Abstract
Background
Achilles tendinopathy is the most prevalent tendon disorder in people engaged in running and jumping sports. Aetiology of Achilles tendinopathy is complex and requires comprehensive research of contributing risk factors. There is relatively little research focussing on potential biomedical risk factors for Achilles tendinopathy. The purpose of this systematic review is to identify studies and summarise current knowledge of biomedical risk factors of Achilles tendinopathy in physically active people.
Methods
Research databases were searched for relevant articles followed by assessment in accordance with PRISMA statement and standards of Cochrane collaboration. Levels of evidence and quality assessment designation were implemented in accordance with OCEBM levels of evidence and Newcastle-Ottawa Quality Assessment Scale, respectively.
Results
A systematic review of the literature identified 22 suitable articles. All included studies had moderate level of evidence (2b) with the Newcastle-Ottawa score varying between 6 and 9. The majority (17) investigated genetic polymorphisms involved in tendon structure and homeostasis and apoptosis and inflammation pathways.
Overweight as a risk factor of Achilles tendinopathy was described in five included studies that investigated non-genetic factors. COL5A1 genetic variants were the most extensively studied, particularly in association with genetic variants in the genes involved in regulation of cell-matrix interaction in tendon and matrix homeostasis. It is important to investigate connections and pathways whose interactions might be disrupted and therefore alter collagen structure and lead to the development of pathology. Polymorphisms in genes involved in apoptosis and inflammation, and Achilles tendinopathy did not show strong association and, however, should be considered for further investigation.
Conclusions
This systematic review suggests that biomedical risk factors are an important consideration in the future study of propensity to the development of Achilles tendinopathy. The presence of certain medical comorbidities and genetic markers should be considered when contemplating the aetiology of Achilles tendinopathy. Further elucidation of biomedical risk factors will aid in the understanding of tendon pathology and patient risk, thereby informing prevention and management strategies for Achilles tendinopathy.
Trial Registration
PROSPERO CRD42016036558
Similar content being viewed by others
Key Points
-
Increased BMI and adverse lipid profile may be important biomarkers of Achilles tendinopathy.
-
Further research is required to confirm an association between genetic variation, of genes encoding collagen proteins and proteins involved in pathways of tendon homeostasis and Achilles tendinopathy.
-
Genetic risk factors of Achilles tendinopathy may be modified by geographic factors.
Background
Achilles tendinopathy is one of the most prevalent overuse tendon injuries associated with physical activities such as running and jumping [1]. It is the most common Achilles tendon disorder, with the highest incidence among runners, track and field athletes and volleyball, tennis and soccer players [1]. The term ‘tendinopathy’ is an umbrella term for the description of tendon conditions encompassing pain, swelling and impaired performance [2, 3]. Achilles tendinopathy can be acute or chronic. Diagnosis is usually made via a combination of clinical history, physical examination with or without medical imaging. The Victorian Institute of Sport Assessment-Achilles questionnaire (VISA-A questionnaire) may also be used to grade the severity of tendinopathy. In the acute phase, the cardinal symptoms are morning pain and stiffness and pain at the beginning and end of exercise sessions, with relief in between. The tendon is diffusely swollen, and there may be palpable crepitus. Tenderness is maximal 2–6 cm above the insertion. In chronic tendinopathy, the tendon remains painful with exercise but the tendon is nodular and thickened rather than swollen and oedematous [4, 5].
Originally, the pain of Achilles tendinopathy was attributed to an inflammatory process. While inflammatory cells have been observed, particularly in the early stages of Achilles tendinopathy, the response does not seem to be a traditional inflammatory response [6, 7]. Several models have been proposed to explain the aetiology of Achilles tendinopathy [8,9,10]. The continuum model of tendon pathology suggested by Cook and Purdam consists of three stages: reactive tendinopathy, tendon dysrepair and degenerative tendinopathy [9]. The first stage of the pathology results from acute overload of the Achilles tendon and can be characterised as a non-inflammatory proliferative response in the cell and matrix. The second stage is described as attempted tendon healing, through increased production of collagen and proteoglycans. Degenerative tendinopathy is the third stage and characterised by potentially irreversible changes in cell and matrix condition such as tenocyte apoptosis and matrix disorder [11]. Conservative, non-invasive management is the initial treatment of choice for Achilles tendinopathy, particularly in the early phases [4]. Recalcitrance to conservative management is not uncommon however, and some clinicians argue that conservative management of chronic Achilles tendinopathy is time consuming and unsatisfactory [5]. Surgery is sometimes recommended after exhaustion of conservative treatments, but response rates are variable [5].
Intrinsic and extrinsic aetiological factors interact in the genesis of Achilles tendinopathy. Intrinsic risk factors include demographic factors (sex, age, weight and height) and genetic polymorphisms; and local anatomical factors include leg length discrepancy, malalignment and decreased flexibility. Extrinsic factors comprise therapeutic agents (corticosteroids, antibiotics), environmental conditions, and physical activity-related factors, including training patterns, technique and equipment [1, 2]. The majority of the studies published over the last two decades are dedicated to the investigation of anatomical features and biomechanical faults as possible causes of Achilles tendinopathy. Several reviews have identified certain anatomic characteristics and biomechanical and training load errors as risk factors for Achilles tendinopathy [12,13,14,15].
