Abstract
Background
Postoperative delirium (PD) is an acute, transient disorder of consciousness, attention, perception, and cognition. Many theories, such as decreased cholinergic neurotransmission and surgery-induced disturbances in melatonin secretion, were proposed as a potential cause for developing PD especially in the elderly.
Previous studies concluded that perioperative rivastigmine significantly reduced the prevalence and severity of PD. Other studies concluded that oral perioperative melatonin was associated with a lower risk of PD. However, the effect of melatonin in patch form was not studied and the effect of perioperative rivastigmine and melatonin patch was not compared.
Our aim was to compare rivastigmine patch to melatonin patch regarding the incidence and severity of PD in elderly patients undergoing major orthopaedic surgery.
Methods
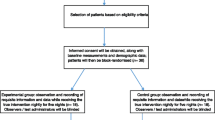
In this double blinded randomized study, 180 elderly patients, ASA I–III, aged 60–85 years undergoing major orthopaedic surgery were divided into two equal groups; group R patients received a rivastigmine patch (4.6 mg) and group M patients received a melatonin patch (7 mg). Both patches were administered 24 h preoperative, on the day of operation and for the following 3 postoperative days. All patients received regional anaesthesia and basic monitoring in the form of NIBP, SPO2, and ECG. Patients were examined for PD using the Confusion Assessment Method (CAM) and level of sedation using the Ramsay Sedation Score (RSS) on the first, second, third, and 7th postoperative day, and for those who develop PD, a CAM-S score was done to assess the severity of PD. Drug-related side effects were recorded. Statistical analyses were performed using a standard SPSS software.
Results
CAM score was positive in a total of 39 patients. Rivastigmine patch significantly decreased the incidence of PD when compared to melatonin patch (P value 0.047). However, CAM-S indicated that the severity of PD was comparable. Patients were more sedated in the melatonin group. There were no melatonin- nor rivastigmine-related perioperative complications. Intraoperative SBP, DBP, and HR were slightly less in melatonin group, although statistically non-significant.
Conclusions
Rivastigmine patch is superior to melatonin patch in decreasing the incidence of PD in elderly patients undergoing major orthopaedic surgery; however, both drugs were comparable in decreasing its severity.
Trial registration
Clinical trails.gov, NCT04189666. December 6, 2019, prospectively registered
Similar content being viewed by others
Introduction
Postoperative delirium (PD) is a typical, extreme sickness of the central nervous system uniquely among hospitalized older individuals and is characterized as an intense, transient issue of consciousness, perception, attention, and cognition which occurs over a brief timeframe and will in general vary throughout the attack (Inouye et al. 1999; Rabe-Jabłońska and Bieńkiewicz 1994).
Different variables may lead to the development of PD including contamination, ageing, surgical procedure, drug for example opiates, duration of opiate administration, preoperative comorbidity, or postoperative disturbance caused by drains, pain sensation, and sleep disorders (Zhang et al. 2015).
Old patients who experience major orthopaedic procedures usually suffer prolonged operative time, serious trauma, and occasionally an intensive care unit stay after surgery, which may increase the incidence of PD. Besides, owing to many other factors, the elderly are vulnerable as they are more susceptible to decreased cerebral blood flow and decreased perceptive ability. Development of PD may cause long-term cognitive impairment or even permanent dementia which increases the incidence of postoperative complications, mortality rates, prolonging hospital stay, and costs (Skrobik 2011; Guo et al. 2016).
The pathogenesis of PD in old patients is confusing. Numerous speculations were proposed; however, the specific pathogenesis of PD is as still ambiguous. Some studies suggested that surgery-induced disturbances in melatonin and cortisol secretion may be involved in the occurrence of PD (Guo et al. 2016; Kazmierski et al. 2014). Also, Wu et al. linked the development of PD to fluctuations in melatonin levels (Wu et al. 2014), while others attributed the development of PD to disturbance in cholinergic neurotransmission and cholinergic deficits (Hshieh et al. 2008).
Management of PD depends mainly on prevention strategies through minimizing the risk factors that tends to develop PD. Guo et al. introduced a multicomponent non-pharmacological methodology known as the Hospital Elder Life Program (HELP) that provides reassuring comfortable environment that ensures effective communication and reorientation. Medications are considered the second line of treatment, and although no specific drug is currently approved for the treatment of delirium, still, various medications were introduced to provide symptomatic relief among these melatonin and cholinergic enhancer (CE) were studied (Guo et al. 2016).
