Abstract
Background
Pneumocephalus is a common complication presented as air in the cranial cavity after cranial surgery. We present a very rare case of isolated new onset aphasia due to pneumocephalus after evacuation of subdural hematoma (SDH). Tension pneumocephalus presenting as isolated aphasia has not been reported earlier although associated paresis has been reported.
Case presentation
We present the case of a 13-year-old male child with a history of fall before the onset of symptoms like headache and vomiting. The immediate MRI of the brain showed left-sided frontotemporoparietal subacute SDH with significant midline shift and subfalcine herniation. The child was subsequently managed with craniotomy and evacuation of hematoma with duraplasty. The patient developed aphasia on second-day post-surgery which progressed from moderate to severe aphasia by day 4. Computed tomography (CT) scan revealed pneumocephalus and an increase in the pneumocephalus in imaging on post-op day 4 with no other abnormalities. The condition was then managed by removing the subgaleal drain and administering high flow oxygen of 10 l/min.
Conclusion
This case signifies the importance of proper diagnosis of new-onset neurological deficits after evacuation of subdural hematoma for the better outcome.
Similar content being viewed by others
Background
Pneumocephalus is a clinical condition presented by air or gas in the intracranial cavity and is usually associated with cranial trauma or surgery [1, 2]. Computed tomography (CT) usually confirms the diagnosis with frontal pneumocephalus being most common followed by post-op neurosurgeries [3]. Pneumocephalus can be typed as acute (< 72 h) or delayed (> 72 h) [5, 6]. Based on the clinical features, pneumocephalus can be differentiated into simple and tension pneumocephalus and the distinction between them is of clinical importance as the latter constitutes as a neurosurgical emergency [4]. Symptoms of tension pneumocephalus may range from headache and dizziness to severe neurological manifestations like hemiparesis. [4]. We present a case of isolated new onset aphasia due to tension pneumocephalus after evacuation of subdural hematoma (SDH). Tension pneumocephalus presenting as an isolated aphasia that has not been reported ever, although associated with paresis, has been reported.
Case presentation
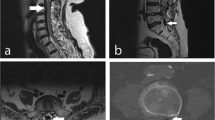
A 13-year-old male child presented 6 h after a fall while playing at school. He complained of a dull aching type of global headache and a radiating pain in the neck. The patient had non-projectile vomiting two to three episodes per day and aggravated headache. Magnetic resonance imaging (MRI) of the brain at emergency (ER) when he presented showed left-sided frontotemporoparietal (FTP) SDH with significant midline shift and subfalcine herniation. The patient was managed with craniotomy and evacuation of hematoma with duraplasty. No breach in frontal sinus was found (Fig. 1).
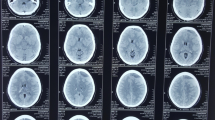
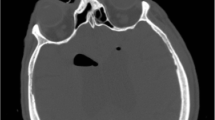
The patient was then extubated and the immediate post-op period was uneventful (Fig. 2a) Immediate post-op was showing left frontal small pneumocephalus with no residual hematoma. The patient developed moderate aphasia (Aphasia Handicap Scale (AHS) = 2) on post-op day 2. It was pure motor aphasia with reduced fluency and articulation; comprehension was intact and not associated with any limb paresis. Complaints gradually progressed over the next 2 days to severe aphasia (Aphasia Handicap Scale (AHS) = 4) [1]. CT scan revealed an increase in pneumocephalus with mass effect (Fig. 2b).
Literature suggests the use of normobaric high flow oxygen of 5–12 l/min [2, 3] through a simple O2 mask, and in our case, we used 10 l/min which is commonly practiced in our institute and the subgaleal drain was also blocked and subsequently removed. Patient aphasia improved completely over the next few days.
Discussion
It is a common practice to place epidural or subgaleal drains after craniotomies so as to prevent intracranial and extracranial blood collection [10]. Effective hemostasis and adequate watertight closure of the dura may not necessitate the placement of vacuum drains. Even after proper care taken during the closure, still, pneumocephalus is a common finding postoperatively, though tension pneumocephalus is rare. Pneumocephalus which is common after the evacuation of subdural hematoma can be confirmed with immediate postoperative CT imaging, which usually gets absorbed within a few days.
Dabdoub et al. and Gore et al. termed pneumocephalus and tension pneumocephalus [2, 3]. Pneumocephalus is usually found in the epidural, subarachnoid, intraventricular, intracerebral, and subdural spaces of trauma patients and post-op patients [9]. Tension pneumocephalus is a variant in which air is collected in the subdural space under pressure, and it is a common practice to place epidural or subgaleal drains less than atmospheric pressure probably due to a ball valve-like mechanism. Tension pneumocephalus causes pressure effects and might cause symptoms like lightheadedness, nausea, headache, vomiting, seizures, and hemiparesis [3, 4].