The contribution of biomedical risk factors to the development of Achilles tendinopathy remains unclear. These may include medical comorbidities and physiological, biochemical and genetic factors. Imaging and histopathological analysis of the degenerative and recovery processes in tendon have provided a better understanding of the processes associated with tendon structure and metabolism. In terms of biochemical and metabolic processes, tendon tissue is relatively inert, with new collagen synthesis being a slow process [5]. Looking at the genetic coding of proteins comprising tendon structure may lead to a better understanding of the underlying molecular processes. Several genetic association studies have demonstrated that genetic polymorphisms influence collagen tissue structure, its turnover, degradation processes and therefore susceptibility to tendon injuries. Medical comorbidities and treatment of medical conditions also affect tendon structure and function [16, 17].
There is relatively little research focussing on potential biomedical risk factors for Achilles tendinopathy. The purpose of this systematic review is to identify studies and summarise current knowledge of biomedical risk factors of Achilles tendinopathy in physically active people. This information will contribute to the understanding of Achilles tendinopathy and may inform future prevention strategies.
Methods
Literature Search Strategy
This systematic review was registered in the international prospective register of systematic reviews PROSPERO (registration number CRD42016036558). Systematic review methodology included a thorough search of all accessible databases of scientific articles. Keywords were selected by following PICO (Patient, Intervention, Comparison, Outcome) principle [18]. Four databases (CINAHL, EMBASE, PubMed and SPORTDiscus) were searched using various combinations of the keywords: “risk OR predisposition OR genetic* OR aetiology OR etiology OR overuse OR pathogenesis” AND “Achilles OR Achilles Tendon” AND “tendinopathy* OR tendinitis OR tendonitis OR tendinosis OR injury OR pain” AND “exercise OR physical activity OR sport* OR run*”. Articles were assessed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [19] and the standards of Cochrane collaboration [18]. The search was completed in August 2016.
Selection Criteria
Selected articles from each database were combined in one electronic library EndNote (Thomson Reuters, version X7). Duplicates were removed automatically in the electronic library. The titles and abstracts were then scanned, and clearly irrelevant studies and the remainder of the duplicates were removed. Following exclusion/inclusion criteria, two reviewers examined the abstracts of the remaining articles and selected studies for the full-text review. Inclusion criteria were the following: (a) retrospective and prospective studies, case-control studies and cohort studies investigating risk factors of Achilles tendinopathy; (b) clear definition of the studied injury and medical diagnosis of the injury; and (c) physically active people as studied subjects. Discrepancies in the lists of selected articles were resolved through the discussion between the reviewers.
Quality Assessment
The quality of the included studies was evaluated applying the Newcastle-Ottawa Quality Assessment Scale (NOS) for case-control and cohort studies [20]. This assessment checklist is recommended by the Cochrane Handbook for Systematic Reviews of Interventions [18, 21]. The NOS checklist assesses quality of the articles in three domains: selection of the studied groups; comparability of the groups and control for confounding factors; and exposure for case-control studies or outcome for cohort studies. Total maximum score is nine for both types of studies. Results of the studies were critically analysed and presented in the narrative form reporting odds ratios (OR) and confidence intervals.
Levels of Evidence
Oxford Centre for Evidence-based Medicine (OCEBM) levels of evidence was used as a guidance to evaluate selected articles. Levels of evidence could be identified according to the type of clinical question [22].
Results Presentation
Results of the studies are described in narrative form, and odds ratios and confidence intervals or relative risks of developing Achilles tendinopathy are reported in Table 2 where possible.
Results
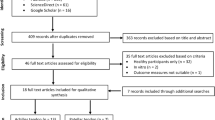
A total of 1631 articles were retrieved after the search of four databases. Following removal of duplicates, 1185 articles remained. Following screening of titles and abstracts, reviewers selected 30 articles as potentially relevant. The final 22 articles were included in the review after full-text screening and discussion between the reviewers. A flow chart of the article selection is given in Fig. 1. All included articles were published in English and had a mixed population of physically active people. Of the 22 included studies, 17 studies recruited runners and people who participated in recreational sports such as squash [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. A single epidemiology study involved military personnel [40], while one study included elderly people involved in tennis, jogging and speed walking [41]. Another study recruited master and veteran athletes from race walking, long- and middle-distance running, jumping, hurdles and sprinting [42]. The remaining two studies recruited physically active people but did not identify the specific physical activities of the recruited cohorts [43, 44]. The majority of studies, 17 of 22, used the same definition of Achilles tendinopathy, assessing clinical diagnostic criteria of symptoms persisting in the Achilles tendon area [26]. One study’s clinical assessment included VISA-A questionnaire as an assessment tool [42]. Twenty-one out of 22 studies involved professional medical diagnosis of Achilles tendinopathy and additionally imaging records’ assessment. The epidemiology study examined over 80,000 medical records of military personnel relied on electronic medical record data [40].
The quality assessment using the NOS tool is presented in the Table 1. Three studies reached maximum score of nine [40, 42, 44], and the lowest score was six, shown in two studies [24, 28]. Studies with the score of nine included one epidemiologic cohort study of military personnel and two cross-sectional studies [40, 42, 44]. As the systematic review selection criteria excluded other systematic reviews, all included studies were assessed as moderate by the level of evidence (levels 3 and 4) (Table 2).
Discussion
The selected studies focused on a diverse range of biomedical risk factors for Achilles tendinopathy such as demographic factors, chronic medical conditions, lifestyle habits and genetic factors, including those contributing to collagen structure and tendon homeostasis and those involved in apoptosis and inflammation. The majority of the included studies were case-control studies (Fig. 1). The main limitation of the included studies was their level of evidence. According to the recommended OCEBM hierarchy, cohort and case-control studies approach levels of evidence 3 and 4, with systematic reviews and randomised controlled trials providing levels 1 and 2 evidence [45].This limitation must be taken into consideration when reviewing the results of these studies. Here, we discuss the different approaches undertaken and highlight the main findings obtained in the search for the key biomedical risk factors for Achilles tendinopathy.
