Abstract
Background
The aim of this study was to evaluate the clinical reliability of ultrasound (US) examination using relative laryngeal movement of 40% as a cutoff point to diagnose pharyngeal abnormalities of swallowing using ultrasonographic examination in dysphagic cerebral palsy (CP) patients and comparing its results with a flexible fiberoptic endoscope.
Methods
Twenty-five cerebral palsy children suffering from clinical dysphagia were included in this study. The rest distance between the thyroid cartilage and the hyoid bone and the shortest distance between them during swallowing were measured by ultrasound, then the approximation distance and the percentage of relative laryngeal movement were calculated. All children also have been submitted for flexible fiberoptic endoscopy (FEES).
Results
The mean value of the percentage of relative laryngeal movement was significantly less in the CP children with pharyngeal phase abnormality diagnosed by the flexible fiberoptic endoscope (p < 0.001). The mean of relative laryngeal movement in CP patients with and without pharyngeal abnormality diagnosed by the flexible fiberoptic endoscope was 20.10 ± 13.73 and 66.19% ± 3.42 respectively.
Conclusion
Ultrasound can efficiently measure the relative laryngeal movement, and as it gives a numerical value, it can be used as a follow-up bedside test in children suffering from dysphagia.
Similar content being viewed by others
Background
Cerebral palsy (CP) is a chronic disorder affecting patient movement [1], and approximately 75% of CP children have dysphagia, which causes malnutrition and impacts their development [2].
The fiberoptic endoscopy (FEES) is used in the assessment of swallowing, particularly the pharyngeal stage [3]; it can be used to demonstrate the penetration and/or aspiration [4], but it does not provide direct information on laryngeal elevation or hyoid–larynx approximation [5].
Dynamic laryngeal movement during swallowing with laryngeal elevation and hyoid–larynx approximation is an essential component of swallowing [6, 7], and it is associated with bolus passage through the pharynx, opening and closure of the cricopharyngeal muscle, and also airway protection [8, 9].
Ultrasound (US) can detect and recognize the hyoid bone and thyroid cartilage, and hence, the percentage of hyoid–laryngeal approximation can be calculated by the measurement of the approximation distances of the two structures [5].
The aim of this work is to assess the diagnostic performance of US for diagnosing abnormalities in the pharyngeal phase of swallowing in dysphagic CP patients using reduced relative laryngeal movement of ≤ 40% compared to flexible fiberoptic endoscopy.
Methods
Patients
The study was done in the Ain Shams Specialized Hospital during the period from August 2016 till February 2017. Twenty-five cerebral palsy children with dysphagia were included in this study. Both fiberoptic endoscopic examination and US examination were done in the same day. Written consents were taken from all parents of patients to participate in this study, according to the rules of the ethical committee.
Technique of US examination
-
Ultrasound assessment was carried out by the same operator for all patients.
-
Children sat with the assistance of their relative to the most comfortable position for them.
-
An ultrasound was performed using an ultrasound machine (LOGIQ™ P7, GE Healthcare) using a high-frequency probe (7–10 MHz). Axial and sagittal ultrasound scanning was performed.
-
The transducer was placed in the midsagittal plane, centered between the anterior border of the hyoid bone and the superior border of the thyroid cartilage, with the central sound wave running perpendicular to this plane.
-
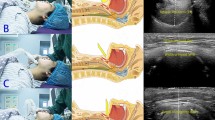
2 to 3 ml of water was inserted into patient’s mouth, then the process of laryngeal elevation using dynamic images with the assist of a cine loop was evaluated (Fig. 1).
-
The distance between the thyroid cartilage and hyoid bone before swallowing (rest distance) was measured and recorded as well as the shortest distance during the swallowing process (Fig. 2).
-
The approximation distance was obtained by subtracting the shortest distance between the thyroid cartilage and hyoid bone during swallowing from the resting distance.
-
Then the percentage of relative laryngeal movement was calculated by dividing the approximation distance by the resting distance.
