Abstract
Background
Unsafe injection practices are an occupational hazard among the nursing staff. Awareness of nurses’ staff members about safe injection practices may vary between different hospitals according to the policies adopted for staff training and systematic auditing.
Aim
To assess awareness and practice of safe injection among nursing staff in a Maternal and Child Hospital, Qassim Region, Saudi Arabia, and Beni-Suef University Hospital, Egypt.
Methods
A cross-sectional study using a structured questionnaire. Observations included 500 injections (250 from each hospital) from October to December 2017.
Results
The mean awareness total scores in both hospitals were 9.98 ± 1.76 and 11.12 ± 0.96 respectively with a significant difference among observed nurses (P = 0.001). The mean safe injection practice total score was 27.13 ± 3.11 and 27.39 ± 2.17. Past year safe injection training was received for 95% and 70% for observed Egyptian and Saudi group of nurses. The majority of nurses (98.8%) were aware of the importance of safe injection practices to minimize blood-borne diseases, and 95.2% of them were aware of the placement of sharps disposal box beside the place of injection procedure. Exposure to the past year needlestick injuries (NSIs) was higher among the observed Egyptian nurses (P = 0.001). Using appropriately stored and refilled disinfectants was done by 48.5% and 51.5% of the observed nurses. Needle separation from its syringe inside sharps disposal box and sharps disposal boxes near patient care areas were observed in 95.2% and 95.6% of both hospitals respectively.
Conclusions and recommendation
Nurses of both hospitals have good awareness and practice of injection safety. This might be attributed to the adoption of appropriate training courses. There is a need for continuous training sessions and auditing for nursing staff to ensure safe injection practices.
Similar content being viewed by others
1 Introduction
Unsafe injection practices by healthcare providers pose a risk for patients and healthcare workers especially infectious and non-infectious adverse events and often are associated with a variety of improper procedures and unsafe settings.
Safe injection practices are a set of preventive measures aiming to optimally perform a safe patients’ injection manner; a “safe injection” should not harm the recipient, should avoid exposing the health care provider to any potential risk, and should not result in a hazardous waste for the community [1].
Four main potential risks might pose a direct patient hazard, namely re-use of injection equipment, where administration of about 16 billion injections are encountered worldwide with about 40% of which involves re-use of injection equipment [2]; accidental needlestick injuries (NSIs) for health care provider resulting in a total of 3 million accidental NSIs in a WHO survey [3]; overuse of injections, where various surveys conducted in different settings indicated a high (up to 56%) at least one injectable preparation was prescribed with an annual ratio of 1.7 to 11.3 injections per person per year [4]; and unsafe sharps waste disposal, where inappropriate collection and disposal of sharp wastes put the health care practitioner and the waste handler including the community at risk of sharps injuries with consequential blood-borne infections [5].
Safe injection practice is a component of standard precautions aimed at maintaining basic levels of patient safety and provider protections, which necessitates proper administration of an injection by a well-trained qualified healthcare provider under complete aseptic technique using a sterile device (syringe, needle, etc.) with its appropriate disposal in a puncture-proof sharps discard container [6, 7].
Proper injection equipment disposal is required not only to check the reuse of disposable syringes but also to minimize the opportunities of avoidable healthcare workers’ (HCWs) potential risks [8].
Improper syringe disposal and NSI incidents reflect that there is a wide gap between healthcare provider knowledge and their practice; therefore, injection-related behavioral changes are required that might be brought by continuous training and regular audit and supervision. After HCWs’ training as regards injection safety and waste management, behavior change and needle recapping were significantly reduced, and safety box use was increased [9].
Unsafe injection practices add to the global burden of blood-borne disease. This accounted for 14% of HIV, 25% HBV, 8% HCV, and 5% of bacterial infections worldwide and for 28 million preventable disabilities [10].
Lack of implementations of guidelines for safe injection practices and medical waste management may result in unsafe injection for healthcare providers as well as patients’ blood-borne risks. The aim of this study was to assess safe injection awareness and practices among nursing staff in an Egyptian and a Saudi hospital.
2 Materials and methods
2.1 Study design
The study design is a cross-sectional comparable design.
2.2 Study setting
The study was conducted in Beni-Suef University Hospital (BSUH), Beni-Suef, Egypt, and Maternal and Child Hospital (MCH), Qassim, Saudi Arabia, in the period from October to December 2017. The two settings were comparable where the study population included nursing staff of intensive care units, emergency departments, and inpatient wards.
