Abstract
Background
Early and accurate risk assessment is an important clinical demand in patients with infective endocarditis (IE). The neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) are independent predictors of prognosis in many infectious and cardiovascular diseases. Very limited studies have been conducted to evaluate the prognostic role of these markers in IE.
Results
We analyzed clinical, laboratory, and echocardiographic data and outcomes throughout the whole period of hospitalization for a total of 142 consecutive patients with definitive IE.
The overall in-hospital mortality was 21%. Major complications defined as central nervous system embolization, fulminant sepsis, acute heart failure, acute renal failure, and major artery embolization occurred in 38 (27%), 34 (24%), 32 (22.5%), 40 (28%), and 90 (63.4%) patients, respectively.
The NLR, total leucocyte count (TLC), neutrophil percentage, creatinine, and C-reactive protein (CRP) level obtained upon admission were significantly higher in the mortality group [p ≤ 0.001, p = 0.008, p = 0.001, p = 0.004, and p = 0.036, respectively].
A higher NLR was significantly associated with fulminant sepsis and major arterial embolization [p = 0.001 and p = 0.028, respectively].
The receiver operating characteristic (ROC) curve of the NLR for predicting in-hospital mortality showed that an NLR > 8.085 had a 60% sensitivity and an 84.8% specificity for an association with in-hospital mortality [area under the curve = 0.729, 95% confidence interval (CI) 0.616–0.841; p = 0.001]. The ROC curve of the NLR for predicting severe sepsis showed that an NLR > 5.035 had a 71.8% sensitivity and a 68.5% specificity for predicting severe sepsis [area under the curve 0.685, 95% CI 0.582–0.733; p = 0.001].
The PLR showed no significant association with in-hospital mortality or in-hospital complications.
Conclusion
A higher NLR, TLC, neutrophil percentage, creatinine level, and CRP level upon admission were associated with increased in-hospital mortality and morbidity in IE patients. Furthermore, a lower lymphocyte count/percentage and platelet count were strong indicators of in-hospital mortality among IE patients.
Calculation of the NLR directly from a CBC upon admission may assist in early risk stratification of patients with IE.
Similar content being viewed by others
Background
Infective endocarditis (IE) is an infection of the heart valves (native or prosthetic); large intrathoracic vessels; intracardiac structures, such as the interventricular septum, chordae tendineae, or mural endocardium; and intracardiac foreign bodies. Despite improvements in the diagnosis and treatment of IE, the in-hospital mortality and morbidity rates of this infection remain high [1,2,3,4].
Recently, with the growing understanding of the roles of various inflammatory markers in IE, studies have focused on new, widely available, and inexpensive inflammatory markers. Recent studies have revealed that various markers, including the WBC count, neutrophil-to-lymphocyte ratio (NLR), and mean platelet volume, are associated with IE and its prognosis [4,5,6,7].
The NLR, a novel marker, has been studied in various immunologic and infectious diseases as well as cardiologic disorders. The NLR is simply acquired using a complete blood count (CBC), which is the most commonly performed test in hospitals.
The NLR has been evaluated in various cardiac disorders, including atherosclerotic heart disease. Studies have revealed considerable prognostic value in addition to significant positive correlations. The predictive value of the NLR for peripheral arterial disease, calcific aortic stenosis, the presence, severity and extent of coronary artery disease, and many other cardiovascular disorders has been shown [8,9,10,11,12,13,14,15].
Platelets are well-established components of the hemostatic system. Recently, several additional functions of platelets have been demonstrated in the pathogenesis of various inflammatory diseases. The lymphocyte count is inversely correlated with inflammation. A lower lymphocyte count indicates an increased risk of inflammation, which correlates with cardiovascular disease burden and mortality [15, 16]. Therefore, the platelet-to-lymphocyte ratio (PLR) is positively correlated with inflammation and can therefore be a useful biomarker to predict the severity of inflammation.
Recently, the PLR was used as a worse prognostic marker for various cardiovascular conditions [17, 18]. However, very limited data are available regarding its predictive role in patients with IE [19]. In our study, we aimed to assess the relationship of the PLR and NLR that are obtained on admission with in-hospital morbidity and mortality in patients with IE, and we compared these two ratios.
