Abstract
Background
Meningitis is a life-threatening infection often associated with high morbidity. Recurrent bacterial meningitis poses a clinical challenge, both clinically and diagnostically. To prevent further recurrences, the underlying causes of recurrent bacterial meningitis should be investigated intensively.
Case presentation
Here, we aim to present a patient referred to our clinic with rhinorrhea and found to the Staphylococcus aureus meningitis related to a clival defect. The patient reported no history of trauma, surgery, or brain neoplasm, and the cerebrospinal fluid leakage was classified as spontaneous. The patient had two episodes of meningitis in the last 4 years, but etiologic data of the previous episodes were absent. A pneumococcal vaccine was administered following her second attack, suggesting a possible Staphylococcus aureus infection due to altered colonization in the sinuses. She was successfully treated with linezolid but refused surgery to correct the defect and was discharged without neurologic sequelae.
Conclusion
Spontaneous cerebrospinal fluid leakage from the clivus which could provoke recurrent meningitis is a rare situation. In conjunction with appropriate rapid antibiotherapy for the prevention of recurrent meningitis, the removal of anatomical risk factors should be a principal aim. Effective surgical procedures prevent recurrences.
Similar content being viewed by others
Background
Recurrent bacterial meningitis is defined as either two or more episodes of meningitis caused by a different bacterial organism or a second or subsequent episode caused by the same organism with a greater than 3-week interval following the completion of the initial therapy [1]. The causes of underlying anatomic, immunologic, or chronic parameningeal infections need to be investigated intensively to prevent further recurrence. The clivus is found in the deepest region of the skull base with one of its walls adjacent to the top of the sphenoid sinus. Cerebrospinal fluid (CSF) leakage from the clivus could lead to recurrent meningitis. In this report, we have discussed this rare anatomic defect and etiologic differentiation in a patient with recurrent bacterial meningitis in conjunction with relevant reported adult cases from the literature.
Case presentation
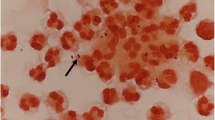
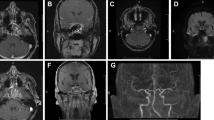
A 64-year-old female was admitted to the emergency room with headache, nausea, and vomiting. Medical history revealed two meningitis episodes: the first being 4 years and the second 2 years previously. Medical data concerning these episodes were absent, but she had been successfully treated with intravenous antibiotics. She was vaccinated with 23-Valent Pneumococcal Polysaccharide Vaccine (PPSV23) following the second meningitis attack. She declared no head trauma, surgery, malignancy, or sinus and ear infections. Beta-lactam allergy was confirmed. Her temperature was 38.3 °C, and she was conscious and oriented. No signs of meningeal irritation were detected, and other system examinations were normal. Her white blood cell (WBC) count was 12,300/mm3 and C-reactive protein level was 1.3 mg/dl (< 0.5, normal reference). Lumbar puncture revealed elevated opening pressure, cloudy appearance of CSF with 1856 WBC (90% polymorph), CSF glucose was 29 mg/dl (serum glucose was 112 mg/dl), and CSF protein was 98.4 mg/dl. CSF Gram stain showed the appearance of Gram-positive cocci in clusters. Linezolid 2 × 600 mg was started due to the beta-lactam allergy with the diagnosis of acute bacterial meningitis. Methicillin-sensitive Staphylococcus aureus was isolated in CSF culture. Her immune system tests were normal. Computed tomography and magnetic resonance imaging of the skull base revealed irregular millimetric bone defects at the clivus (Fig. 1) and excessive pneumatization of the sphenoid bone posteriorly (Fig. 2). A CSF leak was located in the posterior part of the clivus. Rhinorrhea was questioned and confirmed with β-2 transferrin analysis. Surgery was offered to repair the clival defect, but she rejected any surgical interventions. After 2 weeks of linezolid treatment, the patient was discharged without neurologic sequelae. Her 6-month follow-up showed no further sign of meningitis.
Discussion
Our patient has experienced three episodes of meningitis over the last 4 years. The predisposing factor appears to be spontaneous CSF leakage (S-CSF-L) at the posterior part of the clivus. This was based on no other definable history, such as trauma, surgery, or brain neoplasm. The definite cause of S-CSF-L remains elusive. Most cases, however, do have increased intracranial pressure [2]. Pneumatization of the sphenoid bone in conjunction with functional factors, such as the increased intracranial hypertension, continuous erosive effect of CSF and pulsative arteries, and/or other congenital developmental factors, are likely associated with spontaneous CSF leaks [2, 3].
