki et al. [21], who reported sensitivity of 100% and 95.8% and a specificity of 100% and 88.7% for 3D reformatted image and axial image, respectively. Elyan et al. [20] reported sensitivity of 100%, 66.7%, and 33.3% and a specificity of 100%, 76%, and 38.5% for 3D reformatted, coronal, and axial images, respectively, among 24 cases. The lower values of sensitivity and specificity for coronal and axial images in the later study may be explained by the small number of studied cases.
Conclusion
In conclusion, 320 multi-slice CT scans is a valuable and valid tool for postoperative assessment of spinal pedicle screw placement.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 2D:
-
Two dimensional
- 3D VR:
-
Three-dimensional volume rendering
- 3D:
-
Three-dimensional
- L:
-
Lumbar
- MPR:
-
Multi-planar reformation
- MSCT:
-
Multi-slice computed tomography
- S:
-
Sacral
- T:
-
Thoracic
References
Saif M, Bakir A, Dawood S (2017) Post-operative computed tomography to evaluate the accuracy of thoracic and lumbosacral spine pedicular screw fixation. J Fac Med Baghdad 59(3):198–203
Motiei-Langroudi R, Sadeghian H (2015) Assessment of pedicle screw placement accuracy in thoracolumbosacral spine using freehand technique aided by lateral fluoroscopy: results of postoperative computed tomography in 114 patients. Spine J 15:700–704
Laine T, Lund T, Ylikoski M, Lohlikoski J, Schlenzka D (2000) Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. Eur Spine J 9:235–240
Güven O, Yalçin S, Karahan M, Sevinç TT (1994) Postoperative evaluation of transpedicular screws with computed tomography. Orthop Rev 23:511–516
Gonzalez-Cruz J, Karim A, Mukherjee D, Ogden A, Smith D, Nanda A (2006) Accuracy of pedicle screw placement for lumbar fusion using anatomic landmarks versus open laminectomy: comparison of two surgical techniques in cadaveric specimens. Oper Neurosurg 1:13–19
Meter JJ, Polly DW, Miller DW, Popovic NA, Ondra SL (1996) A method for radiographic evaluation of pedicle screw violation of the vertebral endplate: technique. Spine 21:1587–1592
Rutherford Elizabeth E, Tarplett Linda J, Davies Evan M, Harley John M, King Leonard J (2007) Lumbar spine fusion and stabilization: hardware, techniques, and imaging appearances. Radiographics 27:1737–1749
Berquist TH (2006) Imaging of the postoperative spine. Radiol Clin N Am 44:407–418
Douglas-Akinwande AC, Buckwalter KA, Rydberg J, Rankin JL, Choplin RH (2006) Multichannel CT: evaluating the spine in postoperative patients with orthopedic hardware. RadioGraphics 26:97–110
Kachelriess M, Sennst DA, Leidecker C, Schmidt B, Watzke O, Kalender WA (2004) An extensible software-based platform for reconstruction and evaluation of CT images. Radiographics 24(2):601–613
Rao G, Brodke DS, Rondina M, Bacchus K, Dailey AT (2003) Inter- and intraobserver reliability of computed tomography in assessment of thoracic pedicle screw placement. Spine 28(22):2527–2530
Gautschi Oliver P, Bawarjan S, Karl S, Enrico T (2011) Clinically relevant complications related to pedicle screw placement in thoracolumbar surgery and their management: a literature review of 35,630 pedicle screws. Neurosurg Focus 31(4):8–16
Vincenzo A, Luigi G, Irace C, Corona C (2010) Accuracy of pedicle screw placement in the lumbosacral spine using conventional technique: computed tomography postoperative assessment in 102 consecutive patients. J Neurosurg Spine 12:306–313
Laine T, Schlenzka D, Makitalo K, Tallroth K, Nolte LP, Visarius H (1997) Improved accuracy of pedicle screw insertion with computer-assisted surgery: a prospective clinical trial in 30 patients. Spine 22:1254–1258
Castro WHW, Halm H, Jerosch J (1996) Accuracy of pedicle screw placement in lumbar vertebrae. Spine 21:1320–1324
Amiot LP, Lang K, Putzier M (2000) Comparative results between conventional and computer-assisted pedicle screw installation in the thoracic, lumbar, and sacral spine. Spine 25:606–614
Weise L, Suess O, Picht T et al (2008) Transpedicular screw fixation in the thoracic and lumbar spine with a novel cannulated poliaxial screw system. Med Devices 1:33–39
Lothar W, Ralph K, Peter SK, Wolfgang R (2000) Clinical evaluation and computed tomography scan analysis of screw tracts after percutaneous insertion of pedicle screws in the lumbar spine. Spine 25(5):615–621
Aslanbaş O, Oktay K, Özsoy KM, Çetinalp NE, Tuna MG (2018) Assessment of pedicle screw malposition rates in thoracolumbosacral spine: results of postoperative computed tomography in 100 patients. Cukurova Med J 43(4):816–820
