Abstract
Background
Safety is of vital importance for lung resection. The dissection of pulmonary vessels is associated with vascular injury and bleeding, and identification of the vessels is necessary. The most common abnormal branching pattern of the left pulmonary artery is the mediastinal lingular artery. However, a mediastinal basal pulmonary artery is very rare. A case of abnormal branching from the left pulmonary artery to S8 which was diagnosed intraoperatively, and, thus, its dissection was avoided, is reported.
Case presentation
A 76-year-old woman with rheumatoid arthritis was diagnosed with left upper lung adenocarcinoma and visited our hospital. Contrast CT was not performed due to renal dysfunction, and abnormal branching of the left pulmonary artery was not identified. Video-assisted thoracoscopic left upper lobectomy and lymphadenectomy were performed. After the upper pulmonary vein was dissected and tissue around it was detached carefully, a pulmonary mediastinal branch from the left main pulmonary artery was identified descending between the upper pulmonary vein and upper bronchus. It was possible to separate the interlobar fissure safely and preserve A8. On retrospective examination, non-contrast CT showed A8.
Conclusions
Although preoperative identification of left pulmonary mediastinal branches was difficult by non-contrast CT, a careful surgical procedure preserved the left pulmonary mediastinal A8.
Similar content being viewed by others
Background
In lung resection, safety is vitally important. In particular, dissection of pulmonary vessels is associated with vascular injury and bleeding, and identification of the vessels is necessary. The most common abnormal branching pattern of the left pulmonary artery is the mediastinal lingular artery. However, a mediastinal basal pulmonary artery is very rare. A case of abnormal branching from the left pulmonary artery to S8 that was diagnosed intraoperatively and its dissection was avoided is reported.
Case presentation
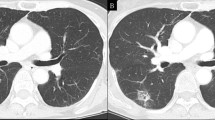
The patient was a 76-year-old woman with rheumatoid arthritis. Computed tomography (CT) had been performed for a medical checkup, and a small nodule was detected in the left upper lobe (S1+2) a year before she visited our hospital. Follow-up CT showed that the nodule with indentation was growing to 22 mm in size, and she was referred to a nearby hospital (Fig. 1). Fluorodeoxyglucose (FDG)-positron emission tomography (PET), brain magnetic resonance imaging, and transbronchial biopsy were performed, showing left upper lung adenocarcinoma classified as cT1bN0M0 Stage IA according to the Union for International Cancer Control classification (seventh edition). Though contrast-enhanced three-dimensional computed tomographic angiography (3DCT) of the pulmonary vessels was usually performed to identify the pulmonary branches preoperatively at that time, it was not performed in the present case due to renal dysfunction, and abnormal branching of the left pulmonary artery was not identified. Video-assisted thoracoscopic left upper lobectomy and lymphadenectomy were performed. A1+2c, the upper pulmonary vein, mediastinal A4+5, A3, and A1+2a+b were detached carefully and dissected. Before separation of the interlobar fissure was completed, a pulmonary mediastinal branch from the left main pulmonary artery was identified descending between the upper pulmonary vein and upper bronchus. The interlobar fissure was separated safely with preservation of A8 (Figs. 2 and 3). On retrospective examination, non-contrast CT showed A8 (Fig. 4).
Conclusions
An abnormal pulmonary branch can induce unexpected bleeding, and careful surgery is needed to dissect the branch to the preserved lobe. The number of left pulmonary branches varies from two to seven, and variations may occur in all segments. Generally, the first anterior branch supplies the lingular division in less than 10% of cases [1]. Recently, lingular artery branching patterns have been reported, with mediastinal origin in 9.2%, interlobar and mediastinal origin in 26.9%, and interlobar origin in 63.9%. Furthermore, 8 of 23 cases with mediastinal lingular artery were overlooked intraoperatively [2]. However, a branch from the first left pulmonary branch to the basal segment is rare.
It is possible that even the operator is not able to recognize a mediastinal lingular artery. Therefore, the possibility of missing a mediastinal basal lung artery is high. A total of 14 cases on the left side were reported only in Japan, including the present case (Table 1) [2,3,4,5,6,7,8,9,10,11,12,13,14,15].
It is possible to identify a basal lung artery preoperatively by contrast-enhanced CT or 3DCT. However, it has been reported that it was not diagnosed by non-contrast CT. In the present case, the mediastinal basal lung artery was identified intraoperatively, though it was difficult to diagnose it preoperatively. Therefore, the discreet separation of the vessel and bronchus is very important. Retrospectively, CT showed the mediastinal basal artery, although the interpretation was difficult; careful CT reading is also important.