Non-Genetic Biomedical Risk Factors
Biomedical risk factors include non-modifiable factors such as age, sex, weight and chronic medical conditions. A cross-sectional study on 178 master track and field athletes did not find any association between Achilles tendinopathy (as determined by VISA-A scores) and age, sex, weight or height [42]. However, the recruitment approach used in this study may have resulted in unintentional exclusion of those with the most severe AT as these athletes may not have been able to compete at the events where recruitment took place.
A study of 450 cases of Achilles tendinopathy in a large military personnel cohort showed that overweight and obesity had a strong association with the development of the injury. Additionally, this study found that moderate alcohol use was associated with increased risk of Achilles tendinopathy. However, the magnitude of the OR was modest and could be explained by the possible influence of alcohol on metabolic and inflammatory factors [40]. A case-control study of 60 patients with mid-portion Achilles tendinopathy and 60 matched uninjured controls by age, sex and body mass index (BMI) showed that patients with Achilles tendinopathy had higher levels of triglycerides (TG), lower levels of high-density lipoprotein cholesterol (HDL-C) and higher TG:HDL-C ratio. These lipid profiles are typical for insulin resistance syndrome and usually described as dyslipidemia. This finding suggests that serum lipids may be involved in the development of Achilles tendinopathy [43, 44]. A second study investigated fat distribution on male and female patients with asymptomatic Achilles tendinopathy. Ultrasound examinations of Achilles tendon in 298 participants identified a higher pathology rate among men than women (17/127, 13%, versus 8/171, 5%). Males with asymptomatic Achilles tendon pathology had elevated waist:hip ratio, were older and had higher central/peripheral fat mass and larger waist circumferences (above 83 cm) compared to individuals without tendon pathology. This pattern of fat tissue distribution around the abdominal area is usually associated with metabolic syndrome and might be linked to the previously reported association between dyslipidemia and Achilles tendinopathy. Surprisingly, women with asymptomatic Achilles tendon pathology had lower central:peripheral fat mass ratios compared to women without pathology, which could be explained by the effect of oestrogen on body fat distribution, a factor that was not investigated in this study [44]. A recent study comparing patients with Achilles tendinopathy aged over 65 years old to matching uninjured controls showed significantly higher prevalence of diabetes, higher BMI and higher level of sport participation in the injured group [41]. These findings are consistent with other studies which indicate susceptibility in those with chronic comorbidities. The types of exercises undertaken by the subjects (speed walking, jogging and tennis) were relatively high risk in nature and may have been beyond the loading capacity of the tendon in ageing individuals [41]. The link between adverse lipid profile and tendinopathy could be explained by adipokine modulation of certain enzymes’ production which are important for tenocyte functioning. Additionally, chronic low-grade inflammation, which is typical for obesity, may affect tendon healing process. At the same time, tendon healing is also disrupted by low concentrations of immune cells that tend to migrate into adipose tissue [46]. A systematic review of 17 articles on the link between lipid profile and tendon health showed a strong association between tendon pathology and high lipid parameters [47].
Genetic Contributors to Collagen Structure and Tendon Homeostasis
Genetic variations are alterations in DNA sequence among individuals that may account for differences in phenotype and occasionally in health state. Genetic variations occurring in more than 1% of a population are considered useful polymorphisms for genetic linkage analysis. One of the most commonly investigated types of genetic variation is the single-nucleotide polymorphism (SNP), a variation in a single nucleotide located at a specific position in the DNA [48]. The genetic studies included in this review all employed a candidate gene approach in order to find genetic polymorphisms in genes that might influence tendon structure and its development and therefore either predispose to or protect from the development of Achilles tendinopathy. Genetic predisposition has long been proposed as a contributor to the development of Achilles tendinopathy. Early studies assessed the genetic association between ABO blood type and tendon injuries, described in several investigations of Finnish and Hungarian patients [49, 50]. However, further research did not support this link, but identified the chromosomal region of interest on the long arm of chromosome 9 (9q), which carries genes closely linked to the ABO blood group gene [27].
This review includes 14 studies investigating 16 genes linked to collagen structure and tendon homeostasis. Two of these investigated genes located in 9q region, particularly tenascin-C (TNC) and COL5A1 [26, 27]. Both studies found an association of polymorphic variants of TNC and COL5A1 genes with the development of Achilles tendinopathy. Tenascin-C regulates cell-matrix interaction in tendon. TNC contained a polymorphism in intron 17 where the number of GT dinucleotide repeats ranged from 3 to 21, and 95% of the alleles contained 12 to 17 GT repeats. Those subjects who were homozygous or heterozygous for the underrepresented alleles of TNC (containing either 13 or 17 GT repeats) were 6.2 times less likely to develop Achilles tendon injury [26] indicating that these variants of TNC may be protective from Achilles tendinopathy. COL5A1 encodes the pro-a1 (V) chain of the type V collagen. Two variants of the COL5A1 gene were associated with an increased risk of Achilles tendinopathy. In contrast, a third variant was underrepresented in subjects with Achilles tendinopathy and therefore was associated with a reduced likelihood of Achilles tendinopathy development [27]. A follow-up study published by the same research group from South Africa in collaboration with researchers from Australia replicated previous shown associations linking COL5A1 gene variants to Achilles tendinopathy in both Australian and South African populations [33]. These studies demonstrate the relevance of the TNC and COL5A1 gene polymorphisms in genetic predisposition to Achilles tendinopathy.
