Abstract
Background
Polycystic ovary syndrome (PCOS) is one of the most common endocrinopathies affecting 5–10% of women of reproductive age. The syndrome is surrounded by controversies regarding both its diagnosis and treatment. The introduction of long-acting GnRH agonists in the late 1980s revolutionized the approach to ovarian stimulation in assisted reproductive technologies by providing the means to downregulate endogenous pituitary gonadotropin secretion and thereby prevent a premature luteinizing hormone surge during exogenous gonadotropin stimulation. The relatively recent introduction of GnRH antagonists in clinical practice has provided another option for ovarian stimulation in IVF. The purpose of this study was to compare the efficacy of the fixed GnRH antagonist vs. GnRH agonist long protocol in patients with polycystic ovary syndrome treated by ICSI.
Results
There is a statistically significant difference between both groups in view of the received dose of gonadotrophin (1901.7 ± 400.6 vs. 1789 ± 368 with p = .004) and duration of stimulation (11.3 ± 0.8 vs. 10.3 ± 1.1 with p = .017). There is no significant difference between both groups in view of pregnancy outcome (37% vs. 32% with p = .125). There is a significant difference between both groups in view of ovarian hyperstimulation syndrome (OHSS) incidence where the rates were 15%, 6%, and 1.5% vs. 4.5%, 2.5%, and .05% with p = 0.04 for mild, moderate, and severe, respectively, form of OHSS in group 1 and group 2.
Conclusion
The antagonist protocol may be the preferred stimulation protocol for PCOS patients treated by ICSI in view of the reduction of OHSS incidence rates without compromising the pregnancy outcome.
Similar content being viewed by others
Background
In 2003, a group of experts agreed for the diagnostic criteria of PCO to include oligo-anovulation, hyperandrogenism/hyperandrogenemia, and polycystic ovaries seen at ultrasound as the third diagnostic markers and to allow for a diagnosis of PCOS. If two of the three criteria were met and the same endocrinopathies were excluded, these are known as the Rotterdam criteria [1].
Polycystic ovarian syndrome (PCOS) is a significant cause of infertility for patients seeking assisted reproductive procedures and occurs in 4–12% of the general population [2].
The objective of the study was to evaluate which protocol is more effective in the prevention of ovarian hyperstimulation syndrome (OHSS) in a specific group of patients (i.e., PCO).
Advantages of antagonists are the shorter duration of the analog treatment, the shorter duration of stimulation with FSH, and the lower risk of developing ovarian hyperstimulation syndrome (OHSS) [3].
One advantage in the context of preventing OHSS may be the possibility of triggering ovulation with a short endogenous luteinizing hormone (LH) surge induced with a GnRH agonist adminstration instead of the prolonged LH action induced by the administration of hCG. In addition, with the standard “long agonist protocol,” approximately 25 daily subcutaneous injections are needed, whereas antagonists require around 5 daily subcutaneous injections [4].
In this study, we compared two known protocols, long agonist and multiple-dose antagonist, for ovulation induction in PCOS patients with a primary goal of the estimation of OHSS incidence rates in addition to other ICSI outcomes such as the number of oocytes retrieved, fertilization, implantation, and pregnancy rates in both groups. It is well known that the comparison between agonist and antagonist had been previously reported in many studies, but we tried to emphasize the superiority of antagonist in the prevention of OHSS.
Previous studies did not account for various patient populations, especially PCOS patients, and so, we conducted this trial. Also, in this study, we used two arms of comparison in this group of patients, and this may add beneficial information about both types of stimulation particularly their effects on the occurrence of OHSS.
In other studies, there were differences in stimulation strategies between the study arms which could serve as uncontrolled confounders [5, 6].
The use of GnRH antagonists in IVF is characterized by both advantages and disadvantages as prevention of premature LH increase and is easier and takes less time. GnRH antagonists act within a few hours after their administration, and thus, they can be administered only when there is a risk for an LH surge. This is in contrast to GnRH agonists where pituitary downregulation occurs only after 7–10 days [7].
Women with polycystic ovary syndrome are also at increased risk for developing ovarian hyperstimulation when aggressively stimulated with exogenous gonadotropins. Both agonists and antagonists can suppress elevated circulating LH concentrations, but the smaller follicular cohorts observed in antagonist cycles may help to reduce the risk of ovarian hyperstimulation in women with polycystic ovary syndrome who tend to be high responders [8].
