Abstract
Background
Extramedullary plasmacytomas account for 4% of all plasma cell tumors and occur mainly in the upper respiratory tract; gastrointestinal system involvement is rare. Extramedullary plasmacytoma of the colon with perforation has not been reported.
Case presentation
A 77-year-old woman with a 1-year history of lower abdominal pain and nausea was admitted to our hospital. An abdominal computed tomography scan revealed a sigmoid tumor with perforation. The patient underwent emergency surgery. Pathological examination led to a diagnosis of plasmacytoma of the colon. The patient did not undergo postoperative adjuvant chemotherapy. She has had no recurrence in 14 months of regular follow-up.
Conclusions
We have herein described a rare case of extramedullary plasmacytoma of the gastrointestinal tract with perforation involving the sigmoid colon.
Similar content being viewed by others
Background
A plasma cell tumor is an immunoproliferative monoclonal disease of the B cell line that originates from malignant transformed plasma cells. Plasmacytoma includes solitary plasmacytoma of bone and solitary extramedullary plasmacytoma.
Solitary extramedullary plasmacytoma has been rarely reported, and its natural history and diagnosis are unclear. Most such plasmacytomas occur in the nasopharynx or upper respiratory tract; only 10% of reported cases have involved the gastrointestinal tract. The stomach and small intestine are the most commonly involved sites in the gastrointestinal tract [1,2,3]. Primary isolated extramedullary plasmacytoma of the colon is extremely rare. No previous reports have described plasmacytoma of the colon with perforation. We herein report a rare case of primary isolated extramedullary plasmacytoma of the colon with perforation and describe the patient’s postoperative clinical course.
Case presentation
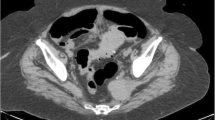
A 77-year-old woman with a 1-year history of lower abdominal pain and nausea was admitted to our hospital. Blood examination showed evidence of an inflammatory response (Table 1), and abdominal computed tomography revealed a sigmoid tumor with perforation (Fig. 1). We suspected sigmoid cancer with perforation, and the patient underwent emergency surgery. Open laparotomy revealed an extensive mass involving the sigmoid colon with surrounding contamination (Fig. 2). The abdominal mass was removed en bloc, including resection of the sigmoid colon. The abdomen was flushed to remove contamination. An artificial anus was made.
Histopathologic examination showed that the oval mass was composed of a diffuse proliferation of plasma cells (Fig. 3a). At the concavity of the site of the perforation showed the tumor cell infiltrated into the subserosa and necrosis of tissue. But we were unable to identify the site of the perforation pathologically. The surgical margins were free from tumor cells. Immunohistochemical examination revealed positivity for CD79a (Fig. 3b), immunoglobulin G, and lambda light chain (Fig. 4a, b). Other markers (CD10, CD20, and kappa light chain) were negative (Fig. 4c). Pathological examination led to a diagnosis of plasmacytoma of the colon. The patient underwent bone marrow biopsy and bone imaging to exclude associated multiple myeloma. Her peripheral blood smear, serum protein electrophoresis, and urine immunoelectrophoresis for Bence-Jones protein were normal.
Postoperatively, the patient was discharged without any complications. She did not undergo postoperative adjuvant chemotherapy and has had no recurrence in 14 months of regular follow-up.
Discussion
Extramedullary plasmacytoma accounts for only 3 to 5% of all plasma cell diseases. These tumors may be solitary or may precede, accompany, or follow the onset of multiple myeloma. Solitary extramedullary plasmacytoma has rarely been reported, and its natural history and diagnosis are unclear. Diagnosis of solitary extramedullary plasmacytoma requires the exclusion of associated multiple myeloma, which is determined by the absence of Bence-Jones protein in the urine, normal serum electrophoresis, and normal bone marrow biopsy [4]. Our present case met these criteria.
Alexiou et al. [5] reported that extramedullary plasmacytoma most often occurs in the nasopharynx or upper respiratory tract (82.2%). Only 17.8% of cases involve the gastrointestinal tract. The stomach and small intestine are the most commonly involved sites in the gastrointestinal tract. Primary isolated extramedullary plasmacytoma of the colon is extremely rare, occurring in only 0.028% of cases [5]. Therefore, its clinical features and prognosis are not well known.
The clinical presentation of extramedullary plasmacytoma of the colon is variable and may include abdominal pain, intestinal bleeding, and diarrhea. Gabriel and Savu [6] reported a rare case in which an extramedullary plasmacytoma was found with ileocecal junction perforation secondary to colonoscopic injury. This is the only previous report to describe extramedullary plasmacytoma with gastrointestinal perforation (Table 2).
In the present case, we were unable to determine the cause of the perforation by pathologic examination. We consider that the tumor was necrosed and perforated; otherwise, as the tumor grew, the intestinal internal pressure increased, resulting in perforation of the sigmoid colon.
Postoperative chemotherapy has no effect on the course of extramedullary plasmacytoma. Our patient did not undergo postoperative adjuvant chemotherapy, and she has had no relapse to date. However, careful follow-up is required.
Because primary isolated extramedullary plasmacytoma in the colon is very rare, the clinical course, treatment guidelines, and prognosis remain unclear. Further study of the clinical features of primary isolated extramedullary plasmacytoma of the colon is necessary to ensure that adequate treatment is administered.
Conclusions
We have described a rare case of extramedullary plasmacytoma of the gastrointestinal tract with perforation of the sigmoid colon. In this case, the prognosis was good because of appropriate treatment involving early surgery.
References
Liebross RH, Ha CS, Cox JD, Weber D, Delasalle K, Alexanian R. Clinical course of solitary extramedullary plasma. Radiother Oncol. 1999;52:245–9. https://doi.org/10.1016/S0167-8140899900114-0.
Hampton JM, Gandy JR. Plasmacytoma of the gastro-intestinal tract. Ann Surg. 1957;145:415–22.
Asselah F, Crow J, Slavin G, Sowter G, Sheldon C, Asselah H. Solitary plasma of the intestine. Histopathology. 1982;6:631–45.
Meritt JW Jr. Plasmacytoma of gastrointestinal tract. Ann Surg. 1955;142:881–8.
Alexiou C, Kau RJ, Dietzfelbinger H, Kremer M, Spiess JC, Schratzenstaller B, et al. Extramedullary plasmacytoma: tumor occurrence and therapeutic concepts. Cancer. 1999;85:2305–14.
Gabriel EM, Savu M. Discovery of a rare ileocecal plasmacytoma. J Surg Case Rep 2014(3):rju016. doi:https://doi.org/10.1093/jscr/rju016.
Acknowledgements
The authors would like to thank Angela Morben, DVM, ELS, from Edanz Group (www.edanzediting.com/ac) for editing a draft of this manuscript.
Funding
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
FK wrote the final manuscript and performed the literature search. KD supervised the writing of the manuscript. HI and TO performed the surgery. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Written informed consent was obtained from the patient for the publication of this report and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kitamura, F., Doi, K., Ishiodori, H. et al. Primary extramedullary plasmacytoma of the sigmoid colon with perforation: a case report. surg case rep 4, 28 (2018). https://doi.org/10.1186/s40792-018-0437-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40792-018-0437-0