Abstract
Background
Clinically isolated syndrome (CIS) is the first neurologic episode of multiple sclerosis (MS). Clinical presentation, neurophysiological studies, and magnetic resonance imaging (MRI) are used to predict risk of conversion to MS. There is little information regarding the risk factors of CIS conversion to MS so far in the Egyptian patients. This study aimed to evaluate the predictors of early conversion of the Egyptian patients with CIS to MS.
Methods
A longitudinal prospective study was conducted on 43 Egyptian patients diagnosed as CIS according to the McDonald criteria (2010). The CIS patients underwent clinical assessment of disability using Expanded Disability Status Scale(EDSS), brain imaging by magnetic resonance imaging (MRI), and visual evoked potential (VEP) at baseline and after 1-year follow-up.
Results
Eight patients (19.6%) with CIS converted to clinically definite MS after 1 year. A logistic regression analysis revealed that the CIS patients with initial clinical presentation with optic neuritis and higher MRI brain lesion number were associated with early conversion to MS (p = 0.003, p = 0.002, respectively). The total MRI brain T2 lesion number that predicts early conversion to MS was four lesions with sensitivity (100%) and specificity (85.7%).
Conclusions
The patients with CIS that early presented with optic neuritis and higher MRI brain lesion number are at higher risk for conversion to clinically definite MS.
Similar content being viewed by others
Background
Clinically isolated syndrome (CIS) refers to a monophasic clinical episode with patient-reported symptoms and objective findings reflecting a focal or multifocal inflammatory demyelinating event in the central nervous system (CNS), developing acutely or sub acutely, with a duration of at least 24 h, with or without recovery, and in the absence of fever or infection, similar to a typical multiple sclerosis relapse (attack and exacerbation) but in a patient not known to have multiple sclerosis (Thompson et al. 2018).
A number of risk factors for conversion to clinically definite MS (CDMS) have been studied, including demographic characteristics, MRI lesions, cerebrospinal fluid (CSF) oligoclonal bands, and more recently vitamin D levels (Kuhle et al. 2015).
Many experts recommended the initiation of a disease-modifying therapy after the initial demyelinating event particularly in patients at high risk for subsequent attacks rather than waiting for dissemination in time based on MRI or clinical outcomes (Frohman et al. 2006). The common problem in early treatment of those patients is that it is difficult to predict which individuals are most at risk for early relapse. It was suggested that early relapse is predictive of worse long-term outcomes (Weinshenker et al. 1989; Amato et al. 1999). To our knowledge, the early predictors for conversion to clinically definite MS in patients with CIS have not been well studied before in Egyptian patients. This study aimed to evaluate those potential predictors of increased risk of conversion within the first year.
Methods
Patients
This study is a longitudinal prospective study conducted on 43 patients diagnosed as clinically isolated syndrome according to McDonald’s criteria (2010) (Polman et al. 2011).The CSF oligoclonal bands could not be assessed in our cohort as the McDonald’s criteria (2010) was applied in this study. The ethical committee of faculty of medicine, Fayoum University has approved the study. Written informed consent was obtained from all patients and controls. The patients were recruited from Neurology Outpatient Clinic, Fayoum University from July 2014 to July 2015. The age of patients ranged from 19 to 55 years.
Methods
All the patients underwent full medical and neurological examination at baseline and after 1 year follow-up including history taking obtained by interviewing the patients, with special emphasis on the following: clinical presentation of the attacks, number of the attacks, and clinical evaluation of disability using Expanded Disability Status Scale (EDSS), and all the patients with CIS underwent visual evoked potential (VEP) evaluation. P 100 latency and amplitude were measured.
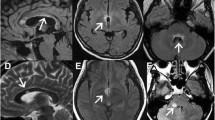
Magnetic resonance imaging of the brain and the cervical spinal cord with contrast was performed at baseline and after 1-year follow-up on 1.5-T superconductive magnetic utilizing spine echo (SE) pulse sequence. The following measures were evaluated manually including the whole T2 hyperintense lesions number, spinal T2 lesions number, and the whole gadolinium (Gd)-enhancing lesions number. The patients underwent clinical and radiological re-evaluation for early detection of conversion to clinically definite MS after 1 year follow-up. The main endpoint of this study relies mainly on follow-up of the CIS patients in a prospective way.