-
The swallowing process was repeated while the transducer was placed in the axial plane with sequential images obtained at the level of the thyroid cartilage to evaluate if there is spillage of water into the laryngeal airway (Fig. 3).
Fiberoptic endoscopy (FEES)
-
FEES was carried out by a phoniatric to assess if there was a pharyngeal phase of swallowing abnormalities.
Analysis of data
-
A relative laryngeal movement less than 40% [5] considered as a diagnostic value for the pharyngeal phase of dysphagia, and the US results were compared to the FEES results.
-
The B mode examination was also done, and penetration/aspiration was diagnosed if water was seen at the level of the vocal cord.
-
The analysis data was done using IBM SPSS statistics (V. 25.0, IBM Corp., USA, 2017). Data were expressed as mean ± SD for quantitative parametric measures in addition to median percentiles for quantitative non-parametric measures and both the number and percentage of categorizing data. Diagnostic validity tests were used, including diagnostic sensitivity and specificity.
Results
Twenty-five CP children with a clinical diagnosis of dysphagia underwent both US examination and FEES. No adverse events occurred during both procedures. The median patient age was 3.5 years.
The median US resting distance was 1.39 cm, and the median US shortest distance was 0.62 cm, while the median US relative laryngeal movement was 63.28% (Table 1).
Of the 25 patients studied, the FEES examination revealed pharyngeal dysphagia in 10 out of 25 (40%) patients, while the US examination revealed reduced relative laryngeal movement (≤ 40%) in 9 out of 25 (36%) patients with a significant correlation between both US and FEES (p value < 0.001) (Table 2). The mean of the reduced relative laryngeal movement in these patients was 20.10 ± 13.73.
The FEES examination revealed normal swallowing in 15 out of 25 (60%) patients while the US examination revealed normal relative laryngeal movement in 16 out of 25 (64%) patients with a significant correlation between both US and FEES (p value < 0.001). The mean of relative laryngeal movement in these patients was 66.19% ± 3.42. The false negative case shows borderline relative laryngeal movement of 45%; yet during the B mode examination, fluid was seen spilled into the laryngeal airway, and the final US diagnosis of this case was an abnormal pharyngeal phase of swallowing (Table 3).
The inter-method agreement between the reduced relative laryngeal movement (≤ 40%) and FEES for diagnosing abnormalities of swallowing pharyngeal phase was 96%, with sensitivity, specificity, positive predictor value, and negative predictor value of 90%, 100%, 100%, and 93.75%, respectively, and the cutoff of our study was 45% with 100% sensitivity, specificity, positive predictive value, and negative predictor value (Table 4).
Discussion
This study demonstrated that ultrasonography quantitatively evaluated reduced laryngeal movement help in the assessment and diagnosis of pharyngeal phase dysphagia in CP children with sensitivity of 96%, and it can be used as an alternative to the FESS as it is a less-invasive and less costly bedside test.
Cerebral palsy is a permanent movement disorder which is attributed to disturbances in the developing fetal or infant brain, and it appears in early childhood [1].
Dysphagia is closely related to gross motor dysfunction in children with CP [10], and oropharyngeal dysphagia occurs in about 85% of children with CP [11].
Over the years, endoscopy has become a standard tool for diagnosing dysphagia [3] [12]. FEES investigates the pharyngeal phase only [13].
Real-time ultrasound is a non-ionizing imaging modality and has been used to observe deglutitive movements since the late 1970s [14, 15]. It was used in preliminary investigations of infants to visualize the bolus movement through the pharyngeal area while they are being breastfed [13].
Larynx elevation is crucial for airway protection and cricopharyngeal muscle relaxation [9, 16, 17]. As the thyroid cartilage approximates to the hyoid bone, the larynx elevates, the epiglottis tilts down and closes to prevent the bolus from entering the trachea, and cricopharyngeal muscle opens subsequently, allowing the bolus to pass through [18, 19]. So incomplete laryngeal elevation is assumed to be one of the major mechanisms in dysphagia and often leads to aspiration [20]. The fiberoptic endoscopic evaluation of deglutition is invasive and does not allow one to quantify swallowing movements [21].