Methods
Subjects and place
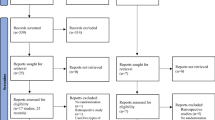
This study was carried out in the ART Unit of International Islamic Center of Population Studies and Research (IICPSR), Al-Azhar University, between August 2012 and September 2014. Data of 400 patients diagnosed with polycystic ovaries enrolled in the study was revised and reported.
Inclusion criteria
The following are the inclusion criteria:
-
1.
PCOS patients diagnosed according to Rotterdam and ASRM/ESHRE consensus criteria 2004, (presence of oligo/amenorrhea, clinical and or hormonal hyperandrogenism, and polycystic ovaries by ultrasound)
-
2.
Age between 20 and 35 years
-
3.
BMI < 30
-
4.
Basal levels of FSH and LH hormones ≤ 10 IU/ml
-
5.
Absence of pelvic pathology as endometriotic cysts, fibroids, and uterine abnormality such as a bicornuate uterus assessed by transvaginal ultrasound
Exclusion criteria
The exclusion criterion is patients in antagonist protocols who triggered by the agonist.
Statistical analysis
Package for Social Sciences (SPSS) for Windows version 20 (IBM, NY, USA) was used. Kolmogorov-Smirnov test for normality was applied to all measured variables. Student t test was used for the comparisons between quantitative variables; chi-square test was used for the comparisons between categorical variables. The sample size was estimated depending on α error = 5%, power of the study = 80%, and effect size that gave the minimally clinical effect using epi-info 7 software for the sample size calculation.
Methodology
Data file of a cohort of 400 PCOS patients was revised and subdivided into 2 equal groups according to the protocols prescribed: group 1 (n = 200) was stimulated by GnRH agonist long mid-luteal protocol, and group 2 (n = 200) was stimulated by fixed (day 7) antagonist protocol. In GnRH agonist long mid-luteal protocol (agonist group), triptorelin 0.1 mg (Decapeptyl 0.1, Ferring, Egypt) daily s.c. injection started on day 21 of the preceding cycle (3 days before the discontinuation of oral contraceptive pills (OCP) for 2 weeks), and complete downregulation was diagnosed if estimated E2 < 50 pg/ml. Then, recombinant FSH (rFSH), Gonal-F (follitropin b, Merck Serono, Egypt) s.c. injection was started at a dose of 150 IU/day (the dose was modified according to the response), and both the agonist and recombinant were continued until the day of triggering. In fixed GnRH antagonist protocol (antagonist group), rFSH was given starting from cycle day 2 in a dose of 150 IU daily (the dose was modified according to the response) to day 7 when antagonist (Cetrotide, cetrorelix 0.25 mg, Merck Serono, Egypt) s.c. daily injection was started, and both rFSH and antagonist were continued until the day of triggering. Coasting was decided in patients showing hyper response (> 15–20 follicles in each ovary and or E2 > 3500 pg/ml). As soon as three follicles with a mean diameter of ≥ 17 mm were reached, 5000 IU of HCG (Pregnyl, Organon, Netherlands) was administered i.m. once and 36 h before ovum pick up. Oocyte retrieval was performed assisted by transvaginal ultrasound-guided double-lumen needle aspiration. All embryos were transferred under abdominal ultrasound guidance. Luteal phase support with 400 mg of micronized progesterone (Utrogestan Laboratoires Besins-International S.A., France) was initiated for 14 days after the embryo transfer. Embryo transfer was canceled, and elective embryo cryopreservation was performed in cases of early OHSS detected 3 days post-oocyte retrieval that could possibly lead to life-threatening OHSS [9] or in cases fulfilling one or more of the criteria for hospitalization [10].The primary outcome measure was the incidence rate of OHSS. Secondary outcome measures were the clinical pregnancy rate (CPR), number of oocytes retrieved, number of embryos transferred, fertilization rate, cancelation rate, duration of stimulation, total dose of stimulation, and E2 concentration on the day of HCG administration. Clinical pregnancy is defined as the presence of gestational sac with fetal heartbeat detected in 6–7 weeks of gestation.
Discussion
Many studies had been shown the difference between long agonist and antagonist protocols for non-PCOS patients treated with IVF/ICSI. In the current study, we had tried to clarify the efficacy of two commonly used protocols prescribed for this category of patients (PCOS patients).