The prevalence of S-CSF-L of all CSF fistulas in any location is between 3 and 40% in the series [4,5,6,7]. S-CSF-L is usually observed at the cribriform plate of the skull base. Sphenoidal and, more specifically, clival localization is even less common [3]. S-CSF-L from the clivus is very rare, with few cases reported in the literature [6, 7]. Meningitis is the most serious clinic complication in these cases.
CSF leakage due to primary defects and/or fracture of the clivus, or osteomyelitis of the clivus might lead to meningitis and recurrent meningitis [5,6,7,8,9,10,11,12,13]. Table 1 summarizes the published characteristics of meningitis cases that include clivus defects. Because of the localization, fractures of the clivus are very rare and defined in only one case [10]. The common feature of all cases, except the one with the clivus osteomyelitis, is that patients present with rhinorrhea prior to meningitis. The preferred surgical procedure to repair the leak is endoscopic endonasal transsphenoidal surgery. No recurrence of the leak or meningitis has been reported following this type of surgery.
In the cases where clival defect was eventually found, the reasons outlined for the recurrences included a failure to give surgical consent following the first episode [5], ineffective first surgery [7], inappropriate antibiotherapy course for osteomyelitis [8], and misidentification of the exact leak site [9]. It is our understanding that the patient discussed herein was misdiagnosed following previous episodes. After the diagnosis of clival defect, however, she declined the surgery. A strict follow-up procedure must be mandated in such cases.
Streptococcus pneumoniae, Gemella haemolysans, Hemophilus influenzae, and Neisseria meningitis have all been reported in specific cases. However, in several other cases, the microorganism was not mentioned. With the exception of postoperative meningitis, S. aureus in bacterial meningitis is rarely found [14, 15]. In the majority of cases, S. aureus reaches the meninges via bacteremia from a non-cranium source, such as endocarditis, epidural abscess, and skin or soft tissue infections. Direct contagious spread from a colonized skull bone in the presence of CSF leakage is unusual. Some case reports have cited S. aureus in the etiology of recurrent bacterial meningitis. The risk factors in these cases include ventriculoperitoneal shunts and dermal sinus tract resulting from epidermoid cyst [16, 17].
Neither of these risk factors was identified in our case. However, the administration of PPSV23 to our patient following her second episode can be described as a risk factor due to the altering of colonization in the sinuses. Some studies have also shown that the nasopharyngeal carriage of S. aureus is increased following the widespread usage of the pneumococcal vaccine [18, 19]. It could be noted that increases in the relatively rare microorganism of meningitis might arise from vaccinations for the more common bacterial agents.
Conclusion
S-CSF-L from the clivus is a rare condition that can cause recurrent meningitis. With the presence of rhinorrhea, detailed radiological imaging should be performed to detect possible CSF leak. Following the administration of an appropriate agent-specific antibiotherapy and the stabilization of the patient, removal of anatomic risk factors should be considered to prevent recurrences. To date, the endoscopic endonasal approach presents the most effective option.
Availability of data and materials
Please contact the corresponding author for additional data and images.
Abbreviations
- CSF:
-
Cerebrospinal fluid
- EET:
-
Endoscopic endonasal transsphenoidal surgery
- F:
-
Female
- G. haemolysans :
-
Gemella haemolysans
- H. influenzae :
-
Haemophilus influenzae
- M:
-
Male
- N. meningitidis :
-
Neisseria meningitidis
- PPSV23:
-
23-Valent Pneumococcal Polysaccharide Vaccine
- S. aureus :
-
Staphylococcus aureus
- S. pneumoniae :
-
Streptococcus pneumoniae
- S-CSF-L:
-
Spontaneous cerebrospinal fluid leakage
- SRTR:
-
Sublabial rhinoseptal transsphenoidal repair
- WBC:
-
White blood cell
References
Tebruegge M, Curtis N. Epidemiology, etiology, pathogenesis, and diagnosis of recurrent bacterial meningitis. Clin Microbiol Rev. 2008;21(3):519–37.
Van Zele T, Kitice A, Vellutini E, Balsalobre L, Stamm A. Primary spontaneous cerebrospinal fluid leaks located at the clivus. Allergy Rhinol (Providence). 2013;4(2):e100–4.