The relative laryngeal movement is used in this study rather than the approximation distance to exclude the normal interpersonal variation, especially as the study deals with children in different ages.
In this study, the mean relative laryngeal movement in CP children with no pharyngeal abnormalities was 66.19% ± 3.42. Similar results were concluded by Kuhl et all. [22] who have examined 42 healthy people and 18 dysphagic patients suffering from different neurological diseases, and they found that the mean relative laryngeal movement was 61% ± 3 in normal subjects. Huang et al. [5] have also examined 15 normal volunteers, 20 patients without dysphagia, and 20 patients with dysphagia, and they found that the mean relative laryngeal movement in normal volunteers was 47.26 ± 4.9% and in stroke non-dysphagic patients 42.66 ± 8.3%.
In our study, the mean relative laryngeal movement in the dysphagic CP children suffering from pharyngeal abnormalities was reduced to less than 40% (20.10 ± 13.73); similar results were also concluded by Huang et al. [5] and Kuhl et al. [22] who showed reduced relative laryngeal movement to less than 40% in patient suffering from dysphagia (34.06 ± 10.9% and 42% ± 10 respectively).
In addition to the evaluation of relative laryngeal movement, B mode examination at the level of the thyroid cartilage may increase the sensitivity of US examination in diagnosing the pharyngeal phase of dysphagia, as the spillage of water into the laryngeal airway could be visualized in these children as air bubbles intermixed with water droplets, and it was beneficial in this study as the only false negative case which showed borderline reduced relative laryngeal movement (45%); penetration of water over the vocal cord was identified during B mode examination and the final US diagnosis was pharyngeal dysphagia.
The reduced relative laryngeal movement cut off value in this study was 45%, which was also similar to Huang et al.’s [5] result who found that the relative laryngeal movement of less than 40% may imply dysphagia, with acceptable sensitivity and specificity.
The limitation of this study is that we compare the result of reduced relative laryngeal movement with the clinical result of FEES, rather than the videofluoroscopic examination which is the gold standard examination for the evaluation of swallowing where the laryngeal movement can be readily measured and compared, yet we use the FEES to avoid exposing the children to X-rays, and despite the limitation of this study, the advantage of US of being a noninvasive, radiation-free, and less-expensive bedside procedure in addition to its quantitative value makes it an emergent and promising examination which can be used in the screening and serial monitoring for treatment response of dysphagia in children; another advantage of US examination is that it can be repeated many times without influencing the children or their parent any psychological disturbance.
Conclusion
Ultrasound can efficiently measure the relative laryngeal movement, which is an important parameter of the swallowing process, and as it gives a numerical value, it can be used as a follow-up bedside test in children suffering from dysphagia.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CP:
-
Cerebral palsy
- FEES:
-
Fiberoptic endoscopic
- US:
-
Ultrasound
References
Shkedy Rabani A, Harries N, Namoora I, Al-Jarrah MD et al (2014) Duration and patterns of habitual physical activity in adolescents and young adults with cerebral palsy. Dev Med Child Neurol 56(7):673–680
Song J, Park H, Lee H et al (2015) Effect of neuromuscular electrical stimulation on swallowing functions in children with cerebral palsy: a pilot randomized controlled trial. Hong Kong J Occup Ther 25:1–6
Sitton M, Arvedson J, Visotcky A et al (2011) Fiberoptic endoscopic evaluation of swallowing in children: feeding outcomes related to diagnostic groups and endoscopic findings. Int J Pediatr Otorhinolaryngol 75(8):1024–1031
Hiss SG, Postma GN (2003) Fiberoptic endoscopic evaluation of swallowing. Laryngoscope 113:1386–1393