Methods
Study design
This is a retrospective analytic study. Patients with definitive/possible IE according to the modified Duke criteria, as diagnosed by the Kasr Al Ainy IE Working Group from January 2011 through July 2016, were reviewed in this study. Only patients for whom full laboratory data were available were enrolled. The IE Working Group used the AHA/ACC guidelines and the ESC guidelines for the diagnosis and management of IE patients [1, 2].
At least three sets of blood cultures were collected for each patient prior to initiating antibiotics. Cultures were collected from different venepunctures, with the first and last samples drawn at least 1 h apart. Each blood culture set consisted of one BACTEC Plus Aerobic/F and one BACTEC Plus anaerobic/F culture vial (Becton Dickinson, Sparks, MD, UAE).
Surgically excised materials, including excised valves, vegetations, infected prostheses, aortic abscesses, and emboli, were submitted for Gram staining, potassium hydroxide preparation (KOH), histopathological examination, and microbial culture.
Serodiagnosis for the detection of antibodies specific to Brucella, Bartonella, and Coxiella and Aspergillus Galactomannan Antigen was performed routinely for all patients.
Trans-thoracic echocardiography (TTE) was performed within 24 h of admission. Transesophageal echocardiography (TEE) was performed, as indicated, within 48–72 h. All images were standardized according to the guidelines of the American Society of Echocardiography [20, 21].
All hematologic and biochemical data were obtained from venous blood samples drawn on the first day when patients were admitted to our hospital.
CBC hemoglobin, total leucocyte count (TLC), neutrophil, lymphocyte, and platelet counts were calculated using a Cell-Dyn 3700 automated cell counter. The PLR and NLR were directly obtained from the CBC on admission [22,23,24].
-
Significant anemia was defined as a blood hemoglobin level < 10 mg/dl to avoid mild anemia that could be attributed to nutritional factors.
-
Normal values of the TLC were defined as ranges from 4000 to 11000/c mm.
-
Normal neutrophil percentage ranges were considered to be from 40 to 75%.
-
Normal lymphocyte percentage ranges were considered to be from 20 to 45%.
-
Normal platelet count ranges were considered to be from 150–400 × 103/L.
C-reactive protein (CRP), serum creatinine, and rheumatoid factor levels were all assessed on admission and periodically across each patient’s in-hospital course.
Severe (fulminant) sepsis was defined as sepsis necessitating ventilation or vasopressor support.
Statistical analysis
Data were coded and entered using the statistical package SPSS (Statistical Package for the Social Sciences) version 23. Data were summarized using the mean, standard deviation, median, minimum, and maximum for quantitative data and using frequencies (counts) and relative frequencies (percentages) for categorical data. Comparisons between quantitative variables were performed using the non-parametric Mann-Whitney test (Chan, 2003a) [25]. For comparing categorical data, the chi-square (χ²) test was performed. An exact test was used instead when the expected frequency was less than 5 (Chan, 2003b) [26]. A receiver operating characteristic (ROC) curve was constructed, and an area under the curve analysis was performed to detect the best cutoff values of the PLR and NLR for detecting mortality and complications. Multivariate logistic regression was performed to identify independent predictors of mortality and complications. p values less than 0.05 were considered as statistically significant [26].
Approval
The study protocol was approved by the Kasr Al Ainy Ethical Committee.
Results
We reviewed 217 patients who were admitted with a diagnosis of definitive/possible IE by the IE working group at Kasr Al Ainy Teaching Hospitals between January 2011 and July 2016. Complete hematological data were available for only 142 patients who were enrolled in the study.
Patients were young; the mean age was 30.95 ± 11.03 years (ranges 12–71). Males were more commonly affected than females (87 [61.3%] versus 55 [38.7%]). The median duration of hospitalization was 40 days (ranges 1–112 days).
Predisposing risk factors
Predisposing factors for IE were rheumatic heart disease (RHD) in 74 patients (52.1%), prosthetic valve and intracardiac devices in 41 patients (28.9%), intravenous (IV) drug abuse in 27 patients (19.1%), congenital heart disease (CHD) in 12 patients (8.5%), and degenerative heart disease in 3 patients (2.1%). A history of previous IE was found in 8 patients (5.6%).
