Abstract
Background
Many studies have evaluated associations between asthma emergency department (ED) visits, hospital admissions (HAs), and ambient ozone (O3) across the US, but not in Texas. We investigated the relationship between O3 and asthma HAs, and the potential impacts of outdoor pollen, respiratory infection HAs, and the start of the school year in Texas.
Methods
We obtained daily time-series data on asthma HAs and ambient O3 concentrations for Dallas, Houston, and Austin, Texas for the years 2003–2011. Relative risks (RRs) and 95% confidence intervals (CIs) of asthma HAs per 10-ppb increase in 8-h maximum O3 concentrations were estimated from Poisson generalized additive models and adjusted for temporal trends, meteorological factors, pollen, respiratory infection HAs, day of the week, and public holidays. We conducted a number of sensitivity analyses to assess model specification.
Results
We observed weak associations between total asthma HAs and O3 at lags of 1 day (RR10 ppb = 1.012, 95% CI: 1.004–1.021), 2 days (RR10 ppb = 1.011, 95% CI: 1.002–1.019), and 0–3 days (RR10 ppb = 1.017, 95% CI: 1.005–1.030). The associations were primarily observed in children aged 5–14 years (e.g., for O3 at lag 0–3 days, RR10 ppb = 1.037, 95% CI: 1.011–1.064), and null in individuals 15 years or older. The effect estimates did not change significantly with adjustment for pollen and respiratory infections, but they attenuated considerably and lost statistical significance when August and September data were excluded. A significant interaction between time around the start of the school year and O3 at lag 2 day was observed, with the associations with pediatric asthma HAs stronger in August and September (RR10 ppb = 1.040, 95% CI: 1.012–1.069) than in the rest of the year (October–July) (RR10 ppb = 1.006, 95% CI: 0.986–1.026).
Conclusions
We observed small but statistically significant positive associations between total and pediatric asthma HAs and short-term O3 exposure in Texas, especially in August and September. Further research is needed to determine how the start of school could modify the observed association between O3 and pediatric asthma HAs.
Similar content being viewed by others
Background
Asthma is a chronic lung disease characterized by inflammation and narrowing of the conducting airways. Acute exacerbations can be triggered by a variety of factors, including stress, physical exertion, airborne allergens, respiratory infections, and both indoor and outdoor air pollutants [1, 2]. Asthma exacerbations can be life-threatening if not treated and are one of the most common causes of emergency department (ED) visits and hospital admissions (HAs) in the US.
Numerous time-series and case-crossover epidemiology studies have been conducted to evaluate whether incidence rates of asthma ED visits and HAs increase following short-term increases in regional ozone (O3) concentrations. These studies have been conducted in a variety of locations across North America, and include analyses of ED visits for asthma in New York City [3], Atlanta [4], Seattle [5], and Canada [6, 7], and analyses of asthma HAs in New York City [8] and Seattle [9]. Most of these studies reported small, statistically significant elevations of population-average ED visits and HAs for asthma in the days following elevated O3 levels, and some evidence indicates that certain groups are more susceptible to O3 exposure, including children [8] and the elderly [10].
In Texas, where O3 is monitored on a year-round basis, O3 levels have sometimes exceeded the National Ambient Air Quality Standard (NAAQS) in Dallas-Fort Worth, Houston-Galveston-Brazoria, and Austin areas from 2003 to 2011 [11]. For example, in 2009–2011, the annual fourth highest daily maximum 8-h average O3 concentrations at the majority of monitoring sites in the Dallas-Fort Worth and Houston-Galveston areas exceeded the then-current O3 NAAQS of 75 parts per billion (ppb). Between 2007 and 2010, Dallas County and Harris County also reported the highest number of HAs for asthma in Texas [12].
Despite elevated O3 concentrations and the relatively high burden of asthma in Dallas and Houston, to our knowledge, no studies have measured associations between daily O3 exposure and either HAs or ED visits for asthma in any regions of Texas. Thus, we conducted a time-series study of ambient O3 and HAs for asthma in Dallas, Houston, and Austin, the three metropolitan areas for which pollen data are available, with stratification by patient age, to determine whether associations vary with age. Because time-series analyses of short-term effects of air pollution can be confounded by time-varying factors associated with both exposure and outcome, we aimed to thoroughly investigate several potential factors known to affect the risk of asthma exacerbations, including outdoor pollen and other aeroallergens, respiratory infection HAs, and – for children – the return to school in August and September. Finally, our analytic approach included a rigorous assessment of model specification, as previous research has demonstrated that results of time-series studies are sensitive to statistical modeling approaches [13, 14].
Methods
Hospital admission data
We obtained daily hospital discharge data from 2003 to 2011 from the Texas Department of State Health Services (TDSHS), for patients who were hospitalized in emergency or urgent care departments in Houston, Dallas, or Austin with a primary diagnosis of asthma (International Classification of Disease, 9th Revision [ICD-9] code 493). Because asthma diagnoses in younger children are not reliable [15], we excluded patients who were younger than 5 years old.