Melatonin (N-acetyl-5-methoxytryptamine) is a neurohormone that is discharged by the pineal gland produced from the amino acid tryptophan. Synthetic melatonin has been effectively utilized in the treatment of sleep disorders and jet lag. It was likewise utilized as a premedication and it provided excellent anxiolysis, sedation, and sympatholytic impacts with the merit of not influencing the patients’ cognition in addition to its analgesic effect. Moreover, a previous study concluded that preoperative administration of melatonin decreased the incidence of PD in addition to having a curative effect on patients who developed PD when used for three postoperative nights (Sultan 2010).
Rivastigmine is an acetyl cholinesterase inhibitor (AChEI) that expands the levels of acetylcholine in the synaptic cleft that stimulates the acetylcholine receptors. It is effectively utilized in the treatment of Alzheimer’s disease and other dementias. And owing to its mechanism of action, it was used in the prevention of delirium by promoting the cholinergic system (Massoud and Gauthier 2010). Previous studies found that using a rivastigmine patch in elderly with cognitive impairment decreased the incidence of PD (Youn et al. 2017).
So, both drugs (rivastigmine and melatonin) were proved successful in decreasing the incidence of PD. However, to our knowledge, melatonin was not studied in the patch form and the effect of both drugs on the severity of PD if developed is not evident. In this prospective, randomized, double-blind study, we compared melatonin patch to rivastigmine patch regarding the incidence and severity of postoperative delirium (PD) in elderly undergoing major orthopaedic surgery.
Patients and methods
We included 180 elderly patients ASA (American Society of Anaesthesiologists) physical, status I–III, and aged 60–85 years old undergoing major orthopaedic surgery (fracture pelvis, hip arthroplasty, total knee and hip replacement) in this study after approval of institution medical ethical committee FMASU R58/2019 and an informed written consent was taken from patients or their authorized relative.
The exclusion criteria are as follows:
-
History of neurological diseases, such as brain insult and stroke; mental disease; and dementia
-
Metabolic disorders and electrolyte disturbances
-
Alcohol dependence or drug abuse;
-
Secondary surgery or infectious complications
-
Severe sensory deficiency causing communication difficulty (deafness or blindness) and illiteracy.
-
CNS medications (antipsychotics, anticonvulsants, antiparkinsonian, antidepressants)
The day prior to the operation, all patients were examined by an anaesthesia resident “who was blinded to the study” for preoperative cognitive impairment using the Confusion Assessment Method (CAM) (Inouye et al. 1990). The CAM scores assess delirium rapidly and accurately, and also differentiates delirium from other cognitive impairment with sensitivity of 94–100% and specificity 90–95%. It is an algorithm that consists of four features: (i) acute and fluctuating variation in mental status, (ii) inattention, (iii) incoherent or disorganized thinking, and (iv) altered level of consciousness.
CAM scores indicate delirium if the first two features are present and either third or fourth feature is present. Patients with delirium were excluded from the study.
The 180 patients were randomly divided into two equal groups (90 patients each) using a computer-generated program. The rivastigmine and melatonin patches were given to the ward nurse who was blinded to the study and administered it to the patient 24 h preoperatively, on the morning of the operation and then every day postoperatively for the following 3 successive days.
In group R, 90 patients received a rivastigmine patch (4.6 mg) (EXELON® PATCH 5 4.6 mg/24 h transdermal patch, NOVARTIS) 24 h before the operation, on the morning of the operation, and then every day postoperatively for 3 successive days.
In group M, 90 patients received a melatonin patch (7 mg) (Melatonin Sleep Patch 7 mg, RESPR ABORATORIES) 24 h before the operation, on the morning of the operation, and then every day postoperatively for 3 successive days.
On the day of the operation, patients did not receive premedication. In the operating room basic monitoring in the form of non-invasive blood pressure (NIBP), systolic blood pressure (SBP), diastolic blood pressure (DBP), pulse oxygen saturation (SPO2), and electrocardiogram (ECG) were attached and recorded every 30 min. Level of intraoperative sedation was monitored using the Ramsay Sedation Scale (RSS) (Ramsay et al. 1974). The RSS consists of 6 points: score 1, patient is anxious and/or restless; 2, orientated, cooperative, and calm; 3, responding to orders; 4, quick response to stimulus; 5, slow response to stimulus; and 6, not responding to stimulus.