Polycystic ovary syndrome (PCOS) is the most common cause of oligo-ovulation and anovulation both in the general population and among women presenting with infertility [11], being a common endocrine disorder affecting 5–10% of women in reproductive age [12].
The long GnRH agonist (GnRH-a) protocol is a conventional protocol, probably the most widely used throughout the world even now, allows a quite good predictability of the work in IVF units, implies a low cancelation rate, and allows to get a relatively high number of pre-ovulatory follicles of retrieved oocytes and, as a consequence, of embryos available for transfer, thus leading to a satisfactory pregnancy rate [13].
The relatively recent introduction of GnRH antagonists in clinical practice has provided another option for ovarian stimulation in IVF [13].The introduction of GnRH antagonists (GnRH-ant) in assisted reproductive technologies (ART) to prevent LH surge seemed to open up a new way towards a more “friendly IVF.” Unlike the indirect pituitary suppression induced by GnRH-a, GnRH-ant administration causes immediate and dose-related inhibition of gonadotropin release by competitive occupancy of the GnRH receptors in the pituitary [14].
In the current study, the data of 400 PCOS patients were collected and revised. The patients included were distributed into 2 equal groups (group 1, received long mid-luteal agonist protocol; group 2, received fixed antagonist protocol). ICSI was performed for all patients, and the data collected was analyzed anonymously.
Nine cases in group 1 and seven cases in group 2 were canceled. The causes of cancelation in group 1 were empty follicles in three cases, failed fertilization in two cases, and early OHSS in four cases. The causes in group 2 were empty follicles in two cases, failed fertilization in four cases, and OHSS in one case (Table 1).
There were no significant differences between both groups in view of age, BMI, and basal hormone levels (Table 2).
There was a significant difference between the groups when comparing the means of the total dose of rFSH given (means ± SD, 1901.7 ± 400 vs. 1789.7 ± 368.6 with p = .004 in group 1 and group 2, respectively) (Table 2 and Fig. 1). This result was similar to the previous studies done on non-PCOS patients [15, 16] whereas some researchers have shown a significant reduction in the number of used HMG in non-PCOS patients [17, 18] and PCOs patients who underwent treatment with GnRH antagonist [19]. The lower dose required with antagonist treatment may be explained by the difference in the behavior of stimulation between the agonist and antagonist protocols in that with agonist stimulation, the complete downregulation required for starting treatment may provoke the depletion of endogenous FSH that may in turn requires augmentation of the gonadotrophin dosage. In antagonist protocol, stimulation with gonadotrophin started before giving antagonist when the levels of endogenous FSH still at the physiological levels that may support the given gonadotrophin, so lower doses were required.
In agreement with our results, many studies supported the finding of reduced stimulation dose in antagonist protocol if compared to agonist rendering ovarian stimulation less costly as in studies by Depalo et al. [7] and Johnston et al. [20].
There is a significant difference between both groups as regards the duration of stimulation by gonadotrophins where the mean ± SD is 11.3 ± 0.8 vs. 10.3 ± 1.1 with p = .017 for groups 1 and 2, respectively (Table 2 and Fig. 2). This result was similar to the result of two previous studies in non-PCOS patients [21, 22]. This also may be explained as mentioned above.
E2 levels estimated at hCG day are significantly different between both groups, i.e., lower levels are at the antagonist group (mean ± SD, 2672.3 ± 768.3 vs. 2528.7 ± 611.4 with p = .039) (Table 2 and Fig. 3).
There is no significant difference between the groups in view of the numbers of oocytes retrieved (mean ± SD, 18.7 ± 4.7 vs. 19.2 ± 3.9 with p = 0.267) (Table 3). The result of our study coincides with the results of the studies of Minaretzis et al. [16] and Hwang et al. [19] who stimulated PCOS patients for ICSI.
The fertilization rate (52% vs. 50% with p = .101) and pregnancy rate (37% vs. 32% with p = .125) for agonist and antagonist groups, respectively, were not significantly different (Table 3). These results were similar to the previous researches in non-PCOS [17, 18] and PCOS patients [19].
In our study, we used the clinical pregnancy rate (CPR) as the primary outcome because the CPR is achieved after ovarian stimulation and IVF represent very important outcome measures for any treatment protocol. There has been conflicting evidence in the literature regarding whether an antagonist protocol is as effective as the long agonist protocol with respect to the CPR and ongoing pregnancy rate (OPR). Significantly lower OPRs are observed in patients on fixed 6-day GnRH antagonist cycles [23].