Our study was reviewed and approved by the TDSHS Institutional Review Board (IRB).
Ambient ozone data
The Texas Commission on Environmental Quality (TCEQ) maintains ambient air monitoring stations, where ambient O3 concentrations are monitored year round. We obtained ambient O3 monitoring data from 2003 to 2011 for three metropolitan areas – Dallas (8 monitoring sites), Houston (44 monitoring sites), and Austin (6 monitoring sites) – from TCEQ. We calculated site-specific daily maximum 8-h moving average O3 concentrations and averaged over all sites within each area to obtain area-specific daily average 8-h maximum O3 concentrations over the entire time period.
Meteorological data
We obtained daily mean temperatures and daily dew point temperatures, which were also measured at air monitoring stations, for the same time period and areas from TCEQ. We calculated area-level daily averages of these meteorological variables.
Pollen data
The National Allergen Bureau (NAB), a section of the American Academy of Allergy, Asthma and Immunology (AAAAI), provides aeroallergen levels from a network of counting stations throughout the US. We obtained the data on daily total pollen and aeroallergen counts from the Allergy and Asthma Center in Georgetown (Austin) from NAB, and we obtained the data for Dallas (ENTDocs Ear, Nose, Throat & Allergy Testing & Treatment in Plano; Family Allergy and Asthma Care in Flower Mound) and Houston (Station 2) directly from the individual stations. Because there are no data available for weekends and holidays, we imputed the missing values as described by Gleason et al. [16]. Briefly, a day with missing pollen counts was assigned the pollen counts from the previous day for up to three consecutive days with missing values. If there were more than three consecutive days with missing pollen values, the remainder of the days were given the pollen value from the succeeding day.
Statistical analysis
Based on patient residential zip code, we aggregated individual-level data to metropolitan area-level daily counts of total asthma HAs, as well as asthma HAs for three specific age groups (5–14 years, 15–64 years, and 65 years and older) in Houston, Dallas, and Austin.
We used a Poisson Generalized Additive model to estimate the relative risks (RRs) and 95% confidence intervals (CIs) for asthma HAs associated with a 10-ppb increase in ambient O3 concentrations at various lags, including single-day lags from current day to six days prior (lag 0, 1, 2, 3, 4, 5, and 6), and multiple-day lags of day 0 to 3 days prior (lag 0–3) and day 0 through six days prior (lag 0–6). For each area, we included the natural logarithm of population size as an offset term and the counts of asthma HAs in the previous four days as covariates to account for autocorrelations in the dependent variable. We adjusted for temporal trend, immediate and delayed effects of meteorological factors, day of the week, and public holidays. We combined the area-specific effect estimates using a random effects model. No significant overdispersion was observed in the time-series data.
The main model is:
where.
E(Y t ) = the expected count of asthma HAs on day t.
Pop j = the total population of the jth area
Ozone t = the O3 concentrations on day t
DOW t = the categorical variable with seven levels specifying the day of the week on day t
Holiday t = the indicator variable specifying whether day t is a federal holiday
Area j = a random intercept for area j
ns(time t , 8 df/year) = a cubic spline function of time with eight knots per year to control for temporal trends
ns(Temp lag0t , 3) = a cubic spline function of the current-day average temperature with 3 degrees of freedom
ns(Temp lag13t , 3) = a cubic spline function of the average of lag 1 through 3 day temperature with 3 degrees of freedom
ns(Dew lag0t , 3) = a cubic spline function of the current-day dew point with 3 degrees of freedom
ns(Dew lag13t , 3) = a cubic spline function of the average of lag 1 through 3 day dew point with 3 degrees of freedom
Y t − 1, Y t − 2, Y t − 3, and Y t − 4 = lag 1, lag 2, lag 3, and lag 4 day of asthma HA counts on day t.
We evaluated pollen levels as a potential confounder for the O3-asthma association. Daily pollen counts were added into the main model in different forms. First, we created a categorical variable (0, <25th percentile, ≥25th percentile and <50th percentile, ≥50th percentile and <75th percentile, ≥75th percentile). Second, we log-transformed daily pollen counts to improve normality (Additional file 1 Fig. S1) and included log(pollen counts) in the model as a linear term. Third, we used the cubic spline of daily pollen counts with 3 degrees of freedom. Similar approaches were used for aeroallergen counts (Additional file 1 Fig. S2). We evaluated various lags of pollen and aeroallergen counts, including same day (lag 0), previous day (lag 1), two days prior (lag 2), and the average of 0 to 2 days prior (lag 0–2). Because there are two counting stations for Dallas, we used the data from the Plano station in the main analysis and the data from the Flower Mound station for sensitivity analyses.