The patients were divided into two groups according to conversion to MS
-
Group Ia (patients who converted to clinically definite MS)
-
Group Ib (patients who did not convert to clinically definite MS)
Statistical analysis
Statistical package for social science (SPSS) version 19 was used for data management and analysis. The Mann-Whitney test was used for comparison of quantitative nonparametric variables including clinical presentation with either optic neuritis or transverse myelitis, percentage of patients with delayed P100 or not. Independent Student’s t test used to compare measures of two independent groups of quantitative parametric data. Logistic regression test was used to assess the association between categorical-dependent and categorical-independent variables and detection of risk ratio. The level p < 0.05 was considered the cut-off value for significance.
Results
Eight patients (19.6%) of the CIS group were converted to clinically definite MS (group Ia) after 1-year follow-up, as regards to their initial clinical presentation, six patients (75%) of the convertors (group Ia) presented with optic neuritis and two patients (25%) presented with spinal cord disorder.
It was found that the mean age at onset was lower in CIS patients who converted to CDMS (26.9 ± 4.4) versus (30.3 ± 4.5) with tendency to reach significant level (p = 0.06). Although females constituted the majority of cases, there was no significant difference between convertors and non-convertors on the basis of gender. As regards the clinical presentation, there was no statistically significant difference between the two groups whether they initially presented with optic neuritis or spinal cord disorder as shown in Table 1.
Although the patients that converted to CDMS showed significant higher EDSS as well as delayed P100 latency scores than non- convertors after 1-year follow-up, there was no significant difference at baseline between the two groups as illustrated in Tables 1 and 2.
In respect to radiological parameters, it was found that the convertors showed higher MRI T2 lesion number than non-convertors (group 1b) at baseline and after 1-year follow-up. However, there was no statistically significant difference in total Gd-enhancing T1 lesion number between the two groups at baseline as shown in Tables 1 and 2.
Multivariate logistic analysis showed that initial clinical presentation with optic neuritis (OR = 1.3, p = 0.003), higher MRI T2 lesion numbers (OR = 1.6, p = 0.002) were independent predicators of CIS conversion to clinically definite MS after 1-year. It was shown that the number of total T2 lesion that predict early conversion of CIS patients for MS was four supratentorial lesions with sensitivity (100%) and specificity (85.7%) as shown in Fig. 1.
Discussion
Clinically isolated syndrome is a term describing the first neurological episode that could be suggestive of multiple sclerosis. This may create a diagnostic and therapeutic dilemma given the difficulty in predicting who will be converting to CDMS. Clinical presentation in combination with MRI of the brain and CSF analysis can be used in CIS patients to detect the patients who at risk for clinically definite MS (Alroughani et al. 2012). It was found in this study that eight patients (19.6%) of CIS after 1-year follow-up were converted to clinically definite MS in concordance to these results, those of Martinelli et al. (2014) which that stated that only 19% of their CIS patients had converted to clinically definite MS in the first year of follow-up, and those of Zhang et al. (2016) which found that 22% of patients with CIS converted to clinically definite MS in first year follow-up and 52% patients converted to clinically definite MS at 5-year follow-up.
It was shown that the CIS patients that converted to MS were younger (below 30 years old) than non-convertors in this study with tendency to reach to a significant level. Similar to this result, Alroughani et al. (2012) found that the mean age of the convertors was less than 30 years and independently associated with a higher risk of developing a second event within 2 years of onset. It was postulated that the African American patients had more rapid disease progression than non-white race/ethnicity and was associated with a higher risk of early second event which has been associated with poorer long-term prognosis (Mowry et al. 2009).
Although most of the convertors were females, there was no statistically significant difference in gender between the two groups, in agreement with this result, some studies (Alroughani et al. 2012; Dobson et al. 2012) that stated that there was no effect of gender on the conversion rate of CIS.
In respect to clinical presentation, it was found that most of convertors (75% of the patients) were initially presented with optic neuritis, and that the multivariate logistic analysis showed that optic neuritis presentation was an independent predictor for conversion after 1-year follow-up in this study. There was a conflict of results in the literature, as Kuhle et al. (2015) found that 31% of the convertors presented with optic neuritis and only 20% presented with spinal cord syndrome, while on the other side, some researchers (Alroughani et al. 2012; Miller et al. 2005) reported that optic neuritis was associated with a lower risk of developing MS than other types of clinically isolated syndrome. This conflict could be attributed to geographical variation in clinical presentation and length of follow-up.
In this study, it was found that there was no significant difference in disability assessed by EDSS between the convertors and non-convertors at baseline while the CIS patients that converted to CDMS showed significant worse EDSS scores after 1-year. It was suggested that the EDSS scores of the first attack may have no significant role in predicting early conversion for CDMS. Bi et al. (2016) studied the characteristics of the CIS patients and their risk factors for progression to MS or neuromyelitis optica(NMO), and it was shown that the average EDSS score of the NMO group was higher than that of the MS group, suggesting that the NMO disability was higher than that of MS. Therefore, the diagnosis of NMO should be paid attention to when the EDSS score of CIS was higher at their initial presentation.