The most recent review indicates that overall GnRH antagonists do not compromise the effectiveness and significantly prevent OHSS [3].
A meta-analysis of Haiyan et al. [24] included 9 RCTs with a total of 1142 women with PCOS and showed no significant difference between the antagonist and long agonist protocols with regard to CPR and OPR.
GnRH antagonist protocols came to be used more frequently in clinics in a wide range of patients, including patients with normal ovarian responses as well as patients with poor or high responses; this last group includes patients with PCOS.
All the above results are in agreement with those previously published by other contributors [18, 19, 25,26,27,28,29].
Previous studies have all agreed that the antagonist protocol is more patient-friendly and convenient [25, 30].
This convenience, added to the equal CPR compared to the agonist protocol, suggests that the antagonist protocol may be the most suitable stimulation regimen for PCOS patients.
A relatively recent RCT study done by Raffaella-Depalo et al. [31] and a retrospective cohort review by Johnston et al. [20] decided that GnRh antagonist is associated with a significantly lower incidence of grade II OHSS, requiring lower gonadotrophin amounts and a shorter duration of stimulation than GnRh agonist.
The role of an antagonist in the reduction of OHSS in PCOS patients may be attributed to the small follicular cohorts observed after exogenous stimulation. This is supported by a study of Fauser [8]. However, this proposal was not recorded in the current study.
There were significant differences between both groups in view of mild, moderate, and severe OHSS (15%, 6%, and 1% vs. 4.5%, 2.5%, and 0.55 with p = .04) in group 1 and group 2 (Table 4 and Fig. 4).
Our results are in agreement with the findings from previous studies in the general population [32, 33, 25]. These observations suggest that the use of GnRH antagonists in the treatment of patients with PCOS results in a safer way of performing ovarian stimulation for IVF.
It is not, however, clear that the difference in the rate of OHSS in the two groups was associated with the number of oocytes retrieved. Despite the similar number of oocytes retrieved in the two groups, it cannot be excluded the number of small follicles, which did not yield oocyte but contributed to the incidence of OHSS.
Women receiving antagonists have been shown to have a lower incidence of ovarian hyperstimulation syndrome (OHSS). Assuming comparable clinical outcomes for the antagonist and agonist protocols, these benefits would justify a change from the standard long agonist protocol to antagonist regimens [32].
It should also be noted that the dose of hCG used for triggering final oocyte maturation in the current study was 5000 IU. This choice was made in order to reduce the occurrence of OHSS in this high-risk population. Consequently, regarding OHSS occurrence, the conclusions drawn in the current study might not be applicable in patients with PCOS in whom 10,000 IU hCG is used for triggering final oocyte maturation.
Conclusion
GnRH antagonist may be soon the preferred protocol for PCOS patients treated with ICSI in view of the reduction of the risk of OHSS, the less cost-effectiveness, and the short stimulation time without compromising the pregnancy outcome.
Availability of data and materials
The data will not be shared because, it is the policy of our center.
Abbreviations
- CPR:
-
Clinical pregnancy rate
- GnRH:
-
Gonadotrophin-releasing hormone
- hCG:
-
Human chorionic gonadotrophin
- OHSS:
-
Ovarian hyperstimulation syndrome
- OPR:
-
Ongoing pregnancy rate
- PCOS:
-
Polycystic ovary syndrome
References
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group (2004) Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 81:19–25
Costello MF, Misso ML, Wong J, Teede HJ (2012) The treatment of infertility in polycystic ovary syndrome: a brief update. Aust N Z J Obstet Gynaecol 52(4):400–403
Al-Inany HG, Youssef MA, Ayeleke RO, Brown J, Lam WS, Broekmans FJ (2016) Gonadotrophin-releasing hormone antagonists for assisted reproductive technology. Cochrane Database Syst Rev (4):CD001750
Youssef MA, Van der Veen F, Al-Inany HG, Mochtar MH, Griesinger G, Nagi Mohesen M, Aboulfoutouh I, van Wely M (2014) Gonadotropin-releasing hormone agonist versus HCG for oocyte triggering in antagonist-assisted reproductive technology. Cochrane Database Syst Rev (10):CD008046
DiLuigi AJ, Engmann L, Schmidt DW, Benadiva CA, Nulsen JC (2011) A randomized trial of microdose leuprolide acetate protocol versus luteal phase ganirelix protocol in predicted poor responders. Fertil Steril 95:2531–2533
Revelli A, Chiadò A, Dalmasso P, Stabile V, Evangelista F, Basso G, Benedetto C (2014) ‘Mild’ vs. ‘long’ protocol for controlled ovarian hyperstimulation in patients with expected poor ovarian responsiveness undergoing in vitro fertilization (IVF): a large prospective randomized trial. J Assist Reprod Genet 31:809–815
Depalo R, Lorusso F, Palmisano M, Bassi E, Totaro I, Vacca M et al (2009) Follicular growth and oocyte maturation in GnRH agonist and antagonist protocols for in vitro fertilisation and embryo transfer. Gynecol Endocrinol. 25(5):328–334. https://doi.org/10.1080/09513590802617762
Fauser BC (2002) Publication of the results in all Dutch centers for in vitro fertilization: an important step towards an improvement in the effectiveness of the treatment. Ned Tijdschr Geneeskd 146(49):2335–2338
Navot D, Bergh P, Laufer N (1992) Ovarian hyperstimulation syndrome in novel reproductive technologies: prevention and treatment. Fertil Steril. 58:249–261
The Practical Committee of American Society of Reproductive Medicine (2004) Multiple pregnancy associated with infertility therapy. J Fertil Steril. 82.