Other studies have assessed the contribution of haplotypes constructed from candidate polymorphisms, in an effort to find interactions between genes or gene products. A collaborative study investigated COL27A1 gene polymorphisms in conjunction with TNC, as COL27A1 is located in the same region of chromosome 9 as the TNC gene. Type XXVII collagen, encoded by COL27A1, is responsible for the key structural framework and tensile strength of the interstitial matrices. Although there were no significant associations between COL27A1 and Achilles tendinopathy, a GCA haplotype (a set of genetic variants located on a single chromosome) constructed from one COL27A1 polymorphism (rs946053) and two TNC polymorphisms (rs13321, rs2104772) showed significant association with Achilles tendinopathy [30]. The study of COL5A1 and MIR608 polymorphisms in South African and Australian cohorts found that a variant of COL5A1 contains a putative polymorphic micro-RNA binding site. The results showed that polymorphisms rs71746744, rs16399 and rs1134170 in COL5A1 and polymorphism rs4919510 in MIR608, which encodes a small micro-RNA, were all independently associated with Achilles tendinopathy, suggesting a role for these four variants on messenger ribonucleic acid (mRNA) stability and the resulting type V collagen synthesis [23]. A follow-up study of the same polymorphisms in a British cohort did not find any independent association between studied COL5A1, MIR608 or IL1β variants and Achilles tendinopathy as it was shown in Australian and South African cohorts [36]. However, an inferred allele combination constructed from COL5A1 SNPs rs12722, rs3196378 and rs71746744 was associated with the risk of Achilles tendon pathology [36].
A further study conducted on South African subjects analysed polymorphisms in the gene encoding for matrix metalloproteinase 3 (MMP3) which is involved in the regulation of extracellular matrix homeostasis. Three of the investigated polymorphisms (rs679620, rs591058, rs650108) showed strong association with Achilles tendinopathy, and the most underrepresented haplotype in patients with Achilles tendinopathy indicated that this variant was protective against Achilles tendinopathy [31]. Moreover, since MMP3 genotyping had been done on the same cohort as COL5A1 reported by September (2009) [33], this study presented allelic combinations of MMP3 rs679620 and COL5A1 rs12722, which are associated with a lower risk of Achilles tendinopathy. Type V collagen is a substrate for MMP3; hence, genetic variants in COL5A1 and MMP3 genes could account for differences in the interactions between the proteins [31]. Further investigation of MMP3 gene’s polymorphisms showed that an inferred haplotype of four SNPs (rs3025058, rs679620, rs591058 and rs650108) was associated with Achilles tendinopathy in an Australian cohort [37].
Polymorphisms in COL12A1 (rs240736, rs970547) and COL14A1 (rs4870723, rs1563392) were investigated as they both encode for proteins involved in the biological processes of fibrillogenesis and, like tenascin C, in the modulation of the tendon response to mechanical stress [34]. Additionally, one study of two cohorts from South Africa and Australia investigated polymorphisms in the three genes coding for type XI collagen that is homologous to type V collagen in function and structure [25]. Type XI collagen is usually expressed not only in cartilage but also in developing tendons. Several polymorphisms (COL11A1 rs3753841 and rs1676486, COL11A2 rs1799907) have been associated with lumbar disc herniation and rheumatoid arthritis. Whilst none of the polymorphisms were independently associated with Achilles tendinopathy, the construction of a pseudohaplotype consisting of three polymorphisms and the COL5A1 polymorphism rs71746744 revealed a significant association with Achilles tendinopathy. It is hypothesized that the interaction of genes encoding for type V and XI collagens could modulate risk of Achilles tendinopathy, allowing for the possibility that the effects of type XI collagen variants in the developing tendon might affect the structural or functional properties of the mature tendon [25].
Genes involved in tendon homeostasis and particularly in the extracellular matrix (ECM) have also been investigated for their association with Achilles tendinopathy risk [24]. The ADAMTS (a disintegrin and metalloproteinase with thrombospondin motifs) family of proteinases are involved in ECM homeostasis and reported to be more highly expressed in pathologic than in healthy tendons. Tissue inhibitor of metalloproteinases (TIMP) inhibits the actions of MMPs and ADAMTS. Previously studied cohorts were genotyped for the ADAMTS2 rs1054480, ADAMTS5 rs226794, ADAMTS14 rs4747096, ADAMTS12 rs3740199 and TIMP2 rs4789932 gene variants. Researchers found a significant association between the rs4789932 TIMP2 variant and Achilles tendinopathy. The balance between TIMPs and MMPs could be a contributing factor for Achilles tendinopathy development [24]. The replication of the study of MMP3 and TIMP2 gene variants in a British cohort showed that a gene variant in TIMP2 rs4789932 was associated with a reduced risk of Achilles tendon pathology in males [38]. The continued investigation of proteins involved in the tendon structure included research of fibrillin and elastin for their role in elasticity, strength and flexibility of tendons. The polymorphisms FBN2 rs331079 and ELN rs2071307 were studied in Australian and South African cohorts, and the GG genotype in rs331079 was overrepresented in the group with Achilles tendinopathy, indicating an association between fibrillin and injury [35]. Another study conducted on the same cohorts investigated the contribution of genes encoding growth factors which play an important role in tendon growth and homeostasis. TGFB1 and GDF5 (encoding for transforming growth factor-β1 and growth/differentiation factor-5, respectively) were selected as candidates as these proteins had been shown to increase mechanical strength after gene transfection in Achilles tendon in experimentally injured animals [51]. This study showed a significant association of Achilles tendinopathy with GDF5 rs143383. However, no association with TGFB1 rs1800469 was identified [29].