2.3 Sample size
A convenient sample of 500 nurses was included in this study. A total of 258 nurses offering direct patient care out of 375 nurses accepted to participate from BSUH; 250 of them continued their participation in the study and 8 withdrew. As for the participating nurses from MCH, 250 out of 453 nurses participated in the study.
2.4 Sampling selection method
We tried hard to make the total population as we included all nurses who offered injection (258/375 were selected from the BSUH in Egypt and 250/453 were selected from the MCH-Qassim in Saudi Arabia).
During the study period, a single observation was carried out by the research team who visited the clinical departments of the hospital to observe injection practices of the nurses; while on duty, a subsequent personal interview was carried out to fill out a questionnaire aiming to assess their awareness as regards safe injection practices. A total of 500 injections were observed (250 from each hospital). A pilot study was done for 30 nurses in each of the selected hospital before the data collection to ensure the clarity and easy handling of the questions. Content validity was assessed by reviewing the literature. The reliability of the questionnaire was calculated using the test-retest method, and no statistical differences were found.
2.5 Tools of study
A structured questionnaire divided into 3 parts was used to assess awareness, practices of safe injection, and accidental NSIs and sharps disposal as follows:
-
Part 1: A 12-item questions to assess their awareness about injection safety. The score for each question was zero or one. Questions with a correct answer were assigned a score of one point and incorrect answers questions were assigned a score of zero point. The total score was classified as: Poor (zero to five), fair (six to eight), and good (nine to 12).
-
Part 2: A 31-item questions to explore nurses' reported practices concerning safety injection. The total score for this set of items ranged from zero to 31. Items that were correctly performed by the nurse were given a score of one point and observations of incorrect practices were given a score of zero point. The total score was classified as: poor (zero to 10), fair (11–20), and good (21–31). The tool used for observing nurses practices was as per World Health Organization (WHO) tool for the assessment of injection safety with some modifications.
-
Part 3: History of accidental NSIs and sharps disposal for observed study nurses was assessed by four item questions.
2.6 Statistical analysis
Data collected were coded and analyzed by the Statistical Package for Social Science (SPSS) version 20 (IBM, USA). Frequency distribution, percentage, and descriptive statistics including mean ± SD were calculated. Chi-square test was performed when indicated. P values of ≤ 0.05 were considered significant.
3 Results
A total of 500 nurse practitioners from the two hospitals participated in the study. For the BSUH participants, the mean nurse age was 33.51 ± 10.17 years, 89% were females, 62% were married, the mean years of experience was 9.8 ± 7.7, and 63.5% of them had a bachelor level of nursing education. The mean age of MCH-Qassim nurses was 32.47 ± 8.53 years, 99% of them were females, 87% of them were married with a mean year of experience of 9.2 ± 8.4, and 80.3% of them had a bachelor level of nursing education.
3.1 Methods of injections
Intravenous administration of medication was the commonest (42%) method of injection, followed by intravenous (IV) sample withdrawal (23.2%), intramuscular route (17.6%), and IV cannula insertion (17.2%). The most common method used for skin site disinfection before the injection was the single-use alcohol swab (87.4%), followed by cotton piece soaked by alcohol (12.3%), and only 0.2% used a cotton piece soaked with Betadine (Table 1).
3.1.1 Awareness about safe injection (12 items)
There was a statistically significant difference in favor of better awareness for 8 items including 2 items showing better training for safe injection practice and waste sorting among BSUH nursing staff members compared to only 3 items in favor for MCH-Qassim nursing members. Only the item shortage of syringe stock at any time during the past month showed no statistical significance (Table 2).
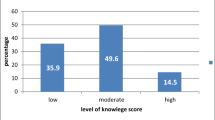
The comparison of the nurses in the two hospitals as regards the safe injection awareness score showed a higher mean total score of 11.12 ± 0.96 for BSUH compared to that of 9.98 ± 1.76 for MCH-Qassim (P < 0.001) (Table 3).
3.1.2 Safe injection practices (31 items)
There was a statistically significant difference in favor of better safe injection practice in 6 items for BSUH and MCH-Qassim nursing staff each. The observation of BSUH nursing staff members showed a higher percentage for intact needles mounted on its syringes inside sharps disposal box (97.6% vs 92.8%) for MCH-Qassim nursing members while for the item “washing hand or using alcohol hand rub before wearing gloves”, 78% and 92% of MCH-Qassim and BSUH nursing staff were observed to perform a correct hand hygiene practice (Table 4).