Azziz R, Carmina E, Dewailly D (2006) Position statement: criteria for defining polycystic ovary syndrome as a predominantly hyperandrogenic syndrome: an Androgen Excess Society guideline. J Clin Endocrinol Metab. 91(11):4237–4245
Diamanti-Kandarakis E and Piperi C (2005): Genetics of polycystic ovary syndrome: searching for the way out of the labyrinth. Hum Reprod Update. 1.
Ye H, Huang G, Pei L (2008) A prospective, randomized controlled study comparing the effects of gonadotropin-releasing hormone agonist long and short protocols for in vitro fertilization. Zhonghua Fu Chan KeZaZhi 36(4):p222–p225
Olivennes F, Belaisch-Allart J, Emperaire JC, Dechaud H, Alvarez S, Moreau L (2000) Prospective, randomized, controlled study of in vitro fertilization-embryo transfer with a single dose of a luteinizing hormone-releasing hormone (LH-RH) antagonist (cetrorelix) or a depot formula of an LH-RH agonist (triptorelin). Fertil Steril 73(2):314–320
Barros Del Gadillo JC, Siebzehnrubl E, Dittrich R, Wildt L, Lang N (2002) Comparison of GnRH agonists and antagonistin unselected IVF/ICSI patients treated with different controlled ovarian hyperstimulation protocols: a matched study. Eur J Obstet Gynecol Reprod Biol 102(2):179–183
Minaretzis D, Alper MM, Oskowitz SP, Lobel SM, Mortola JF, Pavlou SN (1995) Gonadotropin-releasing hormone antagonist versus agonist administration in women undergoing controlled ovarian hyperstimulation: cycle performance and in vitro steroidogenesis of granulosa-lutein cells. Am J Obstet Gynecol 172(5):1518–1525
Albano C, Felberbaum RE, Smitz J, Riethmuller-Winzen H, Engel J, Diedrich K et al (2000) Ovarian stimulation with HMG: results of a prospective randomized phase Ш European study comparing the luteinizing hormone releasing hormone (LHRH)-antagonist cetrorelix and the LHRH-agonist buserelin. Hum Reprod 15(3):526–531
Hohmann FP, Macklon NS, Fauser BCJM (2003) A randomized comparison of two ovarian stimulation protocols with gonadotropin–releasing hormone (GnRH) antagonist cotreatment for in vitro fertilization commencing recombinant follicle-stimulating hormone on cycle day 2 or 5 with the standard long GnRH agonist protocol. J Clin Endocrinol Metab 88(1):166–173
Hwang JL, Seow KM, Lin YH, Huang LW, Hsieh BC, Tsai YL et al (2004) Ovarian stimulation by concomitant administration of cetrorelix acetate and HMG following Diane-35 pretreatment for patients with polycystic ovary syndrome: a prospective randomized study. Hum Reprod 19(9):1993–2000
EB J-MA, DiLuigi AJ, Engmann LL, Maier DB, Benadiva CA, Nulsen JC (2011) Selection of first in vitro fertilization cycle stimulation protocol for good prognosis patients: gonadotropin releasing hormone antagonist versus agonist protocols. J Reprod Med. 56(1–2):12–26
Fluker M, Grifo J, Leader A, Levy M, Meldrum D, Muasher SJ et al (2001) Efficacy and safety of ganirelix acetate Ashrafi et al. Iranian Journal of Reproductive Medicine Vol.3. No.118 versus leuprolide acetate in women undergoing controlled ovarian hyperstimulation. Fertil Steril 75(1):38–45
European and Middle East Orgalutran Study Group (2001) Comparable clinical outcome using the GnRH antagonist ganirelix or a long protocol of the GnRH agonist triptorelin for the prevention of premature LH surges in women undergoing ovarian stimulation. Hum Reprod 16(4):644–651