Patients of both groups received regional anaesthesia, in the form of spinal or epidural anaesthesia according to anaesthesia and surgical team preference and according to each case. Patients were put in the sitting position, the back was sterilized by povidone-iodine, drapes covered the back of the patient, L4-L5 or L3-L4 level was palpated, and local anaesthetic in the form of 1 ml of 2% lidocaine was injected subcutaneously.
In case of spinal anaesthesia, a spinal needle G25 was introduced. After appearance of CSF, heavy Marcaine was injected intrathecally. In case of epidural anaesthesia, a Tuohy needle was introduced; on feeling loss of resistance, a catheter was threaded upward; secured in place, a test dose of 3 ml 2% lidocaine was injected; and then, 12–18 ml of 0.5% isobaric Marcaine was injected.
After completing the surgery, patients were monitored. Basic monitoring in the form of (NIBP, SPO2, and ECG) every 6 h and any abnormality was recorded and managed accordingly. All patients were examined by the same anaesthesia resident “who was blinded to the study” for PD using Confusion Assessment Method (CAM) and level of sedation using RSS on the first, second, third, and 7th postoperative day and for those who develop PD, a CAM-S score (Inouye et al. 2014) was done to assess the severity of PD. CAM-S score which consists of 10 items, including acute onset and/or fluctuating course, inattention, disorganized thinking, altered consciousness, disorientation, deterioration of memory, disorder in perception, psychomotor agitation/retardation, and changes in sleep-wake cycle.
And patients with delirium were followed up and managed properly by a neurology specialist. Patients in the two groups were compared regarding incidence and severity of delirium on postoperative days 1, 2, 3, and 7.
Our primary outcome was to compare the two groups regarding the incidence of developing PD among the elderly patients. The secondary outcome was to compare between both groups regarding the severity of PD and level of sedation.
The endpoint of this study was occurrence of severe infectious complications, secondary surgery or severe metabolic and electrolyte disturbances, development of extrapyramidal symptoms and those patients were excluded from the study.
Ethical committee
FMASU R58/2019
Clinical trial number
NCT04189666
Sample size
Using STATA program, setting alpha error at 5% and power at 80%, results from previous study (11) showed that the incidence of PD in rivastigmine patch group was 16.1% of cases, while it is assumed to be 3% in melatonin patch group
Based on this, 80 cases per group were needed and raised to 90 per group (total 180) to take into account a 10% dropout rate.
Statistical analysis
All statistical analyses were performed using a standard SPSS software package (SPSS statistics for windows version 20 SPSS Inc., Chicago, IL, USA). Student’s t test was used to analyse parametric data, which were expressed as mean ± SD (compare between two groups in quantitative data). Categorical variables were analysed using the χ2 test and were expressed as number and percentage of patients. Data not normally distributed were compared using Mann-Whitney test and were presented as median (IQR). P values < 0.05 were considered statistically significant.
Result
Baseline patient characteristics and the duration of the operation were comparable between the study groups (Table 1).
Intraoperative SBP, DBP, and heart rate (HR) were slightly less in patients who received melatonin, but it was statistically non-significant when compared to those who received rivastigmine patch. While intraoperative SPO2 (97–100) % was comparable between the two groups (Table 2).
During the following 3 postoperative days, the haemodynamic parameters were comparable in both groups but for mean DBP that was slightly less in melatonin group although statistically non-significant (Table 3).
Confusion Assessment Method (CAM) score was positive in a total of 39 patients. There was a significant difference in the incidence of PD between the two groups where 25 patients in the melatonin group and 14 patients in the rivastigmine group (P value 0.047) developed PD (Fig. 1).
Eleven patients in melatonin group and 7 patients in rivastigmine group developed PD on the first postoperative day, while 10 patients in the melatonin group and 5 patients in rivastigmine group developed PD on the second postoperative day, 4 patients in melatonin group, and 2 in the rivastigmine group developed PD on the third postoperative day, while no more patients developed PD afterwards till the 7th day postoperative (Table 4, Fig. 2).
Confusion Assessment Method-S (CAM-S) done in 39 patients only 25 in group M and 14 in group R indicates that the severity of PD delirium in both groups was comparable (Table 5).
Patients were more sedated in the melatonin group during the first second and third postoperative days (Table 6).
There were no melatonin-related side effects as headache, dizziness, drowsiness, nausea, nor rivastigmine-related perioperative complications, including skin eruptions, pneumonia, wound infections, extrapyramidal symptoms, or gastrointestinal trouble.