A thorough analysis of polymorphisms in COL5A1 identified this gene as one of the most likely predisposing factors for Achilles tendinopathy. However, several studies investigating polymorphisms in genes encoding for proteins interacting with type V collagen showed that it is important to be aware of possible connections and pathways whose interactions might be disrupted and therefore alter collagen structure and its functionality and lead to increased or decreased risk of Achilles tendinopathy.
Genetic Contributors to the Pathways Involved in Apoptosis and Inflammation
Candidate genes involved in processes surrounding the development of Achilles tendinopathy, such as tendon turnover and inflammation, have also been considered as possible genetic risk factors. The presence of SNPs in cytokine genes, important contributors to the inflammatory response which have been shown to be upregulated in tendinopathy and mechanically loaded tendon were investigated. Interleukin-1β (IL1β) induces inflammatory mediators that upregulate the expression of proteins involved in degradation of the tendon extracellular matrix such as MMPs which target type V collagen. The IL1β receptor antagonist, IL1ra, is encoded by the IL1RN gene, and its variable number tandem repeat (VNTR) rs2234663 polymorphism has been previously associated with gastrointestinal diseases [52], osteoporotic fractures [53] and atherosclerosis [54]. Whilst genetic variants in IL1β (rs1143627 and rs16944) have been implicated to an increase in IL1β gene expression [55], interleukin-6 (IL6) was found to be linked to tenocyte apoptosis, which is a characteristic of tendinopathy. IL1β and IL6 may also affect COL5A1 gene expression [32]. A SNP in IL6 (rs1800795) was previously shown to alter IL6 expression [56] which may lead to increased tenocyte apoptosis and therefore potentially increase risk for Achilles tendinopathy development. In total, the study investigated four polymorphisms in IL1β, IL1RN and IL6, although none of these polymorphisms were associated with the Achilles tendinopathy diagnosis in either of the South African and Australian population groups studied. However, inferred allele combinations constructed from previously studied COL5A1 polymorphisms and these IL1β, IL6 and IL1RN VNTR polymorphisms were associated with an increased risk of Achilles tendinopathy in combined groups [32]. This study concluded that genetic polymorphisms contributing to the changes in inflammatory pathways may be important contributors to the risk of Achilles tendinopathy.
Polymorphisms in genes encoding caspases (CASP) and nitric oxide synthases (NOS) have also been investigated as these molecules had been shown to be involved in pathways accompanying tendon cell apoptosis, and their expression has been found to be elevated in tendinopathy [28]. South African and Australian cohorts were genotyped for four polymorphisms (CASP8 rs3834129, rs1045485, NOS3 rs1799983 and NOS2 rs2779249). A significant association between both CASP8 polymorphisms (rs3834129, rs1045485) and Achilles tendinopathy was found in both populations. The D/D genotype of rs3834129 was associated with tendinopathy, whilst the C allele of rs1045485 was associated with the absence of Achilles tendinopathy. NOS3 (rs1799983) and NOS2 (rs2779249) were not associated with Achilles tendinopathy. However, the data presented in this study showed that the control group in the Australian cohort was not in Hardy-Weinberg equilibrium (HWE), which refers to constant proportions of allele and genotype frequencies in a population, and therefore, this association should be interpreted with caution. Deviations from HWE in the control group may indicate significant methodological flaws including selection bias, population stratification and genotyping errors [57]. Another drawback of this study was the conclusion that with an odds ratio (OR) of 1.67 for the presence of D/D genotype of rs3834129, the risk of Achilles tendinopathy was 68% higher in the tendinopathy group than in the control group [28]. An OR represents the odds that an outcome will occur given a particular exposure, compared to the odds of the outcome occurring in the absence of that exposure [58]. Therefore, OR does not represent the probability of the outcome, and risk assumptions in percentages may not be valid. Overall, this study was the first that investigated polymorphisms in caspase pathways.
Tumour necrosis factor receptor 1 gene TNFRSF1A, which signals inflammation and apoptosis in response to the tumour necrosis factor-alpha (TNFα), was investigated as a potential gene associated with Achilles tendinopathy [59]. TNFRSF1A rs4149577 had been associated with several musculoskeletal and inflammatory diseases; however, this study was the first to investigate this polymorphism in association with Achilles tendinopathy. Another polymorphism included in this study was the caspase-3 gene CASP3 rs1049253, which was shown to influence CASP3 mRNA expression. Caspase-3 is involved in cellular apoptosis, including roles in chromatin condensation and DNA fragmentation [60]. This study also investigated the influence of the copy number variant (CNV) spanning intron 11-intron 12 in CASP8. CNVs are segments of DNA greater than 1 kb in size that can influence phenotypes by changing gene dosage and disruption of coding sequences in DNA. The results did not show any significant association between Achilles tendinopathy, the investigated polymorphisms and CNV. This is possibly due to the study limitations, such as a relatively small sample size and a possible additional degree of error due to the rounding of copy number data into discrete calls, or may indicate that there is no association between these CNVs and Achilles tendinopathy [39].
While these studies indicate some links between polymorphisms in genes involved in apoptosis and inflammation and Achilles tendinopathy, the majority of these studies were unable to demonstrate that these genes are probable risk factors for Achilles tendinopathy. The processes of apoptosis and inflammation clearly play a role in the pathology of Achilles tendinopathy; however, further investigation should be undertaken to clarify the role of genetic contributors in this pathological processes.