Causative organisms
Causative organisms were identified by blood/tissue culture or serology in 85 patients (59.9%). The most common organisms were Staphylococci [40 patients (47.1%), 40% of them had methicillin-resistant S. aureus (MRSA)], followed by zoonotic organisms as a cause of IE in 14 patients (16.5%) [Brucella spp. in 8 patients, Bartonella henselae in 5 patients and Coxiella burnetii in one patient], and Streptococci (12 patients, 14.1%). Fungi were identified in 11 patients (12.9%).
Laboratory parameters
CBCs were obtained on admission, and CBC parameters were analyzed. Serum creatinine, CRP, and rheumatoid factor levels were also analyzed. Patients were generally anemic with a mean hemoglobin level of 9.89 ± 1.82 gm/dL and a median of 9.75 gm/dL (range, 5.30–14.30 gm/dL). CRP levels were notably high, with a mean of 94.49 ± 74.62 mg/L. Serum creatinine levels were also elevated (mean, 2.19 ± 6.56 mg/dL).
Hematological and other laboratory characteristics on admission are shown in Table 1.
Clinical course and in-hospital outcome
Fifty-seven patients showed a good response to medical treatment, defined as improvement in the general condition of the patient, declining levels of inflammatory markers, and disappearance of fever in response to antimicrobial therapy without surgical intervention.
Cardiac surgery was indicated in 100 patients (70.4%); however, it was only performed in 74 patients; some of the patients died short out of having surgery due to severe morbid condition while some others were scheduled for elective surgery after remission of acute IE episode. The most common indications for surgery were congestive heart failure (CHF) in 47 patients (47% of the total patients with indications for surgery) followed by severe uncontrolled infection in 33 patients (33%).
Major complications, including CHF (NYHA class III–IV), cerebrovascular stroke (CVS), intracranial hemorrhage (ICH), acute renal failure (ARF) requiring dialysis, fulminant sepsis, and major arterial embolization, occurred in 107 patients of the whole group whether indicated for surgery or not. Table 2 shows the details of the complication incidences.
The overall in-hospital mortality was 21.1%. The main causes of in-hospital death were fulminant sepsis, severe heart failure, and surgery-related mortality (40%, 20%, and 16.7% of overall mortality, respectively).
Predictors of in-hospital mortality
Fulminant sepsis, renal insufficiency (creatinine > 2 mg/dl), end-stage renal disease, splenic abscess/infarction, failure to respond to medical therapy alone, and major artery embolization were closely linked to mortality (p < 0.001, p < 0.001, p = 0.020, p = 0.054, p < 0.001, and p = 0.065, respectively). Clinical characteristics associated with increased in-hospital mortality are shown in Table 3.
Hemoglobin level was lower in the mortality group than in the non-mortality group (mean 9.31 ± 1.87 g/dL and 10.04 ± 1.79 g/dL, p = 0.076). A higher mean TLC on admission was noticed among the mortality group (14.6 ± 7.42 × 103/ml and 10.84 ± 4.66 × 103/ml, p = 0.008). The mean neutrophil percentage was significantly higher in the mortality group of patients (78.87% ± 15.11 to 70.37% ± 13.97, respectively, p = 0.001). A lower lymphocyte count/percentage and platelet count were strong indicators of the incidence of in-hospital mortality (p = 0.015, p < 0.001, and p = 0.001, respectively). CRP levels on admission were significantly higher (as a continuous variable) in the mortality group (the mean CRP level was 110 mg/L in the mortality group vs. 91 mg/L in the survival group, p = 0.036), and higher serum creatinine levels on admission and during hospitalization were significantly associated with an increased incidence of in-hospital mortality (p = 0.004 and p< 0.001, respectively).