It was suggested that the neurophysiological studies could predict conversion for CDMS in CIS patients as Swanton et al. (2006) study showed that 64% of CIS patients had VEP abnormal rate, and 24% of the patients had somatosensory evoked potential abnormal rate suggesting that the evoked potential studies were of great value for the prediction of CIS conversion. In this study, there was no significant difference in VEP results between convertors and non-convertors at baseline while, the convertors showed significant delayed p100 latency than non-convertors after 1-year. In agreement with these results, Bi et al. (2016) stated that the individually evoked potential was not predictable for CIS transformation. But the combination of two or three evoked potential anomalies may be helpful in prediction of CIS prognosis.
Conventional MRI has a well-established role in the initial assessment of patients with CIS. The risk for conversion to CDMS is greater in patients presenting with abnormal T2-weighted images. It was found that 50 to 70% of the patients with CIS may have asymptomatic abnormal T2-weighted images at their initial presentation (Miller et al. 2012). Several studies (Kuhle et al. 2015; Alroughani et al. 2012; Miller et al. 2012) had postulated that the number of MRI lesions at baseline was a strong predictor to MS conversion in the CIS patients as those who had ≥ 9 T2 lesion were at a higher risk for conversion. In this study, it was found that the patients that had converted to CDMS have a significant higher T2 lesion numbers at baseline and after 1-year follow-up. Moreover, the multivariate regression analysis had confirmed that higher MRI lesion number is an independent predictor of conversion.
Interestingly, it was found that the number of total MRI brain T2 lesion at the baseline that predict early conversion of CIS patients to MS was four lesions with sensitivity (100%) and specificity (85. 7%).While Martinelli et al. (Martinelli et al. 2014) stated that the number of MRI T2 lesions at baseline appeared to be predictive of CDMS was nine lesions. For patients with fewer than nine lesions, the conversion rate to CDMS was 50 vs. 66% for the patients with nine or more lesions. This difference in results could be attributed to the small numbers of patients and short duration of follow-up.
Although the previous studies (Brex et al. 1999; Pestalozza et al. 2005; Zivadinov et al. 2013) had postulated that the increased risk of conversion for MS was associated with the presence of gadolinium-enhancing lesions, there was no statistically significant difference in the total T1 lesion number between the converted and non-converted groups in this study. Accurate estimation of the incidence of Gd-enhancing lesions at CIS presentation is difficult because of inconsistent administration of contrast across studies. Gd-enhancing lesions may only be present in subjects with abnormal T2-weighted images (Brex et al. 1999). The presence of at least one Gd-enhancing lesion is predictive of time to CDMS in monofocal, but not in multifocal presentations (Nielsen et al. 2009).
This study had some limitations including a short-duration follow-up and small number of participants. Moreover, there is a lack of application of McDonald’s criteria 2017 in this study as this manuscript was submitted to the Egyptian journal of neurology before the publication of McDonald’s criteria 2017. It is highly recommended to have a further estimation of the CSF oligoclonal bands in the patients with CIS to fulfill dissemination of time to determine who will convert to CDMS according McDonald’s criteria 2017 in the upcoming studies.
Conclusions
It was concluded that the patients with CIS that initially presented with optic neuritis and higher MRI brain lesion number are at higher risk for conversion to clinically definite MS, and initiation of disease-modifying therapy should be considered as early as possible to overcome the worse long-term outcomes.
Abbreviations
- CDMS:
-
Clinically definite multiple sclerosis
- CIS:
-
Clinically isolated syndrome
- CNS:
-
Central nervous system
- CSF:
-
Cerebrospinal fluid
- EDSS:
-
Expanded Disability Status Scale
- Gd:
-
Gadolinium
- MRI:
-
Magnetic resonance imaging
- MS:
-
Multiple sclerosis
- NMO:
-
Neuromyelitis optica
- SE:
-
Spine echo
- SPSS:
-
Statistical package for social science
- VEP:
-
Visual evoked potential
References
Alroughani R, Al Hashel J, Lamdhade S, Ahmed SF. Predictors of conversion to multiple sclerosis in patients with clinical isolated syndrome using the 2010 revised McDonald criteria. Int Sch Res Netw. 2012;2012:1–6. https://doi.org/10.5402/2012/792192.
Amato MP, Ponziani G, Bartolozzi ML, Siracusa G. A prospective study on the natural history of multiple sclerosis: clues to the conduct and interpretation of clinical trials. J Neurol Sci. 1999;168(2):96–106.