Comparing the 2 hospitals as regards the safe injection practices score revealed an almost equal mean total score of 27.39 ± 2.17 and 27.13 ± 3.11 respectively with no significant difference (Table 5).
Exposure to needle stick injury and needle disposal showed a significant difference between the two hospitals in favor of less exposure to NSI among MCH-Qassim nurses (5.6%) compared to the 32.4% among BSUH group of nurses, while only 75% of the MCH-Qassim nurses reported disposing the needles as a one unit compared to the 95% for the BSUH group of nurses reflecting better disposition of sharps/needles among the Egyptian group of study nurses (P = 0.001) (Table 6).
4 Discussion
The present study revealed high almost similar percentages (93.2–98%) of an implemented safe injection, infection control, and post-exposure needle stick injury policies and procedures in both hospitals, reflecting appropriate awareness as regards safe injection practice. These results are contrary to the results reported by a similar study in Gharbia, Egypt [11], and by an African study reporting that 62.1% of the respondents reported that such policies are not in existence in their hospitals [12].
In addition, higher safe injection (94.8%) and waste sorting (84.8%) training percentages were reported among the BSUH nursing staff compared to the MCH-Qassim training (70% for each category), reflecting a higher mean safe injection awareness score among the Egyptian participants. The present findings are similar to the reported 91% safe injection practice training in a Romanian study [13] and higher than that reported (27–33%) in Nepal, Ethiopia, and Bangladesh [14,15,16], reflecting the national interest of safe injection training practice among the current study hospitals.
Similarly, high awareness was reported among nurses in both study hospitals as regards measures to be taken after NSI (96% and 92.8%) and blood-borne diseases transmitted by unsafe injection practice (100% and 97.9%). These findings are similar to the reported 92.1% awareness of nurses for measures to be taken after NSI in West Bengal [17], higher than the reported 68% in Patiala, North India [18], and similar to the reported high percentage of awareness of blood-borne diseases transmitted by unsafe injection practice in India [19], West Bengal [17], and Nigeria [20].
Complete vaccination doses against hepatitis B among the 2 hospitals’ nursing study group showed a lower percentage among the MCH-Qassim (62.4%) participants compared to the BSUH (76%) participants. Higher rates were reported by other studies conducted in Nepal (76.8%) [14], Pokhara, Iran (82.3%) [21], Rawalpindi (82.7%) [22], and Karachi (73%) [23]. On the contrary, the vaccination coverage for both hospital groups of nurses was higher than that reported in two similar studies conducted in (52.2 and 21.1% .2% respectively) [24, 25]. Health care providers must be provided with full vaccination coverage for patients’ self-safety.
In this study, good awareness towards safe injection (92% and 99.2%) of the MCH-Qassim and BSUH nursing staff were reported. These rates are similar to the reported 90% good knowledge in a Nigerian study [26] but contrary to the low (37.7%) awareness score reported in Asaba, Nigeria [27], and the rate reported in Esan central LGA of Edo State, Nigeria [28].
Injection safety practices in both hospitals were satisfactory. Most of the observed nurses (95.6%) used new syringes and needles for each injection. These findings were consistent with the reported 95.7% new syringe and needle usage in a similar Egyptian study [11] and the 100% new syringe usage in a Romanian study [13] and higher than the reported 72% in another study in Nepal [14].
Safe injection practice was observed among nurses in this study with a minor difference between the 2 hospital groups. For the item safe injections are prepared on a clean tray, 94% and 79.2% of the observed nurses among MCH-Qassim and BSUH showed a correct practice respectively. A finding which is higher than a similar study conducted in SSKM Hospital, Kolkata, and West Bengal reported that 60% of the nursing personnel maintained the use of clean tray for safe injections [25].
As for the item washing hand or using alcohol hand rub before wearing gloves, 78% and 92% of the MCH-Qassim and the BSUH nursing staff were observed to perform a correct hand hygiene practice, percentages which are lower than the reported percentages in similar Nigerian (78.7%) [20] and Nepalese (63.2%) studies [14] and higher than the lower percentages reported in different studies for hand wash practices: 20% in Nigeria [29], 20% in Patiala [18], 12.5% in West Bengal [25], 4.6% in India [30], and 3.6% in a similar Egyptian study [11]. The discrepancy may be attributed to the higher international awareness and practice training for the hand hygiene practice in the recent years.