Kolibianakis EM, Zikopoulos K, Schiettecatte J, Smitz J, Tournaye H et al (2004) Profound LH suppression after GnRH antagonist administration is associated with a significantly higher ongoing pregnancy rate in IVF. Human Reproduction 1911:2490–2496
Lin H, Li Y, Li L, Wang W, Yang D, Zhang Q (2014) Is a GnRH antagonist protocol better in PCOS patients? A meta-analysis of RCTs. PLoS One. 9(3)
Lainas TG, Sfontouris IA, Zorzovilis IZ et al (2009) Management of severe OHSS by Gn RH antagonist and blastocyst cryopreservation in PCOS patients treated with long protocol. Reprod Biomed On line 18:15–20
Olivennes F, Cunha-Filho JS, Fanchin R, Bouchard P, Frydman R (2002) The use of GnRH antagonists in ovarian stimulation. Human Reprod Update 83:279–290
Ragni G, Vegetti W, Riccaboni A, Engl B, Brigante C, Crosignani PG (2005) Comparison of GnRH agonists and antagonists in assisted reproduction cycles of patients at high risk of ovarian hyperstimulation syndrome. Hum Reprod 20:2421–2425
Kobilianakis EM, Kalogreopoulou L, Griesinger G et al (2007) Among patients treated with FSH and GnRH analogues for in vitro fertilization, is the addition of recombinant LH associated with the probability of live birth? A systemic review and meta-analysis. Human Reprod Update 13(5):445–453
Kurzawa R, Ciepiela P, Baczkowski T, Safranow K, Brelik P (2008) Comparison of embryological and clinical outcome in GnRH antagonist vs. GnRH agonist protocols for in vitro fertilization in PCOS non-obese patients. A prospective randomized study. J Assist Reprod Genet. 25(8):365–374
Orvieto R, Meltcer S, Liberty G, Rabinson J, Anteby EY et al (2012) Does day-3 LH/FSH ratio influence in vitro fertilization outcome in PCOS patients undergoing controlled ovarian hyperstimulation with different GnRH-analogue? Gynecol Endocrinol 286:422–424
Depalo R, Jayakrishan K, Garruti G, Totaro I, Panzarino M, Giorgino F, Selvaggi LE (2012) GnRH agonist versus GnRH antagonist in in vitro fertilization and embryo transfer (IVF/ET). Reprod Biol Endocrinol 10:26
Al-Inany HG, Youssef MA, Aboulghar M, Broekmans F, Sterrenburg M, Smit J, Abou-Setta AM.(2011): Gonadotrophin-releasing hormone antagonists for assisted reproductive technology. Cochrane Database Syst Rev. May 11;(5):CD001750.
Aboulghar MA, Mansour RT, Amin YM, Al-Inany HG, Aboulghar MM, Serour GI (2007) A prospective randomized study comparing coasting with GnRH antagonist administration in patients at risk for severe OHSS. Reprod Biomed Online 15(3):271–279
Acknowledgements
Many thanks to embryology staff for thier support unil this work had finished.
Funding
No fund from any organization.
Author information
Authors and Affiliations
Contributions
BM contributed to the study design, data collection, and statistical analysis. EH contributed to the data collection. EA contributed to the writing of the review and data analysis. EA contributed to the writing of the review and final revision. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the University Medical Ethical Committee (registry number, GYN._199 Med.Research._0000199).
Consent for publication
All authors agreed for the publication at MEF journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Behery, M.A., Hasan, E.A., Ali, E.A. et al. Comparative study between agonist and antagonist protocols in PCOS patients undergoing ICSI: a cross-sectional study. Middle East Fertil Soc J 24, 2 (2020). https://doi.org/10.1186/s43043-019-0002-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43043-019-0002-1