Bi CF, Qian HR, Peng LJ, et al. The correlation factor analysis for conversion of clinically isolated syndrome to multiple sclerosis and neuromyelitis optica. Zhonghua Nei Ke Za Zhi. 2016;55(6):460–5.
Brex PA, O’Riordan JI, Miszkiel KA, et al. Multisequence MRI in clinically isolated syndromes and the early development of MS. Neurology. 1999;53(6):1184–90. https://doi.org/10.1212/WNL.53.6.1184.
Dobson R, Ramagopalan S, Giovannoni G. The effect of gender in clinically isolated syndrome (CIS): a meta-analysis. Mult Scler. 2012;18(5):600–4.
Frohman EM, Havrdova E, Lublin F, et al. Most patients with multiple sclerosis or a clinically isolated demyelinating syndrome should be treated at the time of diagnosis. Arch Neurol. 2006;63(4):614.
Kuhle J, Disanto G, Dobson R, et al. Conversion from clinically isolated syndrome to multiple sclerosis: a large multicentre study. Mult Scler J. 2015;21(8):1013–24. https://doi.org/10.1177/1352458514568827.
Martinelli V, Dalla Costa G, Colombo B, et al. Vitamin D levels and risk of multiple sclerosis in patients with clinically isolated syndromes. Mult Scler J. 2014;20(2):147–55. https://doi.org/10.1177/1352458513494959.
Miller D, Barkhof F, Montalban X, Thompson A, Filippi M. Clinically isolated syndromes suggestive of multiple sclerosis, part I: natural history, pathogenesis, diagnosis, and prognosis. Lancet Neurol. 2005;4(5):281–8.
Miller DH, Chard DT, Ciccarelli O, Reingold S, Neurologists UMC, Kardon R. Clinically isolated syndromes. Lancet Neurol. 2012;11(2):157–69.
Mowry EM, Pesic M, Grimes B, Deen SR, Bacchetti P, Waubant E. Clinical predictors of early second event in patients with clinically isolated syndrome. J Neurol. 2009;256(7):1061–6.
Nielsen JM, Pohl C, Polman CH, et al. MRI characteristics are predictive for CDMS in monofocal, but not in multifocal patients with a clinically isolated syndrome. BMC Neurol. 2009;9(1):19.
Pestalozza IF, Pozzilli C, Di Legge S, et al. Monthly brain magnetic resonance imaging scans in patients with clinically isolated syndrome. Mult Scler J. 2005;11(4):390–4.
Polman CH, Reingold SC, Banwell B, et al. Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol. 2011;69(2):292–302. https://doi.org/10.1002/ana.22366.
Swanton JK, Fernando K, Dalton CM, et al. Modification of MRI criteria for multiple sclerosis in patients with clinically isolated syndromes. J Neurol Neurosurg Psychiatry. 2006;77(7):830–3.
Thompson AJ, Banwell BL, Barkhof F, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018;17(2):162–73. https://doi.org/10.1016/S1474-4422(17)30470-2.
Weinshenker BG, Bass B, Rice GP, et al. The natural history of multiple sclerosis: a geographically based study. 2. Predictive value of the early clinical course. Brain. 1989;112(Pt 6):1419–28.
Zhang Y, Liu G, Han X, Dong H, Geng J. The association of serum 25-hydroxyvitamin D levels with multiple sclerosis severity and progression in a case-control study from China. J Neuroimmunol. 2016;297:127–31.
Zivadinov R, Havrdová E, Bergsland N, et al. Thalamic atrophy is associated with development of clinically definite multiple sclerosis. Radiology. 2013;268(3):831–41.
Ethics approval reference
The research has been approved in the ethical committee, Faculty of medicine, Fayoum University on March 25, 2014, with reference number (1) and code (D-8).
Author information
Authors and Affiliations
Contributions
HAS is responsible for conception of the work, analyzing, interpreting the data, and approving the final reversion of the work. SSS is responsible for analyzing and interpreting the data of the work. LID is responsible for drafting the work, analyzing, interpreting the data, and communicating with the journal during the manuscript submission, peer review, and publication process. MAT is responsible for collecting data and writing the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Faculty of Medicine, Fayoum University Ethical Committee had approved the study; written informed consent were obtained from all the patients and control volunteers before the study initiation.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no conflicts of interest. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Shaheen, H.A., Sayed, S.S., Daker, L.I. et al. Early predictors of conversion in patients with clinically isolated syndrome: a preliminary Egyptian study. Egypt J Neurol Psychiatry Neurosurg 54, 21 (2018). https://doi.org/10.1186/s41983-018-0021-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41983-018-0021-3