In addition to pollen, we also evaluated whether respiratory infection HAs would confound the association between ambient O3 and asthma HAs. We identified patients with primary diagnoses of respiratory infections (pneumonia, ICD-9 codes 480–486; upper respiratory infection, ICD-9 codes 460–465; influenza, ICD-9 code 487) and generated area-level daily counts of total respiratory infections. We evaluated the short-term effect of respiratory infection HAs by adding the same-day total respiratory infection HAs (lag 0) and the average of lag 0 through 2 day total respiratory infection HAs (lag 0–2) into the model as either a linear covariate or cubic splines with 3 degrees of freedom.
We also examined whether the start of the school year would impact the association between ambient O3 and asthma HAs. We first excluded days from August and September and estimated risks of total asthma HAs and pediatric asthma HAs for children aged 5 to 14 years. We also created an indicator variable for the two months of August and September and included the indicator variable and/or the product terms of this indicator variable and the O3 variables in regression models to evaluate confounding and effect modification.
We conducted a series of sensitivity analyses to examine whether specifications of models and covariates impact the results. First, pollen data from the Flower Mound station, instead of Plano, were used for Dallas. Second, we used different degrees of freedom per year for the temporal splines. Third, we used different degrees of freedom splines of temperature and dew point. To evaluate whether the model would give rise to spurious associations, we conducted two sensitivity analyses: 1) including O3 concentrations at lag −1 day in the model, and 2) using a health endpoint that is unrelated to ambient air pollution (acute appendicitis, ICD-9 code 540) as the dependent variable. Last, we repeated all analyses with total aeroallergen (pollen and mold) counts instead of pollen counts. Only two metropolitan areas, Dallas and Houston, were included in this sensitivity analysis because data on mold were not available for Austin.
All statistical analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC).
Results
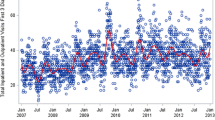
There were a total of 74,824 asthma HAs in Dallas, Houston, and Austin, Texas from 2003 to 2011, which included 16,879 patients 5 to 14 years of age (mean ± standard deviation [SD]: 1.7 ± 2.0 daily visits), 40,991 who were 15 to 64 years of age (4.2 ± 3.0 daily visits), and 16,954 who were 65 years of age or older (1.7 ± 1.6 daily visits). The mean area-level 8-h maximum ambient O3 concentration for all three metropolitan areas was 41.8 ppb. Daily pollen counts were on average about 300, with a wide range from 0 to over 30,000. The average temperature was 68.1 °F (range: 16.6–97.7), and the average dew point temperature was 55.1 °F (range: 6–76.8). Correlations between these factors were generally weak but highly statistically significant. O3 appeared to be positively correlated with temperature (r = 0.3) and pollen counts (r = 0.2), and negatively correlated with asthma HAs (r = −0.1). Descriptive statistics and pairwise correlations for asthma HAs, ambient O3, pollen, and meteorological factors are presented in Tables 1 and 2. Among the three metropolitan areas, ambient O3 concentrations and meteorological factors were comparable, but Dallas had lower average daily pollen counts than Austin and Houston (Additional file 1 Table S1).
Adjusted RRs for total and age-specific asthma HAs per 10-ppb increase in ambient O3 concentrations at various lags are presented in Table 3. For total asthma HAs, the association with same-day 8-h maximum O3 concentrations was null (RR = 1.007; 95% CI: 0.998–1.015). Total asthma HAs were positively associated with O3 concentrations the previous day (lag 1) (RR = 1.012; 95% CI: 1.004–1.021) and two days prior (lag 2) (RR = 1.011; 95% CI: 1.002–1.019), and with the average of O3 concentrations 0 to 3 days prior (lag 0–3) (RR = 1.017; 95% CI: 1.005–1.030). The effect of O3 on pediatric asthma HAs was stronger, with statistically significant associations observed for all three single-day lags (O3 at lag 0 day: RR = 1.027, 95% CI: 1.008–1.047; lag 1 days: RR = 1.025, 95% CI: 1.007–1.043; lag 2 day: RR = 1.019, 95% CI: 1.001–1.038) and the multiple-day lag (O3 at lag 0–3 days: RR = 1.037, 95% CI: 1.011–1.064). In contrast, O3 was not statistically significantly associated with asthma HAs in patients aged 15 years or older for most lag periods. Total and age-specific asthma HAs were generally not statistically significantly associated with O3 concentrations at more than two days prior to the outcome, i.e., lag 3, 4, 5, 6 day and lag 0–6 days(Additional file 1 Table S2).
We evaluated daily pollen levels and total respiratory infection HAs as potential confounders for the associations between ambient O3 concentrations and total and pediatric asthma HAs (Table 4). Adjustment for daily pollen counts alone (Model 2), or in combination with total respiratory infection HAs (Model 3), did not impact the effect estimates for O3 in any meaningful way. The generally null associations between ambient O3 concentrations and asthma HAs for patients aged 15 years or older were not changed with the adjustment for pollen counts and total respiratory infection HAs (data not shown). Using a linear term, categorical variables, or cubic splines to specify pollen counts had little impact on the risk estimates of O3 (Additional file 1 Table S3). Using pollen data from a different counting station for Dallas also did not change the results significantly (Additional file 1 Table S4). Pollen counts and total respiratory infection HAs expressed with a linear term, as a categorical variable, or cubic splines at various lags were evaluated, but the observed confounding effects by these two factors were minimal at all lags (Additional file 1 Table S5). Using total aeroallergen counts instead of pollen counts did not result in any greater changes in the risk estimates for O3 (Additional file 1 Table S6).