Elyan RM, Sanor AM, Abdel-Rahman HEM, Hafez FFM (2017) Role of multi-slice computed tomography in the evaluation of postoperative spine with spinal fixation. Master degree thesis, Radiodiagnosis Department, faculty of medicine, Zagazig Univeristy, Egypt
El Fiki IM, Zaiton F, Awadalla AM (2013) Role of postoperative multislice computed tomography in assessment of pedicle screw placement in spinal surgical fixation. Egypt J Radiol Nucl Med 44:63–70
Schizas C, Michel J, Kosmopoulos V, Theumann N (2007) Computed tomography assessment of pedicle screw insertion in percutaneous posterior transpedicular stabilization. Eur Spine J 16:613–617
Lonstein JE, Denis F, Perra JH et al (1999) Complications associated with pedicle screws. J Bone Joint Surg Am 81:1519–1528
Ashraf S, Ezz EA (2011) Postoperative computed tomography scan assessment of accuracy of pedicle screw placement in dorsolumbar and lumbosacral spine fractures. Egy J Neur Surg 26(1):15
Kim YJ, Lenke LG, Cheh G (2005) Evaluation of pedicle screw placement in the deformed spine using intraoperative plain radiographs: a comparison with computerized tomography. Spine 30:2084–2088
Victor K, Nicolas T, Stefano B, Constantin S (2007) Observer reliability in evaluating pedicle screw placement using computed tomography. Int Orthop 31:531–536
Suat CE, Bilal K, Recai G, Cevri YA (2009) The accuracy of multi-slice three-dimensional computerized tomography on the verification of the pedicle screw trajectory. Orthopedic Rev 1(22):56–59
Jonathan MB, Doug F, Jeremy LF, Eric WN (2009) Accuracy of upper thoracic pedicle screw placement using three-dimensional image guidance. Spine J 9(10):817–821
Parker Scott L, McGirt Matthew J, Harrison Farber S, Amin Anubhav G, Anne-Marie R, Ian S et al (2011) Accuracy of freehand pedicle screws in the thoracic and lumbar spine: analysis of 6816 consecutive screws. Neurosurgery 68:170–178
Rodrigues LMR, Nicolau RJ, Carlo M (2011) Computed tomographic evaluation of thoracic pedicle screw placement in idiopathic scoliosis. J Pediatr Orthop B 20(4):195–198
Iraj I, Sayyahme S, Gavam M (2010) Postoperative computed tomography assessment of pedicle screw placement accuracy. Turkish Neurosurg 20(4):500–507
Attar A, Ugur HC, Uz A (2001) Lumbar pedicle: surgical anatomic evaluation and relationships. Eur Spine J 10:10–15
Tian NF, Xu HZ (2009) Image-guided pedicle screw insertion accuracy: a meta-analysis. Int Orthop 33:895–903
Reidy DP, Houlden D, Nolan PC, Kim M, Finkelstein JA (2001) Evaluation of electromyographic monitoring during insertion of thoracic pedicle screws. J Bone Joint Surg Br 83:1009–1014
Acknowledgements
We would like to thank all participants in our study for their great help and patience.
Funding
No funding had been received.
Author information
Authors and Affiliations
Contributions
AAS set up the design of the study, performed the statistical analysis, assessment, and analysis of images, analyzed the results, and helped in writing, revising, and publishing the study. MAA choose the study idea, helped in the assessment and analysis of images, and revised the final draft of the study. AYS performed and followed up the spinal fixation operations for study participants and revised the final draft of the study. AE participated in the performance and following up the spinal fixation operations for study participants and revised the final draft of the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
-
The manuscript was approved by The Research Ethics Committee and Quality Assurance Unit, Faculty of Medicine, Tanta University.
-
The URL: http://tqac.tanta.edu.eg/new-tqac/QualityAssuranceUnit@hotmail.com
-
Approval Code: 1860/05/13
-
Name of the PI: Alsiagy A. Salama
-
Name of the department: Diagnostic Radiology
-
Type of the research: Promotion research
-
Date of approval: May 2013
-
All patients included in this study gave written informed consent to participate in this research, and any possible risks were clarified.
Consent for publication
All patients included in this research gave written informed consent to publish the data contained within this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Salama, A.A., Amin, M.A., Soliman, A.Y. et al. Postoperative 320 multi-slice computed tomography in assessment of pedicle screw insertion in thoraco-lumbar fixation. Egypt J Radiol Nucl Med 50, 57 (2019). https://doi.org/10.1186/s43055-019-0050-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-019-0050-7