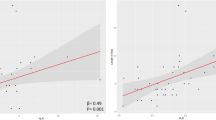
A higher NLR was significantly associated with an increased incidence of in-hospital mortality (p ≤ 0.001), and the ROC curve of the NLR for predicting in-hospital mortality is shown in Fig. 1. An NLR over 8.085 measured upon admission had a 60% sensitivity and an 84.8% specificity for predicting in-hospital mortality [area under the curve = 0.729, 95% confidence interval (CI) 0.616–0.841; p ≤ 0.001].
Laboratory characteristics associated with increased in-hospital mortality are shown in Table 4.
The number of vegetations was significantly associated with mortality; the higher the number of vegetations was, the higher the risk of the in-hospital mortality [p = 0.002]. Severe acute aortic regurgitation and prosthetic valve complications and MRSA or Candida infections were also associated with a high incidence of in-hospital mortality [p = 0.007, p = 0.030, and p = 0.030 or p = 0.028, respectively].
Through multivariate analysis, predictors of in-hospital mortality were a higher TLC on admission [odds ratio (OR) = 1.487; 95% CI, 1.173 to 1.863; p = 0.001], a low lymphocyte percentage on admission [OR = 1.207; 95% CI, 1.015 to 1.435; p = 0.033], and a low lymphocyte count on admission [OR = 0.998; 95% CI, 0.996 to 0.999; p = 0.008].
Predictors of in-hospital morbidities
A higher NLR was significantly associated with an increased incidence of fulminant sepsis and major artery embolization (p = 0.001 and p = 0.028, respectively).
The ROC curve of the NLR for predicting embolization to different organs is shown in Fig. 2. An NLR over 3.045 measured upon admission had a 73.3% sensitivity and a 51.9% specificity for predicting embolization [area under the curve 0.611, 95% CI 0.516–0.707; p = 0.028].
An NLR over 5.035 measured upon admission had a 71.8% sensitivity and a 68.5% specificity for predicting severe sepsis [area under the curve 0.685, 95% CI 0.582–0.733; p = 0.001]. The ROC curve of the NLR for predicting severe sepsis is shown in Fig. 3.
A higher CRP level on admission was also significantly associated with an increased incidence of CNS complications (p = 0.055).
While the PLR showed trends towards an increased incidence of in-hospital sepsis and major artery embolization (p = 0.136 and p = 0.186, respectively), there was no association between a higher PLR and in-hospital mortality in our patients.
Discussion
IE is an infrequent yet life-threatening disease with considerable morbidity and mortality rates that have been unchanged for more than 3 decades [1, 2, 6, 27]. The in-hospital mortality rate of patients with IE varies from 15 to 30% [28,29,30,31,32,33,34,35,36].
Rapid identification of patients at highest risk of death may offer the opportunity to change the course of the disease (i.e., emergency or urgent surgery) and improve prognosis [37]. Current guidelines recommend additional protective measures in high-risk patients [1, 2]; however, identifying patients at greater risk in the early phases of disease is not easy because of the non-uniformity and complexity of IE.
The PLR and NLR are independent predictors of worse prognosis in many infectious and cardiovascular diseases [8,9,10,11,12,13,14,15, 17, 18]; however, a very limited number of studies have been conducted to evaluate the prognostic role of these markers in IE [5,6,7, 19].
The aim of this study was to determine the value of the PLR and NLR as predictors of in-hospital morbidity and mortality among IE patients.
We analyzed clinical, laboratory, and echocardiographic data and the clinical course throughout the entire period of hospitalization in a total of 142 consecutive patients with definitive/possible IE diagnoses. The PLR and NLR were obtained directly from a CBC obtained upon admission.
In our study, the mortality rate was 21% (30 patients), while complications of CVS, fulminant sepsis, acute heart failure, ARF, and embolization to different vital organs occurred in 38 (27%), 34 (24%), 32 (22.5%), 40 (28%), and 90 (63.4%) patients, respectively.
We found that an NLR over 8.085 measured upon admission had a 60% sensitivity and an 84.8% specificity for predicting in-hospital mortality among IE patients [area under the curve = 0.729, 95% CI 0.616–0.841; p ≤ 0.001]; the high cutoff value in our study compared to the cutoff value of 7 from the study by Turak et al. [6] may be due to delayed presentation from the onset of disease symptoms (the mean time to referral in our study was 43 days) or introduction of antibiotics before referral, which alters the TLC and the NLR.