Conclusions
It is clear from previous research that biomechanical issues and training load errors are risk factors for Achilles tendinopathy [14]. This systematic review suggests that biomedical risk factors are an important consideration in the future study of propensity to the development of Achilles tendinopathy. Increased BMI and adverse lipid profile were associated with tendinopathy and may be important biomarkers of tendon pathology. It is evident that certain genetic markers contribute to the risk profile of Achilles tendinopathy; however, the demonstrated associations are currently somewhat ambiguous, and predictive power has not been demonstrated. Further investigation is required in this area. In addition, there appears to be diversity in the genes, dependent on geographical differences that are significantly associated with Achilles tendinopathy. This suggests that genetic risk factors for tendinopathy might be modified by geographic factors. It is evident that the risk of Achilles tendinopathy conferred by biomedical factors is complex and may be a result of the interplay between various genetic, biochemical and systemic factors which may be exacerbated by physical load. Further elucidation of biomedical risk factors will aid in the understanding of tendon pathology and patient risk, thereby informing prevention and management strategies for Achilles tendinopathy.
Abbreviations
- ADAMTS:
-
A disintegrin and metalloproteinase with thrombospondin motifs
- CASP :
-
Gene encoding caspases
- CNV:
-
Copy number variant
- COL11A1 :
-
Gene encoding pro-alpha1(XI) chain of type XI collagen
- COL11A2 :
-
Gene encoding pro-alpha2(XI) chain of type XI collagen
- COL12A1 :
-
Gene encoding alpha chain (XI) of type XII collagen
- COL14A1 :
-
Gene encoding alpha chain (XI) of type XIV collagen
- COL27A1 :
-
Gene encoding Type XXVII collagen
- COL5A1 :
-
Gene encoding pro-alpha1 (V) chain of the type V collagen
- DNA:
-
Deoxyribonucleic acid
- ECM:
-
Extracellular matrix
- ELN :
-
Gene encoding elastin
- FBN2 :
-
Gene encoding fibrillin-2
- GDF5 :
-
Gene encoding growth/differentiation factor-5
- HDL-C:
-
High-density lipoprotein cholesterol
- HWE:
-
Hardy-Weinberg equilibrium
- IL1RN :
-
Gene encoding IL1β receptor antagonist IL-1ra
- IL1β:
-
Gene encoding Interleukin-1β
- IL6 :
-
Gene encoding Interleukin-6
- MIR608 :
-
Gene encoding small micro-RNA
- MMP3 :
-
Gene encoding matrix metalloproteinase 3
- mRNA:
-
Messenger ribonucleic acid
- NOS:
-
Newcastle-Ottawa Quality Assessment Scale
- NOS :
-
Gene encoding nitric oxide synthases
- OCEBM:
-
Oxford Centre for Evidence-based Medicine levels of evidence
- OR:
-
Odds ratio
- PICO:
-
Patient Intervention, Comparison, Outcome
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- SNP:
-
Single nucleotide polymorphism
- TG:
-
Triglycerides
- TGFB1 :
-
Gene encoding transforming growth factor-β1
- TIMP:
-
Tissue inhibitor of metalloproteinases
- TNC :
-
Gene encoding tenascin-C
- TNFRSF1A :
-
Tumour necrosis factor receptor 1 gene
- TNFα:
-
Tumour necrosis factor-alpha
- VISA-A questionnaire:
-
Victorian Institute of Sport Assessment-Achilles questionnaire
- VNTR:
-
Variable number tandem repeat
References
Jarvinen TA, Kannus P, Maffulli N, Khan KM. Achilles tendon disorders: etiology and epidemiology. Foot Ankle Clin. 2005;10(2):255–66.
Padhiar N, Acharya N, Chan R, Davinii K, Crisp T, King J, et al. Achilles tendinopathy. Part 1—Pathophysiology and clinical features. SportEX Medicine. 2010;45:23–30.
Maffulli N. Overuse tendon conditions: time to change a confusing terminology. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 1998;14(8):840–3.
Maffulli N, Sharma P, Luscombe KL. Achilles tendinopathy: aetiology and management. Journal Of The Royal Society Of Medicine. 2004;97(10):472–6.
Kader D, Saxena A, Movin T, Maffulli N. Achilles tendinopathy: some aspects of basic science and clinical management. Br J Sports Med. 2002;36(4):239.
Khan KM, Bonar F, Desmond PM, Cook JL, Young DA, Visentini PJ, et al. Patellar tendinosis (jumper’s knee): findings at histopathologic examination, US, and MR imaging. Victorian Institute of Sport Tendon Study Group. Radiology. 1996;200(3):821–7.
Scott A, Khan K, Cook J, Duronio V. What is “inflammation”? Are we ready to move beyond Celsus? Br J Sports Med. 2004;38(3):248–9.
Abate M, Silbernagel KG, Siljeholm C, Di Iorio A, De Amicis D, Salini V, et al. Pathogenesis of tendinopathies: inflammation or degeneration? Arthritis Res Ther. 2009;11(3):235.
Cook J, Rio E, Purdam C, Docking S. Revisiting the continuum model of tendon pathology: what is its merit in clinical practice and research? British journal of sports medicine. 2016:bjsports-2015-095422.
Fu S-C, Rolf C, Cheuk Y-C, Lui PP, Chan K-M. Deciphering the pathogenesis of tendinopathy: a three-stages process. BMC Sports Science, Medicine and. Rehabilitation. 2010;2(1):30.
Cook J, Purdam CR. Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. Br J Sports Med. 2009;43(6):409–16.
Kvist M. Achilles tendon injuries in athletes. Ann Chir Gynaecol. 1991;80(2):188–201.
Kvist M. Achilles tendon injuries in athletes. Sports Med. 1994;18(3):173–201.
Lorimer A, Hume P. Achilles tendon injury risk factors associated with running. Sports Med. 2014;44(10):1459–72.