Of note, for the item needles separated from its syringe inside sharps disposal box, there was a statistically significant difference between the 2 hospital nursing groups, where 97.6% of needles were found not separated inside the sharps box in BSUH vs. 92.8% for the MCH-Qassim. In addition, for the item presence of sharps disposal box near patient care areas, it was observed to be present in 97.6% in BSUH and 93.6% in MCH-Qassim (P = 0.001). These findings reflect a better practice than that reported in a similar Nigerian study which revealed that 25% of nurses frequently leave sharps at the patient’s bedside [12].
Preparing patient’s skin in an appropriate aseptic method was higher in MCH-Qassim (97.6%) than in BSUH (86.8%). Similarly, 99.03% of injections were prepared clean using aseptic precautions in a study conducted in India [19].
In the current study, a high score of safe injection practice among nurses of the 2 study hospitals was reported (97.6% and 98%). This finding is contrary to the reported low percentage (40 to 61.4% from North to West India) of safe injection practice [31, 32]. The good awareness and safe injection practices among the 2 hospital study nurses in the present study may be due to implementation of universal standard infection control practices in the Egyptian and Saudi Arabian nursing curriculum and the continuous professional training programs.
Nurses who have experienced needle stick injury in the past 12 months before the study constituted 5.6% among the MCH-Qassim nurses compared to 32.4% among the BSUH group of nurses. These findings are lower than that reported in a Nigerian study with a NSI of 15.8% [20] when compared with the MCH-Qassim group of nurses while higher for the BSUH-Egypt ones. In addition, NSI among both study groups are far less than that reported in other studies: 67.6% and 40.4%, in the 2 hospitals in Ibadan, Nigeria [12], and 50% in India [33]. This disagreement might reflect the national interest in both countries towards safe injection training practice among the current study hospitals and positive attitude and appropriate implementation of safe injection policy and procedures.
In this study, the practice of two-handed recapping of needles after use and disposal in sharps box or disposal in non-medical waste constituted very low percentage in both hospitals (0.8% and 0.4%, respectively). Findings which are far below than that reported (71.4%) in a similar Egyptian series [11] and in other developing countries reported percentages of 9.05 to 17% in two Indian studies [19, 34], 11% in Pakistan [35], 19.1% in Nigeria [20], and 58% in Cambodia [36].
4.1 Limitations of the study
It is a single hospital questionnaire-based observational study in each country aimed to describe the pattern of safe injection practices among nurses. A single observation might not reflect the regular practice of nurses. There is a possibility of bias as healthcare providers may alter their behavior when they know that they are being observed. The possibility of bias is very high in the reported needlestick injuries; the main reasons stated for not reporting were time constraint and low perceived risk of disease transmission due to incident. This study did not aim for the consequent management of NSIs for the participants.
5 Conclusions and recommendations
Awareness and practice of injection safety were found to be good among nurses of BSUH, Egypt, and MCH, Qassim, Saudi Arabian. Appropriate training courses were implemented for the observed group of nurses. Continuous health care professional development for infection control and safe injection practice should be encouraged. Early preventive intervention and reporting of NSIs to hospital administration should also be an essential part of injection safety. Frequent infection control auditing is mandatory to ensure safe injection practices.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Change history
25 February 2020
Following publication of the original article [1], we have been notified that one of the authors��� given names is not reflected correctly.
Abbreviations
- BSUH:
-
Beni-Suef University Hospital
- IV:
-
Intravenous
- MCH:
-
Maternal and Child Hospital
- NSIs:
-
Needlestick injuries
- SPSS:
-
Statistical Package for Social Science
References
Injection Safety Aide Memoire, WHO 2002- guidelines. Available on the Internet at http://www.injectionsafety.org. SIGN toolbox (1.1).
Hauri A, Armstrong G, Hutin Y. The global burden of disease attributable to contaminated injections given in health care settings. Int J STD AIDS. 2004;15(1):7–16.
Pruss-Ustun A, Rapiti E, Hutin Y. Sharps injuries: global burden of disease from sharps injuries to health care workers. Environmental burden of disease series N° 3, WHO 2003.
Hutin YJ, Hauri AM, Armstrong GL. Use of injections in healthcare settings worldwide, 2000: literature review and regional estimates. BMJ. 2003;327(7423):1075.