3DCT is useful to identify the running condition of the pulmonary vessels preoperatively. However, contrast medium should be avoided when there is renal dysfunction, allergy, and so on. On the other hand, 3DCT without contrast medium has been reported to have slightly poorer resolution but may be helpful [16]. Actually, we constructed 3DCT of our case using non-contrast CT retrospectively (Fig. 5). It was necessary to spend several hours to make this image because it was difficult to distinguish artery from vein without contrast medium. The surface of pulmonary artery may be jagged; however, it helps to comprehend pulmonary pattern of branching.
In conclusion, although preoperative identification of left pulmonary mediastinal branches was difficult on non-contrast CT, a careful surgical procedure preserved the left pulmonary mediastinal A8.
Abbreviations
- 3DCT:
-
Three-dimensional computed tomographic angiography
- CT:
-
Computed tomography
- FDG-PET:
-
Fluorodeoxyglucose-positron emission tomography
References
Shields TW. Surgical anatomy of the lungs. In: Shields TW, LoCicero 3rd J, Reed CE, Feins RH, editors. General thoracic surgery. 7th ed. Philadelphia: Lippincott Williams & Wilkins; 2009. p. 79.
Nagata T, Nakamura Y, Kariatsumari K, Otsuka T, Aoki M, Sato M. Potentially overlooked branches of the left pulmonary artery. Asian Cardiovasc Thorac Ann. 2016;24:676–80.
Bamba J, Tomoyasu H, Tanimura S, Masaki M. Abnormal branching of the left pulmonary artery to the lateral and posterior basal segments. Nihon Kyobu Geka Gakkai Zasshi. 1985;33:366–8.
Iwabuchi S, Okabe T, Koike K. Aberrant ramuts of left pulmonary artery to inferior lingular and anterior basal segment (A5+8). Jpn J Chest Surg. 1995;9:159–63.
Sano M, Mizuno T, Iizuka M, Yamada T, Kasugai T, Ishiguro H. Abnormal branching of left pulmonary artery to the lateral and posterior basal segments. Nihon Kyobu Geka Gakkai Zasshi. 1996;44:1772–5.
Moriyama S, Miyoshi K, Tada A, Kurosaki T. A case report of abnormal branching of left A8+9 pulmonary artery. Jpn J Chest Surg. 2009;23:58–61.
Kataoka K, Nishikawa T, Fujiwara T, Matsuura M. A case of lung cancer with an extremely rare branching pattern of the left A5+8+9+10 pulmonary artery. Haigan. 2010;50:362–5.
Sueda T, Takami K, Omiya H, Kodama Y, Kuriyama K, Tsujinaka T. A case of abnormal branching of the left anterobasal pulmonary artery with primary lung cancer. J Jpn Surg Assoc. 2011;72:630–5.
Kaneda Y, Samura M, Kanayama Y, Okazaki M, Noshima S, Zempo N. A case of abnormal branching of the left A9 pulmonary artery from the left main pulmonary artery. J Jpn Surg Assoc. 2012;73:1920–3.
Kozu Y, Maniwa T, Isaka M, Ohde Y, Kondo H, Endo M. A case of abnormal branching of A5 and A8b as a common trunk from the left main pulmonary artery. Jpn J Chest Surg. 2012;26:772–5.
Matsumoto K, Yamasaki N, Tsuchiya T, Miyazaki T, Tomoshige K, Hayashi H, et al. Three-dimensional computed tomography for a mediastinal basal pulmonary artery. Ann Thorac Surg. 2012;94:e115–6.
Kato H, Oizumi H, Inoue T, Watarai H. A case report of lung cancer with abnormal branching of the left A8 pulmonary artery detected during left upper lobectomy. Haigan. 2014;54:6–11.
Yajima K, Neyatani H, Takahashi T. A resected case of left upper lung cancer with A4, A5, A9 and A10 arising as a common trunk from the left main pulmonary artery. Haigan. 2014;54:84–8.
Kawai N, Kawaguchi T, Yasukawa M, Tojo T. Two cases of lower lobectomy with mediastinal inferior lobar branch in lung cancer. Jpn J Chest Surg. 2015;29:786–91.
Sonoda D, Mikubo M, Shiomi K, Satoh Y. Abnormal branching of the left lingular pulmonary artery diagnosed by three-dimensional computed tomographic angiography in a patient with lung cancer: a case report. J Cardiothorac Surg. 2016;11:17.
Watanabe S, Arai K, Watanabe T, Koda W, Urayama H. Use of three-dimensional computed tomographic angiography of pulmonary vessels for lung resections. Ann Thorac Surg. 2003;75:388–92.
Availability of data and materials
Data sharing is not applicable to this article, as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Contributions
YM performed surgery, carried out the acquisition of data, and drafted the manuscript. NU and HA proofread the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The patient provided informed consent for the publishing.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Mizukami, Y., Ueda, N. & Adachi, H. Intraoperative diagnosis with abnormal branching of the left A8 pulmonary artery from the left main pulmonary artery. surg case rep 4, 68 (2018). https://doi.org/10.1186/s40792-018-0475-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-018-0475-7