Dias Lopes A, Hespanhol Junior LC, Yeung SS, Pena Costa LO. What are the main running-related musculoskeletal injuries? Sports Med. 2012;42(10):891–905.
Gaida JE, Cook JL, Bass SL. Adiposity and tendinopathy. Disability & Rehabilitation. 2008;30(20-22):1555–62.
Lewis T, Cook J. Fluoroquinolones and tendinopathy: a guide for athletes and sports clinicians and a systematic review of the literature. Journal of Athletic Training (Allen Press). 2014;49(3):422–7.
Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions: Wiley Online Library. 2008.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–9.
GA Wells BS, D O'Connell, J Peterson, V Welch, M Losos, P Tugwell. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 200 [cited 3 March 2016]; Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Sara H, Downs NB. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–84.
Jeremy Howick ICJLL, Paul Glasziou, Trish Greenhalgh, Carl Heneghan, Alessandro Liberati, Ivan Moschetti, Bob Phillips, Hazel Thornton, Olive Goddard and Mary Hodgkinson. The Oxford levels of evidence 2. 2008 [cited; Available from: http://www.cebm.net/index.aspx?o=5653
Abrahams Y, Laguette MJ, Prince S, Collins M. Polymorphisms within the COL5A1 3′-UTR that alters mRNA structure and the MIR608 gene are associated with Achilles tendinopathy. Ann Hum Genet. 2013;77(3):204–14.
El Khoury L, Posthumus M, Collins M, Handley CJ, Cook J, Raleigh SM. Polymorphic variation within the ADAMTS2, ADAMTS14, ADAMTS5, ADAM12 and TIMP2 genes and the risk of Achilles tendon pathology: a genetic association study. J Sci Med Sport. 2013;16(6):493–8.
Hay M, Patricios J, Collins R, Branfield A, Cook J, Handley CJ, et al. Association of type XI collagen genes with chronic Achilles tendinopathy in independent populations from South Africa and Australia. Br J Sports Med. 2013;47(9):569–74.
Mokone GG, Gajjar M, September AV, Schwellnus MP, Greenberg J, Noakes TD, et al. The guanine-thymine dinucleotide repeat polymorphism within the tenascin-C gene is associated with achilles tendon injuries. Am J Sports Med. 2005;33(7):1016–21.
Mokone GG, Schwellnus MP, Noakes TD, Collins M. The COL5A1 gene and Achilles tendon pathology. Scand J Med Sci Sports. 2006;16(1):19–26.
Nell EM, Van Der Merwe L, Cook J, Handley CJ, Collins M, September AV. The apoptosis pathway and the genetic predisposition to Achilles tendinopathy. J Orthop Res. 2012;30(11):1719–24.
Posthumus M, Collins M, Cook J, Handley CJ, Ribbans WJ, Smith RKW, et al. Components of the transforming growth factor-β family and the pathogenesis of human achilles tendon pathology—a genetic association study. Rheumatology. 2010;49(11):2090–7.
Saunders CJ, Van Der Merwe L, Posthumus M, Cook J, Handley CJ, Collins M, et al. Investigation of variants within the COL27A1 and TNC genes and Achilles tendinopathy in two populations. J Orthop Res. 2013;31(4):632–7.
Raleigh SM. Variants within the MMP3 gene are associated with Achilles tendinopathy: possible interaction with the COL5A1 gene. Br J Sports Med. 2009;43(7):514–20.
September AV, Nell E-M, O'Connell K, Cook J, Handley CJ, Merwe L, et al. A pathway-based approach investigating the genes encoding interleukin-1β, interleukin-6 and the interleukin-1 receptor antagonist provides new insight into the genetic susceptibility of Achilles tendinopathy. Br J Sports Med. 2011;45(13):1040–7.
September AV. Variants within the COL5A1 gene are associated with Achilles tendinopathy in two populations. Br J Sports Med. 2009;43(5):357–65.
September AV, Posthumus M, Van Der Merwe L, Schwellnus M, Noakes TD, Collins M. The COL12A1 and COL14A1 genes and Achilles tendon injuries. Int J Sports Med. 2008;29(3):257–63.
El Khoury L, Posthumus M, Collins M, van der Merwe W, Handley C, Cook J, et al. ELN and FBN2 gene variants as risk factors for two sports-related musculoskeletal injuries. Int J Sports Med. 2015;36(4):333–7.
Brown KL, Seale KB, El Khoury LY, Posthumus M, Ribbans WJ, Raleigh SM, et al. Polymorphisms within the COL5A1 gene and regulators of the extracellular matrix modify the risk of Achilles tendon pathology in a British case-control study. Journal Of Sports Sciences. 2016;35(15):1-9.
Gibbon A, Hobbs H, van der Merwe W, Raleigh SM, Cook J, Handley CJ, et al. The MMP3 gene in musculoskeletal soft tissue injury risk profiling: a study in two independent sample groups. Journal Of Sports Sciences. 2016;35(7):655-662.
El Khoury L, Ribbans WJ, Raleigh SM. MMP3 and TIMP2 gene variants as predisposing factors for Achilles tendon pathologies: attempted replication study in a British case-control cohort. Meta Gene. 2016;9:52–5.
Rickaby R, El Khoury L, Ribbans WJ, Raleigh SM. Variation within three apoptosis associated genes as potential risk factors for Achilles tendinopathy in a British based case-control cohort. Gene. 2015;571(2):167–71.
Owens BD, Wolf JM, Seelig AD, Jacobson IG, Boyko EJ, Smith B, et al. Risk factors for lower extremity tendinopathies in military personnel. Orthopaedic Journal of Sports Medicine. 2013;1(1):1–8.