Discussion
In the current study, we compared between rivastigmine and melatonin patch regarding their ability to decrease the incidence and severity of PD in elderly patients undergoing major orthopaedic surgery, so 180 elderly patients were randomly divided into two groups 90 patients each where group R received rivastigmine patch (4.6 mg) and group M received melatonin patch (7 mg). Either patch was administered 24 h before the operation, on the morning of the operation, and then every day postoperatively for 3 successive days.
We found that postoperative delirium occurred in 25 patients, 27.8% in the melatonin group and 14 patients 15.6% in the rivastigmine group (p = 0.047). The mean severity of delirium in the two groups as determined by the CAM-S was decreased in both groups with no significant difference (p = 0.477), and that reflects the ability of both drugs to decrease the incidence and severity of PD in elderly patients undergoing major orthopaedic surgery. However, it was obvious that rivastigmine patch achieved a significant reduction in the incidence of developing PD even more than melatonin patch.
We also noticed that patients were more sedated in the melatonin group during the first, second, and third postoperative day which we attribute to both the sedative and analgesic effects of melatonin. Also, owing to its sedative and analgesic effects, melatonin can reduce the consumption of other sedative drugs and opioid analgesics, which is possibly the cause of decreased severity of delirium in the melatonin group.
In this study, we used the patch form in order to ensure blindness of the patient and health care givers to the drug used. Moreover, the patch form has the advantage of being easily applied, escapes drug first-pass metabolism, and thus provides high bioavailability and long duration of action which increases patient’s compliance.
Previous study concluded that cholinergic enhancers (CE) such as rivastigmine can be used to diminish the occurrence of PD (Yoon et al. 2017). Another study added that it may also diminish the severity of PD (Youn et al. 2017). However, others found that rivastigmine and other CE did not add any benefit regarding the incidence nor the severity of PD (Sampson et al. 2007; Liptzin et al. 2005; Gamberini et al. 2009). Regarding melatonin, previous studies showed that it decreased the incidence of PD and can, as well, be used in treating PD (Guo et al. 2016; Sultan 2010). However, all these studies used the oral form of melatonin and to our knowledge none has compared the effectiveness of both drugs on PD.
Our study revealed that application of rivastigmine patch preoperative and for 3 successive days postoperative decreased the incidence of PD (15.6%) as well as decreased its severity (CAM-S range 7–10, Median = 9, IQR = 1.5). This was in consistence with the results reached by Youn et al. who found that rivastigmine patch significantly reduced the prevalence (16.1%) and severity of PD (Youn et al. 2017). However, Yoon et al. in a meta-analysis stated that CE decreased the risk of PD through enhancing central cholinergic transmission but it did not affect the severity of the delirium (Yoon et al. 2017). This difference may be because of variable types of the CE used in the included studies with variable duration of treatment.
Contrary to our study, other studies claimed that CE did not affect the incidence of PD and that may be due to the difference in the methodology and population included in these studies, e.g., Sampson et al. (Sampson et al. 2007) administered the CE for 3 successive days postoperatively with no preoperative or intraoperative dose as in our study. Liptzin et al. (Liptzin et al. 2005), also was unable to demonstrate a benefit for CE in preventing or treating delirium in a relatively young and cognitively intact elderly patients who had low incidence to develop PD. Also, Gamberini et al. (Gamberini et al. 2009) did not support prophylactic administration of oral rivastigmine in preventing PD in cognitively intact elderly patients experiencing elective cardiac surgery with cardiopulmonary bypass.
Jackson et al. revealed that rivastigmine had no impact on delirium incidence or duration. However, they included cognitively intact elderly patients (Jackson et al. 2017).
Our study did not reveal any rivastigmine-related complications such as skin eruptions, pneumonia, wound infections, extrapyramidal side effects, and gastrointestinal upset. This can be due to the small dose of 4.6 mg used in this study. This result was different from that reached by Van Eijk et al. (Van Eijk et al. 2010) who ended their study due to increased mortality in the rivastigmine group but this may be due to the increasing dose of rivastigmine they used in critically ill patients.
During the study, there was no significant difference between the two groups regarding intraoperative and postoperative haemodynamics although systolic and diastolic blood pressure was slightly lower in the melatonin group. This could be related to the antihypertensive effect of melatonin. This antihypertensive effect was demonstrated by Mohamed et al. and Gupta et al. who concluded that melatonin premedication can effectively reduce the stress responses to laryngoscopy and intubation (Mohamed et al. 2013; Gupta et al. 2016).