Additionally, we found that a high NLR on admission was significantly associated with an increased in-hospital incidence of severe sepsis. The ROC curve of the NLR for predicting severe sepsis shows that an NLR over 6.19 measured upon admission had a 71.8% sensitivity and a 68.5% specificity for predicting severe sepsis [area under the curve = 0.685, 95% CI; 0.582–0.733, p = 0.001]. This is also a higher cutoff value than that in the report by Turak et al. [6].
A higher NLR measured upon admission was also associated with an increased incidence of embolization to different organs [p = 0.028].
In our study, the PLR showed no significant association with in-hospital mortality or the occurrence of in-hospital complications in IE patients. To the best of our knowledge, only one study has been conducted to evaluate the relationship between the PLR and in-hospital mortality in IE patients. Zencir et al. retrospectively analyzed the data from 59 patients diagnosed with definitive IE and found that a higher PLR on admission was associated with increased in-hospital mortality in patients with IE (p = 0.008) [19].
To date, very few reports have referred to a possible prognostic role of CBC parameters in identifying high-risk IE patients. Further studies might be needed to evaluate the prognostic significance of such parameters.
Limitation of the study
The study was limited by being a retrospective study and by being carried out in a tertiary referral center where patients were referred late, which might have increased the incidence of morbidities and mortality.
Conclusion
A CBC is an easy non-invasive test that is routinely performed on IE patients on admission and during follow-up. In our study, a higher NLR, TLC, and CRP and creatinine levels (> 1.99 mg/dL) obtained upon admission were associated with increased in-hospital mortality and morbidity in IE patients. Additionally, a lower lymphocyte count/percentage and platelet count were strong indicators of in-hospital mortality among IE patients.
Calculation of the NLR directly from a CBC obtained upon admission may assist in early risk stratification of patients with IE.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- ARF :
-
Acute renal failure
- CBC:
-
Complete blood count
- CHD:
-
Congenital heart disease
- CHF:
-
Congestive heart failure
- CI:
-
Confidence interval
- CRP:
-
C-reactive protein
- CVS:
-
Cerebrovascular stroke
- ICH :
-
Intracranial hemorrhage
- IE:
-
Infective endocarditis
- KOH:
-
Potassium hydroxide preparation
- MRSA:
-
Methicillin-resistant S. aureus
- NLR:
-
Neutrophil-to-lymphocyte ratio
- PLR:
-
Platelet-to-lymphocyte ratio
- RHD :
-
Rheumatic heart disease
- ROC curve:
-
Receiver operating characteristic curve
- TEE:
-
Transesophageal echocardiography
- TLC:
-
Total leucocyte count
- TTE:
-
Trans-thoracic echocardiography
References
Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F et al (2015) 2015 ESC guidelines for the management of infective endocarditis: the task force for the management of infective endocarditis of the European Society of Cardiology (ESC) endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J 36(44):3075–3128
Baddour LM, Wilson WR, Bayer AS, Fowler VG Jr, Bolger AF, Levison ME et al (2005) Infective endocarditis: diagnosis, antimicrobial therapy, and management of complications: a statement for healthcare professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young, and the Councils on Clinical Cardiology, Stroke, and Cardiovascular Surgery and Anesthesia, American Heart Association: endorsed by the Infectious Diseases Society of America. Circulation. 111(23):e394–e434
Moreillon P, Que YA (2004) Infective endocarditis. Lancet. 363(9403):139–149
Gunebakmaz O, Kaya MG, Kaya EG, Ardic I, Yarlioglues M, Dogdu O et al (2010) Mean platelet volume predicts embolic complications and prognosis in infective endocarditis. Int J Infect Dis 14(11):e982–e985