Huang Y-L, Hsieh S-F, Chang Y-C et al (2009) Ultrasonographic evaluation of hyoid–larynx approximation in dysphagic stroke patients. Ultrasound Med Biol. 35(7):1103–1108
Cichero J (2006) Conditions commonly associated with dysphagia. In: Cichero J, Murdoch B (eds) Dysphagia: foundation, theory and practice. Wiley, Chichester, England/New York, pp 237–243
Leonard RJ, Kendall KA, McKenzie S et al (2000) Structural displacements in normal swallowing: a videofluoroscopic study. Dysphagia 15:146–152
Mendelsohn MS, McConnel FM (1987) Function in the pharyngoesophageal segment. Laryngoscope 97:483–489
Sivarao DV, Goyal RK (2000) Functional anatomy and physiology of the upper esophageal sphincter. Am J Med 108(4a):27–37
Kim JS, Han ZA, Song DH et al (2013) Characteristics of dysphagia in children with cerebral palsy, related to gross motor function. Am J Phys Med Rehabil. 92(10):912–919
Benfer KA, Weir KA, Bell KL et al (2013) Oropharyngeal dysphagia and gross motor skills in children with cerebral palsy. Pediatrics. 131(5):1553–1562
Sarwat SA (2016) The role of fiberoptic endoscopic evaluation of swallowing in the assessment of pediatric dysphagia. Egyptian J Otolaryngol. 32:67–74
Dodrill P (2015) Gosa MM (2015): Pediatric dysphagia: physiology, assessment, and management. Ann Nutr Metab. 66(5):24–31
Chi-Fishman G (2005) Quantitative lingual, pharyngeal and laryngeal ultrasonography in swallowing research: a technical review. Clin Linguist Phon 19:589–604
Shawker TH, Sonies B, Hall TE et al (1984) Ultrasound analysis of tongue, hyoid, and larynx activity during swallowing. Invest Radiol 19:82–86
Cook IJ, Dodds WJ, Dantas RO et al (1989) Opening mechanisms of the human upper esophageal sphincter. Am J Physiol 257:G748–G759
Ishida R, Palmer JB, Hiiemae KM (2002) Hyoid motion during swallowing: factors affecting forward and upward displacement. Dysphagia 17:262–272
Kendall KA, McKenzie S, Leonard RJ et al (2000) Timing of events in normal swallowing: a videofluoroscopic study. Dysphagia 15:74–83
Ohmae Y, Logemann JA, Kaiser P et al (1995) Timing of glottic closure during normal swallow. Head Neck 17:394–402
Veis SL, Logemann JA (1985) Swallowing disorders in persons with cerebrovascular accident. Arch Phys Med Rehabil 66:372–375
Leder SB, Sasaki CT, Burrell MT (1998) Fiberoptic endoscopic evaluation of dysphagia to identify silent aspiration. Dysphagia 13:19–21
Kuhl V, Eicke BM, Dieterich M, Urban PP (2003) Sonographic analysis of laryngeal elevation during swallowing. J Neurol 250:333–337
Acknowledgements
Not applicable
Funding
No funds, sponsorship, or financial support to be disclosed.
Author information
Authors and Affiliations
Contributions
AA has performed the ultrasound examination and carried out the interpretation of US images. He has participated in the data collection and writing the manuscript. EA has participated in the data collection, conceived of the study, and helped to draft the manuscript. SB has performed the flexible fiberoptic endoscope procedure and carried out the interpretation of them. HE has participated in the data collection and team organization and participated in the result interpretation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Available
Consent for publication
Not applicable
Competing interests
We agree that all copyright ownership is transferable to the Association of University Radiologists when the manuscript is accepted for publication in EJRNM. We certify that the submitted article will not constitute “Redundant Publication.” This study is not previously published nor submitted elsewhere and the methods employed respect the Helsinki Declaration of 1975, as revised in 1983. The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Abdelrahman, A.S., Abdeldayem, E.H., Bassiouny, S. et al. Role of ultrasound in evaluation of pharyngeal dysphagia in children with cerebral palsy. Egypt J Radiol Nucl Med 50, 14 (2019). https://doi.org/10.1186/s43055-019-0014-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-019-0014-y