The blood pressure-lowering effect of melatonin is either directly through increasing nitric oxide that causes dilatation of arterial smooth muscles (Simko and Paulis 2007) or through binding to melatonin receptors in the blood vessels decreasing its response to circulating catecholamines (Wan et al. 1999) or through melatonin receptors in the brain, decreasing central adrenergic outflow (Anwar et al. 2001) in addition to its sedative and analgesic effect.
We also observed slight non-significant intraoperative reduction in the heart rate in patients receiving melatonin patch. This finding can be explained by the sedative, anxiolytic, and analgesic actions of melatonin. This reduction in HR was also observed by Mohamed et al. and Gupta et al. (Mohamed et al. 2013; Gupta et al. 2016).
Limitations
One of the limitations of the study is that we did not add a control group for better comparison of the effect of both drugs, so we could not assess decrease in severity. Moreover, we did not evaluate other PD-associated risk factors besides preoperative cognitive level. We did not assess the implementation of multidisciplinary intervention programme run by an in-hospital care team in addition to the medical treatment in decreasing the incidence of PD and this may require further studies.
Conclusion
Rivastigmine patch was superior to melatonin patch in decreasing the incidence of PD in elderly patients undergoing major orthopaedic surgery. However, both drugs were comparable in decreasing its severity.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- PD:
-
Postoperative delirium
- ASA:
-
American Society of Anaesthesiologists
- NIBP:
-
Non-invasive blood pressure
- SPO2 :
-
Pulse oxygen saturation
- ECG:
-
Electrocardiogram
- CAM:
-
Confusion Assessment Method
- RSS:
-
Ramsay Sedation Score
- CAM-S score:
-
Confusion Assessment Method-Severity
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- HR:
-
Heart rate
- HELP:
-
Hospital Elder Life Program
- CE:
-
Cholinergic enhance
- AChEI:
-
Acetyl cholinesterase inhibitor
- CSF:
-
Cerebrospinal fluid
References
Anwar MM, Meki AR, Rahma HH (2001) Inhibitory effects of melatonin on vascular reactivity: possible role of vasoactive mediators. Comp Biochem Physiol C Toxicol Pharmacol 130:357–367
Gamberini M, Bolliger D, Lurati Buse GA et al (2009) Rivastigmine for the prevention of postoperative delirium in elderly patients undergoing elective cardiac surgery-a randomized controlled trial. Crit Care Med 37:1762–1768
Guo Y, Sunb L, Lic L, Jiaa P, Zhanga J, Jiangb H, Jianga W (2016) Impact of multicomponent, nonpharmacologic interventions on perioperative cortisol and melatonin levels and postoperative delirium in elderly oral cancer patients. Arch Gerontol Geriatr 62:112–117
Gupta, P., Jethava, D., Choudhary, R. and Jethava, D. (2016). Role of melatonin in attenuation of haemodynamic responses to laryngoscopy and intubation. Indian Journal of Anaesthesia, 60(10), p.712.
Hshieh TT, Fong TG, Marcantonio ER, Inouye SK (2008) Cholinergic deficiency hypothesis in delirium: a synthesis of current evidence. J Gerontol A Biol Sci Med Sci 63:764–772
Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI (1990) Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 113(12):941–948
Inouye SK, Schlesinger M, Lydon TJ (1999) Delirium: a symptom of how hospital care is failing older persons and a window to improve quality of hospital care. Am J Med 106:565–573
Inouye SK, Kosar CM, Tommet D, Schmitt EM, Puelle MR, Saczynski JS, Jones RN (2014) The CAM-S: development and validation of a new scoring system for delirium severity in 2 cohorts. Ann Intern Med 160(8):526–533
Jackson TA, Moorey HC, Sheehan B, Maclullich AM, Gladman JR, Lord JM (2017) Acetylcholinesterase activity measurement and clinical features of delirium. Dement Geriatr Cogn Disord 43(1-2):29–37. https://doi.org/10.1159/000452832
Kazmierski J, Banys A, Latek J, Bourke J, Jaszewski R, Sobow T et al (2014) Mild cognitive impairment with associated inflammatory and cortisol alterations as independent risk factor for postoperative delirium. Dement Geriatr Cogn Disord 38:65–78
Liptzin B, Laki A, Garb JL, Fingeroth R, Krushell R (2005) Donepezil in the prevention and treatment of post-surgical delirium. Am J Geriatr Psychiatry 13(12):1100–1106
Massoud F, Gauthier S (2010) Update on the pharmacological treatment of Alzheimer’s disease. Curr Neuro pharmacol 8:69–80
Mohamed AA, Atef HM, El Kassaby AM, Ismail SA, Helmy AM (2013) Effects of melatonin premedication on the hemodynamic responses and perfusion index during laryngoscopy and endotracheal intubation. Med J Cairo Univ 81:859-67. www.medicaljournalofcairouniversity.net. (n.d.). medical journal cairo university. [online] Available at: http://www.medicaljournalofcairouniversity.net/ [].