We also considered the impact of the start of the school year on the observed associations between ambient O3 and total and pediatric asthma HAs (Table 4). Excluding data from August and September, the RRs for O3 and total asthma HAs were attenuated and generally did not remain statistically significant. Similarly, associations between O3 and pediatric asthma HAs became null when data around the start of school year were excluded from the analyses.
We further evaluated whether the time period around the start of school year confounded and/or modified the associations between pediatric asthma HAs and ambient O3 concentrations (Table 5). Inclusion of an indicator variable for the two months of August and September resulted in only minimal changes in the risk estimates for ambient O3 concentrations, suggesting that this time period did not confound the observed association between pediatric asthma HAs and ambient O3. Results from Model 3 show that the effect estimates of ambient O3 concentrations at lag 2 day were considerably stronger in August and September (RR = 1.040, 95% CI: 1.012–1.069) than those in the rest of the year (October–July) (RR = 1.006, 95% CI: 0.986–1.026). The interactions, however, were not significant for same-day concentrations (pinteraction = 0.24), previous-day concentrations (pinteraction = 0.75), and concentrations at lag 0–3 days (pinteraction = 0.12). This finding suggests that the association between pediatric asthma HAs and ambient O3 at lag 2 day was modified by the time period around the start of the school year.
Finally, we conducted a series of sensitivity analyses regarding model and covariate specifications. We found that the results were not sensitive to increased degrees of freedom in cubic splines of temperature and dew point (Additional file 1 Table S7). We also evaluated whether assuming 4, 8, or 12 degrees of freedom in the temporal splines impacted results for all ages combined or specific age categories, and for lags of 0, 1, 2, and 0–3 days. We found that effect estimates for O3 were higher when assuming 4 degrees of freedom vs. 8, but the results were similar for 8 and 12 degrees of freedom (Additional file 1 Table S8). O3 concentrations at lag −1 day were not associated with asthma HAs (Additional file 1 Table S9), nor were acute appendicitis HAs associated with ambient O3 levels (Additional file 1 Table S10), indicating that the main model did not give rise to spurious associations.
Discussion
In an all-year time-series analysis of ambient O3 and asthma HAs in three major metropolitan regions of Texas, we found small, statistically significant increases in daily rates of total asthma HAs one to 3 days following elevated O3 levels. Associations were strongest for the 5- to 14-year-old age group, but null for people over the age of 14. The observed effects of ambient O3 on asthma HAs in school-age children appeared to be stronger in the time period around the start of school year (August and September) but were null in the rest of the year (October–July). In sensitivity analyses, we evaluated whether the strength and precision of estimates varied with differences in model specification, and we found that our results were robust to most variations. It is unknown whether any such model misspecification would affect the validity of associations at shorter lags.
Only a few studies have evaluated O3 and asthma exacerbations in Texas. In a study of lifeguards in the Galveston area, Thaller et al. [17] reported that short term O3 exposure was associated with a reduced ratio of forced expiratory volume in one second to forced vital capacity (FEV1/FVC), with a greater decrease observed for individuals with asthma (change = −0.6, p < 0.05) than nonasthmatics (change = −0.4, p < 0.01). Zora et al. [18], however, reported that O3 was not associated with worsened control of asthma in El Paso, Texas (change in asthma control questionnaire score = 0.006, p = 0.9). Raun et al. [19] conducted a study of ambient O3 and ambulance-treated asthma attacks in Houston and reported a small elevation in asthma events associated with a 20-ppb increase in O3 concentrations at lag 0–2 days (RR = 1.07, 95% CI: 1.03–1.11). These studies varied considerably with regard to methodology and asthma exacerbation endpoints, and reported inconsistent results. The association between ambient O3 concentrations and emergency/urgent care asthma HAs observed in our study was similar to the findings of Raun et al. [19], likely due to the similarity between the asthma exacerbation endpoints evaluated.
It is notable that our results are quantitatively similar to those of other time-series and case-crossover investigations of ambient O3 and asthma ED visits and HAs conducted in locations across the world. Recently, Zheng et al. [20] conducted a systematic review of all published epidemiology analyses of this topic; pooling the results of 71 studies in a meta-analysis, Zheng et al. [20] estimated a meta-RR of 1.018 (95% CI: 1.013, 1.023) per 10-ppb increase in O3 for individuals of all ages. This is comparable to the magnitude of associations with total asthma HAs we observed in our main analyses.