Cornelissen CG, Frechen DA, Schreiner K, Marx N, Krüger S (2013) Inflammatory parameters and prediction of prognosis in infective endocarditis. BMC Infect Dis 13(1):272
Turak O, Özcan F, İşleyen A, Başar FN, Gül M, Yilmaz S et al (2013) Usefulness of neutrophil-to-lymphocyte ratio to predict in-hospital outcomes in infective endocarditis. Can J Cardiol 29(12):1672–1678
Bozbay M, Ugur M, Uyarel H, Cicek G, Koroglu B, Tusun E et al (2014) Neutrophil-to-lymphocyte ratio as a prognostic marker in infective endocarditis: in-hospital and long-term clinical results. J Heart Valve Dis 23(5):617–623
González-Fajardo JA, Brizuela-Sanz JA, Aguirre-Gervás B, Merino-Díaz B, Del Río-Solá L, Martín-Pedrosa M et al (2014) Prognostic significance of an elevated neutrophil–lymphocyte ratio in the amputation-free survival of patients with chronic critical limb ischemia. Ann Vasc Surg 28(4):999–1004
Açar G, Fidan S, Uslu ZA, Turkday S, Avci A, Alizade E et al (2015) Relationship of neutrophil–lymphocyte ratio with the presence, severity, and extent of coronary atherosclerosis detected by coronary computed tomography angiography. Angiology. 66(2):174–179
Arbel Y, Finkelstein A, Halkin A, Birati EY, Revivo M, Zuzut M et al (2012) Neutrophil/lymphocyte ratio is related to the severity of coronary artery disease and clinical outcome in patients undergoing angiography. Atherosclerosis. 225(2):456–460
Avci A, Elnur A, Göksel A, Serdar F, Servet I, Atilla K et al (2014) The relationship between neutrophil/lymphocyte ratio and calcific aortic stenosis. Echocardiography. 31(9):1031–1035
Shah N, Parikh V, Patel N, Patel N, Badheka A, Deshmukh A et al (2014) Neutrophil lymphocyte ratio significantly improves the Framingham risk score in prediction of coronary heart disease mortality: insights from the National Health and Nutrition Examination Survey-III. Int J Cardiol 171(3):390–397
Ommen OS, Gibbons GR, Hodge HD, Thomson TS (1997) Usefulness of the lymphocyte concentration as a prognostic marker in coronary artery disease. Am J Cardiol 79(6):812
Horne BD, Anderson JL, John JM, Weaver A, Bair TL, Jensen KR et al (2005) Which white blood cell subtypes predict increased cardiovascular risk? J Am Coll Cardiol 45(10):1638–1643
Sandhaus LM, Meyer P (2002) How useful are CBC and reticulocyte reports to clinicians? Am J Clin Pathol 118(5):787–793
Bath PM, Butterworth RJ (1996) Platelet size: measurement, physiology and vascular disease. Blood Coagul Fibrinolysis 7(2):157–161
Ayça B, Akin F, Çelik Ö, Yüksel Y, Öztürk D, Tekiner F, Çetin Ş, Okuyan E, Dinçkal MH (2015) Platelet to lymphocyte ratio as a prognostic marker in primary percutaneous coronary intervention. Platelets. 26(7):638–644
Hudzik B, Szkodzinski J, Gorol J, Niedziela J, Lekston A, Gasior M et al (2015) Platelet-to-lymphocyte ratio is a marker of poor prognosis in patients with diabetes mellitus and ST-elevation myocardial infarction. Biomarkers Med 9(3):199–207
Zencir C, Akpek M, Senol S, Selvi M, Onay S, Cetin M et al (2015) Association between hematologic parameters and in-hospital mortality in patients with infective endocarditis. Kaohsiung J Med Sci 31(12):632–638
Cheitlin MD, Armstrong WF, Aurigemma GP, Beller GA, Bierman FZ, Davis JL et al (2003) ACC/AHA/ASE 2003 guideline update for the clinical application of echocardiography: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASE Committee to Update the 1997 Guidelines for the Clinical Application of Echocardiography). J Am Coll Cardiol 42(5):954–970
Habib G, Badano L, Tribouilloy C, Vilacosta I, Zamorano JL, Galderisi M (2010) Recommendations for the practice of echocardiography in infective endocarditis. Eur J Echocardiogr 11(2):202–219
Tefferi A, Hanson CA, Inwards DJ. How to interpret and pursue an abnormal complete blood cell count in adults. In Mayo Clinic Proceedings 2005(Vol. 80, No. 7, pp. 923-936). Elsevier.