Rabe-Jabłońska J, Bieńkiewicz W. [Anxiety disorders in the fourth edition of the classification of mental disorders prepared by the American Psychiatric Association: diagnostic and statistical manual of mental disorders (DMS-IV) -- options book] Psychiatr Pol. 1994 Mar-Apr;28(2) 255-268. PMID: 8208869.
Ramsay M, Savege TM, Simpson ER, Goodwin R (1974) Controlled sedation with aphaxalone-alphadolone. Br Med J 2:656–659
Sampson EL, Raven PR, Ndhlovu PN, Vallance A, Garlick N, Watts J et al (2007) A randomized, double-blind, placebo-controlled trial of donepezil hydrochloride (Aricept) for reducing the incidence of postoperative delirium after elective total hip replacement. Int J Geriatr Psychiatry 22:343–349. https://doi.org/10.1002/gps.1679
Simko F, Paulis L (2007) Melatonin as a potential antihypertensive treatment. J Pineal Res 42:319–322
Skrobik Y (2011) Delirium prevention and treatment. Anesthesiol Clin 29:721–727
Sultan SS (2010) Assessment of role of perioperative melatonin in prevention and treatment of postoperative delirium after hip arthroplasty under spinal anaesthesia in the elderly. Saudi J Anaesth 4:169–172. https://doi.org/10.4103/1658-354X.71132
Van Eijk MM, RoesKC, Honing ML, Kuiper MA, Karakus A, van der Jagt M,E et al. (2010) Effect of rivastigmine as an adjunct to usual care with haloperidol on duration of delirium and mortality in critically ill patients: a multicentre, double-blind, placebo-controlled randomised trial. Lancet 376:1829-1837.
Wan Q, Man HY, Liu F, Braunton J, Niznik HB, Pang SF et al (1999) Differential modulation of GABA A receptor function by Mel1a and Mel1b receptors. Nat Neurosci 2:401–403
Wu Y, Wang J, Wu A, Yue Y (2014) Do fluctuations in endogenous melatonin levels predict the occurrence of postoperative cognitive dysfunction (POCD)? Int J Neurosci 124(11):787–791
Yoon BH, Yoo JI, Youn YC, Ha YC (2017) Cholinergic enhancers for preventing postoperative delirium among elderly patients after hip fracture surgery: a meta-analysis. European Geriatric Medicine 8:486–491
Youn YC, Shin HW, Choi BS, Kim SY, Lee JY, Ha YC (2017) Rivastigmine patch reduces the incidence of postoperative delirium in older patients with cognitive impairment. Int J Geriatr Psychiatry 32:1079–1084
Zhang WY, Wu WL, Gu JJ, Sun Y, Ye XF, Qiu WJ et al (2015) Risk factors for postoperative delirium in patients after coronary artery bypass grafting: a prospective cohort study. J Crit Care 30:606–612
Acknowledgements
Not applicable
Funding
There was no external funding
Author information
Authors and Affiliations
Contributions
R M proposed the idea and study design and was a major contributor in writing the manuscript. A A analysed and interpreted the patient data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval and consent to participate were approved by Faculty of Medicine—Ain Shams University Ethical committee, FMASU R58/2019. Clinical trial number is NCT04189666. An informed written consent was taken from patients or their authorized relative.
Consent for publication
“Not applicable”
Competing interests
The authors declare that they have no competing interests
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Rivastigmine and Melatonin Patches used in the study.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hussien, R.M., Shoukry, A.A. Rivastigmine patch (Exelon patch) compared to melatonin patch in prevention of postoperative delirium in the elderly. Ain-Shams J Anesthesiol 12, 37 (2020). https://doi.org/10.1186/s42077-020-00087-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s42077-020-00087-6