In addition to our core analysis, a primary objective of our investigation was to determine whether observed associations between O3 and rates of asthma HAs were affected by various time-varying factors that could confound ecological relationships between air pollution and respiratory health. Because any true associations between air pollution and health are small in absolute magnitude, residual or unmeasured confounding can strongly impact the accuracy of study results [14]. In contrast to observational study designs in which individual-level health, exposure, and covariate data are collected (i.e., panel studies or prospective cohort studies), time-series studies are ecological in design and information on potential confounders is not available for specific individuals. Typically, confounding by time-varying factors is addressed in time-series analyses using flexible splines of calendar time, presumed to act as surrogates for potential confounders that vary on long to moderate time frames, on the order of months, seasons, or years [21].
We assessed whether the association between O3 and asthma was affected by accounting for the “September effect,” a spike in rates of asthma exacerbations for school-age children that occurs following the beginning of each new school year [22]. Researchers have ascribed this increase in asthma exacerbations to a variety of factors, including stress [22] or exposure to respiratory viruses [23], and some time-series analyses of pediatric asthma exclude the period at the beginning of the school year to avoid confounding by this factor [3]. Excluding August and September from our analysis substantially affected our results (effect estimates were strongly attenuated and less precise). Further evaluation revealed that the time period around the start of school year was not a confounder, but an effect modifier for the observed associations between ambient O3 and asthma HAs among school-age children. Effects of O3 appeared to be stronger in August and September compared to the rest of the year. This interaction observed in our study suggests that children are more susceptible to O3 during this period (perhaps because of stress or increased viral infections).
We also explored the possibility that observed associations between O3 and asthma hospitalizations were confounded by exposure to airborne pollen. Previous research indicates that increased regional concentrations of outdoor aeroallergens are associated with increases in numerous outcomes related to respiratory morbidity, including asthma ED visits [16, 24,25,26] and asthma hospitalizations [27]. If daily O3 concentrations are even slightly correlated with ambient pollen concentrations, measured associations between O3 and asthma exacerbations could be confounded. Correlation coefficients between measured O3 and pollen for a particular study region may not reflect the direction or magnitude of true correlation in the case that either measurement is affected by random measurement error.
To address the hypothesis that asthma-O3 associations were confounded by ambient pollen, we adjusted for concentrations of outdoor pollen measured at regional stations up to two days prior to the date of outcome. We observed minimal impact on the associations between O3 and daily asthma HAs for any age group. Based on this finding alone, however, we cannot rule out the possibility that outdoor pollen and other aeroallergens are confounders for the O3-asthma association. We used pollen counts measured at stations in Houston, Dallas, and Austin to estimate exposures in the study population, but this approximation may poorly reflect actual pollen exposures. Pollen exposures generally exhibit a high degree of spatial variability across a region and, as a result, the concentrations from local stations may be poor surrogates for true exposure. In addition, airborne pollen is a highly heterogeneous mixture. Only sensitized individuals are likely to experience respiratory effects on days of elevated pollen levels, and, furthermore, the risk of respiratory effects for each sensitized individual varies strongly by type of pollen, because different individuals are sensitized to one or more types of pollen. Therefore, the ecological design of our study, as well as the measurement error associated with estimates of pollen exposure, may limit our model’s ability to accurately account for any true confounding by pollen that may exist. In addition, the shape of the dose-response relationship between pollen exposure and asthma exacerbations, on either the population or individual level, is unknown; one recent analysis indicated that the associations between ambient pollen and respiratory health varies strongly by the form of the pollen covariate included in statistical models [24]. Thus, our finding of limited confounding by pollen in our study region may have occurred because pollen exposure is incorrectly specified in our models.
Similarly, we pursued the hypothesis that confounding could occur in time-series studies of O3 and asthma due to the very strong association between respiratory infections and asthma exacerbations. For example, viral infections are the single most important trigger of pediatric asthma exacerbations, estimated to cause over 80% of acute exacerbations [28]. Panel studies and time-series studies of air pollution and asthma have presented some evidence that respiratory infections may confound observed associations [4, 29]. We assessed evidence for any such confounding in our study population by adding adjustment variables derived from daily counts of HAs for respiratory infections. Specifically, we varied lag relationships and functional forms for total respiratory infection HAs for inclusion in statistical models. We observed little evidence that respiratory HAs confounded relationships between O3 and total and pediatric asthma HAs in Texas. Previous studies have shown that specific viruses increase risk of asthma exacerbations while others viruses do not [30]. Because respiratory infection HAs were only a crude proxy measure of individual exposure to respiratory infections, our analyses cannot rule out confounding by respiratory infections completely.
There are several strengths of our investigation that should be considered when interpreting our results, including the large sample size in our analysis and the use of area-specific monitoring data to estimate daily O3 exposures to populations living in different areas of the study region. We explored confounding by pollen, respiratory infection HAs, and the start of the school year, using an alternative approach to adjusting for flexible functions of calendar time, which is the approach typically used to approximate seasonal changes in time-varying confounders. We also rigorously assessed the robustness of our model specification, including an analysis evaluating the associations between asthma HAs occurring the day before O3 exposure [31] and a negative control analysis, in which we evaluated whether acute appendicitis was associated with O3 [32]. Results of these sensitivity analyses did not provide evidence for model misspecification; however, these sensitivity analyses cannot completely rule out all forms of model misspecification. The fact that our analyses for extended lag periods consistently indicated a statistically significant decrease in asthma HAs six days following an increase in ambient O3 supports the potential for model misspecification, because it is unlikely that O3 truly protects against asthma exacerbations six days later.