Abate M, Salini V, Schiavone C. Achilles tendinopathy in elderly subjects with type II diabetes: the role of sport activities. Aging Clin Exp Res. 2015;28(2):355-358.
Longo UG, Rittweger J, Garau G, Radonic B, Gutwasser C, Gilliver SF, et al. No influence of age, gender, weight, height, and impact profile in Achilles tendinopathy in masters track and field athletes. Am J Sports Med. 2009;37(7):1400–5.
Gaida JE, Alfredson L, Kiss ZS, Wilson AM, Alfredson H, Cook JL. Dyslipidemia in achilles tendinopathy is characteristic of insulin resistance. Med Sci Sports Exerc. 2009;41(6):1194–7.
Gaida JE, Alfredson H, Kiss ZS, Bass SL, Cook JL. Asymptomatic Achilles tendon pathology is associated with a central fat distribution in men and a peripheral fat distribution in women: a cross sectional study of 298 individuals. BMC Musculoskelet Disord. 2010;11:41.
Group OLoEW. The Oxford 2011 levels of evidence. Oxford, UK: Oxford centre for evidence-based medicine; 2011.
Abate M, Oliva F, Schiavone C, Salini V. Achilles tendinopathy in amateur runners: role of adiposity (tendinopathies and obesity). Muscles, Ligaments And Tendons Journal. 2012;2(1):44–8.
Tilley BJ, Cook JL, Docking SI, Gaida JE. Is higher serum cholesterol associated with altered tendon structure or tendon pain? A systematic review. British journal of sports medicine. 2015:bjsports-2015-095100.
Wright AF. Genetic variation: polymorphisms and mutations. Wiley Online Library. 2005.
Maffulli N, Reaper JA, Waterston SW, Ahya R. ABO blood groups and Achilles tendon rupture in the Grampian region of Scotland. Clin J Sport Med. 2000;10(4):269–71.
Leppilahti J, Puranen J, Orava S. ABO blood group and Achilles tendon rupture. Ann Chir Gynaecol. 1995;1995:369–71.
Rickert M, Wang H, Wieloch P, Lorenz H, Steck E, Sabo D, et al. Adenovirus-mediated gene transfer of growth and differentiation factor-5 into tenocytes and the healing rat Achilles tendon. Connect Tissue Res. 2005;46(4-5):175–83.
Mansfield JC, Holden H, Tarlow JK, Di Giovine FS, McDowell TL, Wilson AG, et al. Novel genetic association between ulcerative colitis and the anti-inflammatory cytokine interleukin-1 receptor antagonist. Gasrtoenterology-Baltimore then Philadelphia. 1994;106:637-.
Langdahl BL, Løkke E, Carstens M, Stenkjær LL, Eriksen EF. Osteoporotic fractures are associated with an 86‐base pair repeat polymorphism in the interleukin‐1‐receptor antagonist gene but not with polymorphisms in the interleukin‐1β gene. J Bone Miner Res. 2000;15(3):402–14.
Olofsson PS, Sheikine Y, Jatta K, Ghaderi M, Samnegård A, Eriksson P, et al. A functional interleukin-1 receptor antagonist polymorphism influences atherosclerosis development. The interleukin-1 beta: interleukin-1 receptor antagonist balance in atherosclerosis. Circ J. 2009;73(8):1531–6.
Landvik NE, Hart K, Skaug V, Stangeland LB, Haugen A, Zienolddiny S. A specific interleukin-1B haplotype correlates with high levels of IL1B mRNA in the lung and increased risk of non-small cell lung cancer. Carcinogenesis. 2009;30(7):1186–92.
Fishman D, Faulds G, Jeffery R, Mohamed-Ali V, Yudkin JS, Humphries S, et al. The effect of novel polymorphisms in the interleukin-6 (IL-6) gene on IL-6 transcription and plasma IL-6 levels, and an association with systemic-onset juvenile chronic arthritis. J Clin Investig. 1998;102(7):1369.
Namipashaki A, Razaghi-Moghadam Z, Ansari-Pour N. The essentiality of reporting Hardy-Weinberg equilibrium calculations in population-based genetic association studies. Cell Journal (Yakhteh). 2015;17(2):187.
Scotia N. Explaining odds ratios. J Can Acad Child Adolesc Psychiatry. 2010;19:227.
Gaida JE, Bagge J, Purdam C, Cook J, Alfredson H, Forsgren S. Evidence of the TNF-α system in the human Achilles tendon: expression of TNF-α and TNF receptor at both protein and mRNA levels in the tenocytes. Cells Tissues Organs. 2012;196(4):339–52.
Porter AG, Jänicke RU. Emerging roles of caspase-3 in apoptosis. Cell Death Differ. 1999;6(2):99–104.
Funding
Funding is provided by the Collaborative Research Network for Advancing Exercise & Sports Science (CRN-AESS).
Authors’ Contributions
MK contributed to the conception and design of the review and analysis and interpretation of the results and drafted the manuscript. NV contributed to the conception and design of the review, analysis and draft revision. KA contributed to the critical revision of the manuscript. DH contributed to the critical revision of the manuscript. All authors read and approved the final manuscript.
Competing Interests
Maria Kozlovskaia, Nicole Vlahovich, Kevin Ashton and David Hughes have no conflict of interest.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kozlovskaia, M., Vlahovich, N., Ashton, K. et al. Biomedical Risk Factors of Achilles Tendinopathy in Physically Active People: a Systematic Review. Sports Med - Open 3, 20 (2017). https://doi.org/10.1186/s40798-017-0087-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40798-017-0087-y