Pagella F, Pusateri A, Matti E, Zoia C, Benazzo M, Gaetani P, et al. Endoscopic management of spontaneous clival cerebrospinal fluid leaks: case series and literature review. World Neurosurg. 2016;86:470–7.
Loew F, Pertuiset B, Chaumier EE, Jaksche H. Traumatic, spontaneous and postoperative CSF rhinorrhea. Adv Tech Stand Neurosurg. 1984;11:169–207.
Oleś K, Składzien J, Betlej M, Chrzan R, Mika J. Spontaneous cerebrospinal fluid leak at the clivus. Wideochir Inne Tech Maloinwazyjne. 2015;10(4):593–9.
Codina Aroca A, Gras Cabrerizo JR, De Juan DM, Massegur SH. Spontaneous cerebrospinal fluid fistula in the clivus. Eur Ann Otorhinolaryngol Head Neck Dis. 2017;134(6):431–4.
Asad S, Peters-Willke J, Brennan W, Asad S. Clival defect with primary CSF rhinorrhea: a very rare presentation with challenging management. World Neurosurg. 2017;106:1052.e1–4.
Hayashi T, Uchiumi H, Yanagisawa K, Ogawa Y, Handa H, Tsukamoto N, et al. Recurrent Gemella haemolysans meningitis in a patient with osteomyelitis of the clivus. Intern Med. 2013;52(18):2145–7.
Tandon V, Garg K, Suri A, Garg A. Clival defect causing primary spontaneous rhinorrhea. Asian J Neurosurg. 2017;12(2):328–30.
Tohge R, Takahashi M. Cerebrospinal fluid rhinorrhea and subsequent bacterial meningitis due to an atypical clival fracture. Intern Med. 2017;56(14):1911–4.
Coiteiro D, Távora L, Antunes JL. Spontaneous cerebrospinal fluid fistula through the ClivusReport of two cases. Neurosurgery. 1995;37(4):826–8.
Ahmad FU, Sharma BS, Garg A, Chandra PS. Primary spontaneous CSF rhinorrhea through the clivus: possible etiopathology. J Clin Neurosci. 2008;15(11):1304–8.
Ramos A, García-Uría J, Ley L, Saucedo G. Transclival cerebrospinal fluid fistula in a patient with Marfan’s syndrome. Acta Neurochir. 2007;149(7):723–5 discussion 725.
Aguilar J, Urday-Cornejo V, Donabedian S, Perri M, Tibbetts R, Zervos M. Staphylococcus aureus meningitis: case series and literature review. Medicine (Baltimore). 2010;89(2):117–25.
Pintado V, Meseguer MA, Fortún J, Cobo J, Navas E, Quereda C, et al. Clinical study of 44 cases of Staphylococcus aureus meningitis. Eur J Clin Microbiol Infect Dis. 2002;21(12):864–8.
Cherian A, Baheti NN, Easwar HV, Nair DS, Iype T. Recurrent meningitis due to epidermoid. J Pediatr Neurosci. 2012;7(1):47–8.
Spanu T, Romano L, D’Inzeo T, Masucci L, Albanese A, Papacci F, et al. Recurrent ventriculoperitoneal shunt infection caused by small-colony variants of Staphylococcus aureus. Clin Infect Dis. 2005;41(5):e48–52.
Devine VT, Jefferies JM, Clarke SC, Faust SN. Nasopharyngeal bacterial carriage in the conjugate vaccine era with a focus on pneumococci. J Immunol Res. 2015;2015:394368.
Ebruke C, Dione MM, Walter B, Worwui A, Adegbola RA, Roca A, et al. High genetic diversity of Staphylococcus aureus strains colonising the nasopharynx of Gambian villagers before widespread use of pneumococcal conjugate vaccines. BMC Microbiol. 2016;16:38.
Acknowledgements
Not applicable.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
ANE and RE were involved in giving care to the patient and wrote the manuscript. BB interpreted the images and contributed to the diagnosis. FA developed the primary concept and designed the manuscript. HV supervised the authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
A written informed consent was obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Emecen, A.N., Ertekin, R., Baysal, B. et al. Clival defect in the pathogenesis of recurrent meningitis: a case report and literature review. Egypt J Neurosurg 34, 36 (2019). https://doi.org/10.1186/s41984-019-0066-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-019-0066-3