In addition to the uncertainties in model specification and in estimating true exposure to airborne pollen and respiratory infections, additional limitations in our time-series approach should be acknowledged. Like many other time-series studies, we estimated daily O3 exposure using measurements from central site monitors in each metropolitan area, and these estimates may vary substantially from true O3 exposures in the study population. The resultant exposure measurement error could be classical and/or Berkson in nature, biasing effect estimates and standard errors in directions that are difficult to predict [33]. Additional data collection would be needed to characterize the precise effect of this error on epidemiology associations; for example, a personal exposure study could be conducted to quantify how well central site monitor measurements predict personal exposure. Similarly, measurement errors are also likely present in the meteorological data. In addition, our analysis did not account for any potential confounding by co-pollutants, such as particulate matter less than 2.5 μm in diameter, that may be correlated with O3 in this study area.
Conclusions
We observed weak, positive associations between ambient O3 and asthma HAs in Texas, with the strongest effects among school-age children. However, these associations varied significantly during the year, with the strongest associations observed at the beginning of the school year, a period of large increases in pediatric asthma exacerbations. Further research is needed to determine whether this effect modification occurs in other time-series analyses of pediatric asthma and air pollution.
Abbreviations
- AAAAI:
-
American Academy of Allergy, Asthma and Immunology
- CI:
-
Confidence Interval
- ED:
-
Emergency Department
- FEV1 :
-
Forced Expiratory Volume in One Second
- FVC:
-
Forced Vital Capacity
- HA:
-
Hospital Admission
- ICD-9:
-
International Classification of Disease, 9th Revision
- IRB:
-
Institutional Review Board
- NAAQS:
-
National Ambient Air Quality Standard
- NAB:
-
National Allergen Bureau
- O3 :
-
Ozone
- Ppb:
-
Parts Per Billion
- RR:
-
Relative Risk
- SD:
-
Standard Deviation
- TCEQ:
-
Texas Commission on Environmental Quality
- TDSHS:
-
Texas Department of State Health Services
- US:
-
United States
References
Barnes PJ. 2008. Asthma. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, Loscalzo J, editors. Harrison's principles of internal medicine. 17th ed. New York: McGraw-Hill Medical; 2008. p. 1596–607.
Mayo Clinic. Asthma. 2012. http://www.mayoclinic.org/diseases-conditions/asthma/basics/definition/CON-20026992. Accessed 14 Jan 2014.
Ito K, Thurston GD, Silverman RA. Characterization of PM2.5, gaseous pollutants, and meteorological interactions in the context of time-series health effects models. J Expo Sci Environ Epidemiol. 2007;17(Suppl. 2):S45–60.
Strickland MJ, Darrow LA, Klein M, Flanders WD, Sarnat JA, Waller LA, et al. Short-term associations between ambient air pollutants and pediatric asthma emergency department visits. Am J Respir Crit Care Med. 2010;182(3):307–16.
Mar TF, Koenig JQ. Relationship between visits to emergency departments for asthma and ozone exposure in greater Seattle. Washington Ann Allergy Asthma Immunol. 2009;103:474–9.
Stieb DM, Szyszkowicz M, Rowe BH, Leech JA. Air pollution and emergency department visits for cardiac and respiratory conditions: a multi-city time-series analysis. Environ Health. 2009;8:25.
Villeneuve PJ, Chen L, Rowe BH, Coates F. Outdoor air pollution and emergency department visits for asthma among children and adults: a case-crossover study in northern Alberta. Canada Environ Health. 2007;6:40.
Silverman RA, Ito K. Age-related association of fine particles and ozone with severe acute asthma in new York City. J Allergy Clin Immunol. 2010;125(2):367–73.
Sheppard L, Levy D, Norris G, Larson TV, Koenig JQ. Effects of ambient air pollution on nonelderly asthma hospital admissions in Seattle, Washington, 1987-1994. Epidemiology. 1999;10(1):23–30.
Ji M, Cohan DS, Bell ML. Meta-analysis of the association between short-term exposure to ambient ozone and respiratory hospital admissions. Environ Res Lett. 2011; doi: 10.1088/1748-9326/6/2/024006.
Texas Commission on Environmental Quality (TCEQ). Compliance with eight-hour ozone standard. 2016. https://www.tceq.texas.gov/cgi-bin/compliance/monops/8hr_attainment.pl. Accessed 11 Aug 2016.
Texas Dept. of State Health Services (TDSHS). Prevalence, mortality, and hospitalization rates due to asthma by county and public health region, Texas, 2004–2010. Texas Asthma Control Program, Report to Texas Commission on Environmental Quality (TCEQ). 2012; October 11. https://www.dshs.texas.gov/WorkArea/linkit.aspx?LinkIdentifier=id&ItemID=8589984799.