World Health Organization (WHO) best practices for injections and related procedures toolkit. March 2010. WHO/EHT/10.02 ISBN 978 92 4 159925 2. Available at https://apps.who.int/iris/bitstream/handle/10665/44298/9789241599252_eng.pdf;jsessionid=0DB0C5CCD2A5D71190B064DFE5DA4F45?sequence=1.
World Health Organization (WHO): Question & Answers, Safety of injections. http://apps.who.int/medicinedocs/documents/s15276e/s15276e.pdf. Question and Answers Injection Safety.pdf (Accessed 18 Mar 2018).
Central for Disease Control and Prevention (CDC). Injection Safety. Available at https://www.cdc.gov/injectionsafety/ip07_standardprecaution.html. Accessed Feb 2019.
World Health Organization (WHO): Revised injection assessment tool (tool Crevised). Geneva: Geneva, Switzerland; 2008. Available at https://www.who.int/infection-prevention/tools/injections/ToolC-revised.pdf
Mantel C, Khamassi S, Baradel K, Nasri H, Mohsni E, Duclos P. Improved safety after targeted interventions in the Syrian Arab Republic. Tropical Med Int Health. 2007;12:422–30.
Reid S. Preliminary results of the WHO GBD from unsafe injections [abstract]. In: Report on Annual Meeting of the Safe Injection Global Network, 9-11 November 2010, Dubai, United Arab Emirate. Geneva: World Health Organization; 2010. who.int/injection_safety/sign/en/.
Ismail NA, Aboul Ftouh AM, EL-Shoubary WH, Mahaba H. Safe injection practice among health care workers in Gharbia Governorate, Egypt. East Mediterr Health J. 2007;13(4):893–906.
Adejumo PO, Dada FA. A comparative study on knowledge, attitude, and practice of injection safety among nurses in two hospitals in Ibadan, Nigeria. Int J Infect Control. 2013;9(1):1–6.
Chisevescu P, Mihailescu I, Mihailescu GP, Pasat L, Ion-Nedelcu N, Popa MI. Injection practices among nurses--Valcea Romania 1998. MMWR Morb Mortal Wkly Rep. 2001;50(4):59–61.
Hari PK, Shanti P, Sudarshan S, Neena G, Varidmala J, Parvati P. Awareness and practices on injection safety among nurses working in hospitals of Pokhara. Nepal Int J Med Health Sci. 2014;3(4):301–7.
Aderaw Z. Assessment on magnitude of needle stick and sharp injuries and associated factors among health care workers in East Gojjam zone health institutions, Amahara Regional State, Ethiopia. Glob J Med Res. 2013;13(3):41–9.
Chowdhury AKA, Roy T, Faroque ABM, Bachar SC, Asaduzzaman M, Nasrin N, et al. A comprehensive situation assessment of injection practices in primary health care hospitals in Bangladesh. BMC Public Health. 2011;11(779):1–13.
Joardar GK, Chatterjee C, Sadhukhan SK, Chakraborty M, Das P, Mandal A. Needle sticks injury among nurses involved in patient care: a study in two medical college hospitals of West Bengal. Indian J Public Health. 2008;52(3):150–2.
Kaur R, Kaur P, Lal P. Adherence to universal work precautions: a study among nurses and laboratory technicians in a teaching hospital of North India. J Commun Dis. 2010;42(2):161–3.
Mehta DR, Pillai A, Singh AP. An observational study of safe injection practices in a tertiary care teaching hospital. Int J Appl Res. 2016;2(5):733–7.
Ijachi OO, Audu O, Araoye M. Knowledge, attitude and practice of injection safety among Benue State University Teaching Hospital healthcare professionals. J Community Med Prim Health Care. 2016;28(2):26–33.
Gurung NS, Paudel K, Pun CB. Needle stick injuries among health care workers in a tertiary care teaching hospital, Pokhara, Nepal. J Gandaki Med Col. 2010;3(1):47–50.
Siddique K, Anil S, Shoaib SF, Anwar’s IA. Knowledge attitude and practices regarding needle stick injuries amongst healthcare providers. Pak J Surg. 2008;24(8):243–8.
Aslam M, Taj T, Ali A, Mirza W, Ali H, Dar MI, Badar N. Needle Stick Injuries Among Health Care Workers of Public Sector Tertiary Care Hospitals of Karachi. J Coll Physicians Surg Pak. 2010;20(3):150–3.