There are instances reporting aphasia, hemiparesis, and cranial nerve compression symptoms. The left hemisphere controls the analytical and language function. In the patients who are right-handed, we could expect that their left hemisphere would be dominant; as a result, language impairment is observed in them. Broca’s area present in the frontal lobe of the dominant hemisphere is usually the left side. The compression of motor neurons present in this area causes aphasia [7, 8]. The CT scan of our patient showed an accumulation of air and compression in the frontal region on the left, explaining this patient’s transient aphasia.
The percentage of oxygen in the atmospheric air is 21%. The normal partial pressure of oxygen (PO2) within the brain tissue ranges from 25 to 36 mmHg. The diffusion of O2 into the brain tissue in case of pneumocephalus is usually large. The brain tissue and blood show higher oxygen content due to its high solubility, and as a result, rapid absorption of oxygen is seen for maintaining the partial pressure within the pneumocephalus, the same as in the surrounding tissue [3].
As per Gore et al. predictions, in regard to the absorption of intracranial air, the rate of pneumocephalus absorption and FiO2 concentration should always be equal and the rate of absorption should be regulated as per the size of the pneumocephalus [3].
Conclusion
Tension pneumocephalus causing hemiparesis and aphasia though rare have been reported, but isolated aphasia due to tension pneumocephalus has not been reported. This case signifies the importance of proper diagnosis of new-onset neurological deficits after the evacuation of subdural hematoma and management with high flow oxygen and proper placement of collecting chamber at the level of the patient’s tragus to allow continuous drainage and for the better outcome.
Abbreviations
- AHS:
-
Aphasia Handicap Scale
- CT:
-
Computed tomography
- ER:
-
Emergency
- FTP:
-
Frontotemporoparietal
- MRI:
-
Magnetic resonance imaging
- SDH:
-
Subdural hematoma
References
Azuar C, Leger A, Arbizu C, Henry-Amar F, Chomel-Guillaume S, Samson Y. The aphasia rapid test: an NIHSS-like aphasia test. J Neurol. 2013;260:2110–7.
Dabdoub CB, Salas G, Silveira EN, Dabdoub CF. Review of the management of pneumocephalus. Surg Neurol Int. 2015;6:155.
Gore PA, Maan H, Chang S, Pitt AM, Spetzler RF, Nakaji P. Normobaric oxygen therapy strategies in the treatment of postcraniotomy pneumocephalus. J Neurosurg. 2008;108:926–9.
Ihab Z. Pneumocephalus after surgical evacuation of chronic subdural hematoma: is it a serious complication? Asian J Neuro. 2012;7(2):66–74.
Kankane VK, Gupta TK. Outcome of posttraumatic delayed intracerebral tension pneumatocele: prospective study of four cases: single institutional experience. Asian J Neuro. 2018;13(4):1087–95.
Marupudi NI, Mittal M, Mittal S. Delayed pneumocephalus-induced cranial neuropathy. Case Rep Med. 2013;2013:1–5.
Mehesry TH, Shaikh N, Duthie DJR, Malmstrom MF, Marcus AE, Khan A. Aphasia and upper limb weakness reversed by reabsorption of pneumocephalus. Trauma Acute Care. 2016;1(1):9.
Mortimer R, Owens E, Howlett DC. An unusual case of aphasia. BMJ. 2017;357:j2792.
Reddi S, Honchar H, Robbins MS. Pneumocephalus associated with epidural and spinal anesthesia for labor. Neurol Clin Pract. 2015;5:376–82.
Yadav M, Nikhar SA, Kulkarni DK, Gopinath R. Cardiac arrest after connecting negative pressure to the subgaleal drain during craniotomy closure. Case Rep Anesthesiol. 2014;2014:3.
Acknowledgments
We wish to thank our colleagues and radiologist (Dr Sandeep Kumar Nandamuri) from Star hospitals for helping us with the study.
Funding
No funds received
Availability of data and materials
Not applicable
Author information
Authors and Affiliations
Contributions
VKC assisted in the surgery and management of treatment, in the collection and compiling of data, and in the writing of the manuscript. JA contributed to the collection and compiling of the data and wrote, reviewed, and corrected the manuscript. GSC assisted in the surgery and management of treatment. NKP reviewed and corrected the manuscript. BRSCY assisted in the surgery and management of treatment. SS reviewed and corrected the manuscript. SS performed the surgery and reviewed and corrected the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Informed written consent for this information to be published was signed by patients parent.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Chagalakonda, V., Adulla, J., Chamle, G.S. et al. A very rare case of isolated aphasia due to tension pneumocephalus after subdural hematoma (SDH) evacuation: a case presentation. Egypt J Neurosurg 34, 15 (2019). https://doi.org/10.1186/s41984-019-0037-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41984-019-0037-8