Bell ML, Samet JM, Dominici F. Time-series studies of particulate matter. Annu Rev Public Health. 2004;25:247–80.
Lumley T, Sheppard L. Assessing seasonal confounding and model selection bias in air pollution epidemiology using positive and negative control analyses. Environmetrics. 2000;11:705–17.
Mayo Clinic. Childhood asthma. 2013. http://www.mayoclinic.org/diseases-conditions/childhood-asthma/basics/tests-diagnosis/con-20028628. Accessed 25 Feb 2015.
Gleason JA, Bielory L, Fagliano JA. Associations between ozone, PM2.5, and four pollen types on emergency department pediatric asthma events during the warm season in New Jersey: a case-crossover study. Environ Res. 2014; doi: 10.1016/j.envres.2014.03.035.
Thaller EI, Petronella SA, Hochman D, Howard S, Chhikara RS, Brooks EG. Moderate increases in ambient PM2.5 and ozone are associated with lung function decreases in beach lifeguards. J Occup Environ Med. 2008;50(2):202–11.
Zora JE, Sarnat SE, Raysoni AU, Johnson BA, Li WW, Greenwald R, et al. Associations between urban air pollution and pediatric asthma control in El Paso, Texas. Sci Total Environ. 2013; doi: 10.1016/j.scitotenv.2012.11.067.
Raun LH, Ensor KB, Persse D. Using community level strategies to reduce asthma attacks triggered by outdoor air pollution: a case crossover analysis. Environ Health 2014; doi: 10.1186/1476-069X-13-58.
Zheng XY, Ding H, Jiang LN, Chen SW, Zheng JP, Qiu M, et al. Association between air pollutants and asthma emergency room visits and hospital admissions in time series studies: a systematic review and meta-analysis. PLoS ONE 2015; doi: 10.1371/journal.pone.0138146.
Armstrong B, Gasparrini A. Time series regression analysis. 2014. http://csm.lshtm.ac.uk/themes/time-series-regression-analysis. Accessed 22 Sept 2014.
Silverman RA, Ito K, Stevenson L, Hastings HM. The relationship of fall school opening and emergency department asthma visits in a large metropolitan area. Arch Pediatr Adolesc Med. 2005;159(9):818–23.
Eggo RM, Scott JG, Galvani AP, Meyers LA. Respiratory virus transmission dynamics determine timing of asthma exacerbation peaks: evidence from a population-level model. Proc Natl Acad Sci U S A. 2016; doi:10.1073/pnas.1518677113.
Ito K, Weinberger KR, Robinson GS, Sheffield PE, Lall R, Mathes R, et al. The associations between daily spring pollen counts, over-the-counter allergy medication sales, and asthma syndrome emergency department visits in New York City, 2002–2012. Environ Health 2015; doi: 10.1186/s12940-015-0057-0.
Jariwala S, Toh J, Shum M, de Vos G, Zou K, Sindher S, et al. The association between asthma-related emergency department visits and pollen and mold spore concentrations in the Bronx, 2001–2008. J Asthma 2014; doi: 10.3109/02770903.2013.853779.
Zhong W, Levin L, Reponen T, Hershey GK, Adhikari A, Shukla R, et al. Analysis of short-term influences of ambient aeroallergens on pediatric asthma hospital visits. Sci Total Environ. 2006; doi: 10.1016/j.scitotenv.2006.06.019.
Dales R, Liu L, Wheeler AJ, Gilbert NL. Quality of indoor residential air and health. CMAJ. 2008;179:147–52.
Busse WW, Lemanske RF Jr., Gern JE. Role of viral respiratory infections in asthma and asthma exacerbations. Lancet 2010; doi: 10.1016/S0140-6736(10)61380-3.
Rabinovitch N, Zhang L, Murphy JR, Vedal S, Dutton SJ, Gelfand EW. Effects of wintertime ambient air pollutants on asthma exacerbations in urban minority children with moderate to severe disease. J Allergy Clin Immunol. 2004;114(5):1131–7.
Khetsuriani N, Kazerouni NN, Erdman DD, Lu X, Redd SC, Anderson LJ, et al. Prevalence of viral respiratory tract infections in children with asthma. J Allergy Clin Immunol. 2007; doi: 10.1016/j.jaci.2006.08.041.
Peel JL, Tolbert PE, Klein M, Metzger KB, Flanders WD, Todd K, et al. Ambient air pollution and respiratory emergency department visits. Epidemiology. 2005;16(2):164–74.
Lumley T, Sheppard L. Time series analyses of air pollution and health: straining at gnats and swallowing camels? Epidemiology. 2003;14(1):13.
Zeger SL, Thomas D, Dominici F, Samet JM, Schwartz J, Dockery D, et al. Exposure measurement error in time-series studies of air pollution: concepts and consequences. Environ Health Perspect. 2000;108(5):419–26.