Omar AA, Abdo NM, Salama MF, Al-Mousa HH. Occupational injuries prone to infectious risks amongst healthcare personnel in Kuwait: a retrospective study Med Princ Pract. 2015;24(2):123–8.
Bobby P, Sima R, Dipankar C, Sukamol B, Raghunath M, Nabanita B, Biswajit B. A study on safe injection practices of nursing personnel in a tertiary care hospital of Kolkata, West Bengal, India. TAF Prev Med Bull. 2011;10(6):681–6.
Abdulraheem IS, Amodu MO, Saka MJ, Bolarinwa OA, Knowledge UMMB. Awareness and compliance with standard precautions among health workers in North Eastearn Nigeria. J Community Med Health Edu. 2012;2:131.
Isara AR, Ofili AN. Knowledge and practice of standard precautions among health care workers in the Federal Medical Centre, Asaba, Delta state, Nigeria. Niger Postgrad Med J. 2010;17(3):204–9.
Alice TE, Akhere AD, Ikponwonsa O, Grace E. Knowledge and practice of infection control among health workers in a tertiary hospital in Edo state, Nigeria. Direct Res J Health Pharmacol (DRJHP). 2013;1(2):20–7.
Bolarinwa OA, Salaudeen AG, Aderibigbe SA, Musa OI, Akande TM, Bamidele JO. Injection safety practices among primary health care workers in Ilorin, Kwara state of Nigeria. HSJ. 2012;6(3):496–507.
Rehana HS, Deepti C, Ravinder SK, Tanuj C, Arpit A, Sharmac GK. Injection practices of healthcare professionals in a tertiary care hospital. J Infect Public Health. 2012;5:177–81.
Kermode M, Jolley D, Langkham B, Thomas MS, Holmes W, Giffod SM. Compliance with universal/standard precautions among health care workers in rural north India. Am J Infect Control. 2005;33(1):27–33.
Vaz K, McGrowder D, Alexander-Linda R, Gordon L, Brown P, Irving R. Knowledge, attitude and compliance with universal precautions among health care workers at the university hospital of West Indies, Jamaica. Int J Occup Environ Med. 2010;1(4):171–81.
Muralidhar S, Singh PK, Jain RK, Malhotra M, Bala M. Needlestick injuries among health care workers in a tertiary care hospital of India. Indian J Med Res. 2010;131:405–10.
Pandit NB, Choudhary SK. Unsafe injection practices in Gujarat, India. Singap Med J. 2008;49(11):936–9.
Zafar A, Aslam N, Nasir N, Meraj R, Mehraj V. Knowledge, attitudes and practices of health care workers regarding needle stick injuries at a tertiary care hospital in Pakistan. J Pak Med Assoc. 2008;58(2):57–60.
Vong S, Perz JF, Sok S, Som S, Goldstein S, Hutin Y, Tulloch J. Rapid assessment of injection practices in Cambodia, 2002. BMC Public Health. 2005;5:56. https://doi.org/10.1186/1471-2458-5-56.
Acknowledgements
The authors would like to thank all the participants who helped us in this study.
Patients’ rights
Patients (or their caregiver) in the patient care areas were informed about the observation for their attending nurse, the benefit (improvement of safe injection is to be achieved through research) of this study was fully explained to them, and there are no potential risks with no effect on the medical care received.
Funding
There was no source of funding.
Author information
Authors and Affiliations
Contributions
MA and ML conceived and designed the study and finalized the methodology and tools used. MA, ML, and AA collected the data and analyzed and drafted the manuscript. All the authors made significant contributions in the manuscript writing and finalizing of the manuscript. The final manuscript has been read and approved by all the authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of the Faculty of Medicine, Beni-Suef University (FBBSU-REC). Necessary administrative approval was obtained from the directors of both health facilities included in the study. A written informed consent was obtained from the participants including filling a questionnaire addressing their awareness about safe injection practices and unexpected observation for the injection practices by a study team member. Study objectives and procedures were explained in detail to each participant and it was clearly explained to them that the results would only be used for research. Participation in the study was voluntary. The investigators ensured the anonymous identity of study participants and data were kept protected to ensure confidentiality and privacy of information.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Anwar, M.M., Mohamed Lotfy, A.A. & Alrashidy, A.A. Safe injection awareness and practices among nursing staff in an Egyptian and a Saudi hospital. J. Egypt. Public. Health. Assoc. 94, 21 (2019). https://doi.org/10.1186/s42506-019-0018-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42506-019-0018-5