Fairbanks VF, Tefferi A (2000) Normal ranges for packed cell volume and hemoglobin concentration in adults: relevance to ‘apparent polycythemia’. Eur J Haematol. 65(5):285–296
Shearer WT, Rosenblatt HM, Gelman RS, Oyomopito R, Plaeger S, Stiehm ER et al (2003) Lymphocyte subsets in healthy children from birth through 18 years of age: the Pediatric AIDS Clinical Trials Group P1009 study. J Allergy Clin Immunol 112(5):973–980
Chan YH (2003) Biostatistics 102: quantitative data–parametric & non-parametric tests. Blood Press 140(24.08):79–00
Chan YH (2003) Biostatistics 103: qualitative data-tests of independence. Singapore Med J. 44(10):498–503
Tornos P, Gonzalez-Alujas T, Thuny F, Habib G (2011) Infective endocarditis: the European viewpoint. Curr Probl Cardiol 36(5):175–222
Duval X, Delahaye F, Alla F, Tattevin P, Obadia JF, Le Moing V et al (2012) Temporal trends in infective endocarditis in the context of prophylaxis guideline modifications: three successive population-based surveys. J Am Coll Cardiol 59(22):1968–1976
Murdoch DR, Corey GR, Hoen B, Miró JM, Fowler VG, Bayer AS et al (2009) Clinical presentation, etiology, and outcome of infective endocarditis in the 21st century: the International Collaboration on Endocarditis–Prospective Cohort Study. Arch Intern Med 169(5):463–473
Nadji G, Rusinaru D, Rémadi JP, Jeu A, Sorel C, Tribouilloy C (2009) Heart failure in left-sided native valve infective endocarditis: characteristics, prognosis, and results of surgical treatment. Eur J Heart Fail 11(7):668–675
Thuny F, Disalvo G, Belliard O, Avierinos JF, Pergola V, Rosenberg V et al (2005) Risk of embolism and death in infective endocarditis: prognostic value of echocardiography: a prospective multicenter study. Circulation. 112(1):69–75
Leone S, Ravasio V, Durante-Mangoni E, Crapis M, Carosi G, Scotton PG et al (2012) Epidemiology, characteristics, and outcome of infective endocarditis in Italy: the Italian Study on Endocarditis. Infection. 40(5):527–535
Meshaal MS, Labib D, Said K, Hosny M, Hassan M, Al Aziz SA et al (2018) Aspergillus endocarditis: diagnostic criteria and predictors of outcome. A retrospective cohort study. PloS One. 13(8):e0201459
Meshaal MS, Kassem HH, Samir A, Zakaria A, Baghdady Y, Rizk HH (2015) Impact of routine cerebral CT angiography on treatment decisions in infective endocarditis. PloS One. 10(3):e0118616
García-Cabrera E, Fernández-Hidalgo N, Almirante B, Ivanova-Georgieva R, Noureddine M, Plata A et al (2013) Neurological complications of infective endocarditis: risk factors, outcome, and impact of cardiac surgery: a multicenter observational study. Circulation. 127(23):2272–2284
Delahaye F, Alla F, Béguinot I, Bruneval P, Doco-Lecompte T, Lacassin F et al (2007) AEPEI GROUP. In-hospital mortality of infective endocarditis: prognostic factors and evolution over an 8-year period. Scand J Infect Dis 39(10):849–857
Olmos C, Vilacosta I, Fernandez C, Lopez J, Sarria C, Ferrera C et al (2012) Contemporary epidemiology and prognosis of septic shock in infective endocarditis. Eur Heart J 34(26):1999–2006
Acknowledgements
None
Funding
The authors did not receive any specific funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the research equally. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Kasr Al Ainy Ethical Committee. The ethical committee exempted the study from a specific consent, being a retrospective analytic study that reveals no identifiable personal or private information.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Meshaal, M.S., Nagi, A., Eldamaty, A. et al. Neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) as independent predictors of outcome in infective endocarditis (IE). Egypt Heart J 71, 13 (2019). https://doi.org/10.1186/s43044-019-0014-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43044-019-0014-2