Acknowledgments
We acknowledge NAB, AAAAI, and the following people and pollen stations for providing the pollen and aeroallergen data: Dr. Sheila Amar at Allergy & Asthma Center of Georgetown (Austin area); Dr. Jeffrey Adelglass at ENTDocs Ear, Nose, Throat & Allergy Testing & Treatment in Plano (Dallas area); Dr. Marie Fitzgerald at Family Allergy and Asthma Care in Flower Mound (Dallas area); and Mr. Tony Huynh at Station 2 in Houston. We thank Dr. Stephanie Shirley and Ms. Hailey Hyde of TCEQ for their help conditioning the pollen and aeroallergen data. We also thank Dr. Mara Seeley for contributions to the IRB submission, Mr. Shuo Zhao for contributions to conditioning the ozone data, Dr. Thuy Lam for reviewing SAS code, and Ms. Carla Walker for editing the manuscript.
Funding
Through a consulting contract between Gradient and the Texas Commission on Environmental Quality (TCEQ), Gradient staff have provided scientific consulting services to TCEQ on matters related to ambient ozone and health risks. The work reported in this paper was supported by the TCEQ work orders 582–13–32,032-06 (PCR No. 42658) and 582–15–51,942-02 (PCR No. 62741).
Availability of data and materials
The datasets generated during and/or analyzed during the current study are not publicly available because hospital admission data are confidential. But the datasets are available from the corresponding author on reasonable request with permission from the Texas Department of State Health Services Institutional Review Board.
Author information
Authors and Affiliations
Contributions
JEG designed the study and was a major contributor in writing the manuscript. KZ obtained the data on hospital admissions, ozone, and meteorological factors, contributed to the statistical analyses, and was a major contributor to writing the manuscript. CTL was a major contributor to the statistical analyses and writing the manuscript. GT conditioned raw data and generated analytical datasets, and was a major contributor to the statistical analyses. XL conducted the statistical analyses and was a major contributor to writing the manuscript. SL obtained the pollen and aeroallergen data, and was a major contributor to writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The work reported in this paper involved human data. We obtained ethics approval from the Texas Department of State Health Services (TDSHS) Institutional Review Board #1 (IRB# 14–059). We did not obtain informed consent because we used de-identified hospital admissions data collected by TDSHS.
Consent for publication
Not applicable.
Competing interests
The authors are current (JEG, KZ, XL) and former (GT, CTL) employees of Gradient, an independent environmental and risk science consulting firm, in Cambridge, Massachuestts, and a current employee (SL) of the Texas Commission on Environmental Quality (TCEQ). The work reported in this paper was conducted by the authors during the normal course of their employment, and the authors have the sole responsibility for the analysis, writing, content, and conclusions in this article. The conclusions are not necessarily those of TCEQ.
JEG, KZ, and CTL have provided written and/or oral comments to the US Environmental Protection Agency (EPA) and/or the EPA Clean Air Scientific Advisory Committee (CASAC) on various NAAQS documents of criteria air pollutants. JEG, KZ, and CTL have also authored review articles and/or conducted original research on the health effects associated with ambient air pollutants. GT, XL, and SL do not have any conflicts or competing interests, either financial or non-financial.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1: Fig. S1.
Histograms of pollen counts. A. Original data. B. Log-transformed data. Fig. S2 Histograms of aeroallergen counts. A. Original data. B. Log-transformed data. Table S1 Descriptive statistics of asthma HAs, ambient O3, pollen, and meteorological factors in Dallas, Houston, and Austin, Texas, from 2003 to 2011. Table S2 Associationsa between asthma HAs and ambient O3 concentrations in Dallas, Houston, and Austin, Texas, from 2003 to 2011. Table S3 Associationsa between asthma HAs and ambient O3 concentrations, with adjustment for pollen, in Dallas, Houston, and Austin, Texas, from 2003 to 2011. Table S4 Associations between asthma HAs and ambient O3 concentrations, with adjustment for pollen using alternative dataa for Dallas. Table S5 Associations between asthma HAs and ambient O3 concentrations, with adjustments for pollen and respiratory infection HAs, in Dallas, Houston, and Austin, Texas, from 2003 to 2011. Table S6 Results of asthma HAs per 10 ppb increase in O3 concentrations, with adjustment for aeroallergen, in Dallas and Houston, Texas, from 2003 to 2011. Table S7 Sensitivity analyses with different specifications of temperature and dew point . Table S8 Sensitivity analysesa with different specifications of temporal trend. Table S9 Sensitivity analysesa with O3 concentrations at lag −1 day. Table S10 Associationsa between acute appendicitis HAs and ambient O3 in Dallas, Houston, and Austin, Texas, from 2003 to 2011. (XLSX 95 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Goodman, J.E., Zu, K., Loftus, C.T. et al. Ambient ozone and asthma hospital admissions in Texas: a time-series analysis. asthma res and pract 3, 6 (2017). https://doi.org/10.1186/s40733-017-0034-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40733-017-0034-1