Abstract
Human immunodeficiency virus (HIV) still poses enigmatic threats to human life. This virus has mastered in bypassing anti retroviral therapy leading to patients’ death. Circulating viruses are phenomenal for the disease outcome. This hypothesis proposes a therapeutic strategy utilizing receptor-integrated hematopoietic, erythroid and red blood cells. Here, HIV specific receptors trap circulating viruses that enter erythrocyte cytoplasm and form inactive integration complex. This model depicts easy, effective removal of circulating HIV without any adverse effect.
Similar content being viewed by others
Background
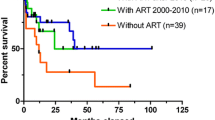
Having around 36 years of understanding after its discovery [1], scientists are still haunting a full and effective cure for human immunodeficiency virus (HIV) and its outcome acquired immunodeficiency syndrome (AIDS). Till date thousands of research efforts have revealed plethora of information regarding its life cycle [2,3,4,5,6,7,8] that characterized enigmatic AIDS. These immense knowledge provided possible targets for AIDS therapy [3,4,5, 8,9,10,11] that intervene entry, replication, packaging or budding of the virus leading to anti-retroviral therapy (ART) [12,13,14,15,16,17]. Apart from having diverse side-effects, ART has certain limitations too, as it only delays patients’ death but does not cure AIDS and also it only targets replicating HIVs and not the latent viral particles. Moreover, in doing so, it evokes successive immune compromising reactions making the situation worse. Circulating replicative HIV remains the biggest threat toward successful AIDS therapy. Therefore, an effective strategy is essential that can confer resistance towards circulating HIV particles. If replicating HIV particles were somehow eliminated, it would greatly reduce the effective viral burden from human body. On the other hand, latency provide base for long term existence of HIV without eliciting any immune response hiding deep inside immune organs [18,19,20]. Very recently, other than anti-retroviral drugs, such as experimentally promising HIV vaccine [21], neutralizing antibodies [22,23,24] and Clustered regularly interspaced short palindromic repeat-CRISPR-associated protein-9 nuclease (CRISPR-Cas 9) have shown effectiveness against HIV [25, 26] with certain limitations [27].
The most fascinating event in the viral life cycle is that only a few viral proteins effectively control and direct the cellular pathways for their own sake. So, knowledge of viral proteins functioning in the virus life cycle and properly targeting them may confer successful elimination of HIV from human body.
Hypothesis
Previously transgenic mice showed effectiveness against Coxsackie virus B infection [28]. Here in this hypothesis, a therapeutic strategy has been proposed for AIDS treatment that would utilize bone marrow stem cells. The proposed therapeutic strategy exploits receptor-integrated red blood corpuscles (riRBC) to trap and finally kill the circulating HIVs. According to this model, RBC membranes can be loaded with cluster of differentiation 4 (CD4) receptor along with C-C chemokine receptor type 5 (CCR5) and C-X-C chemokine receptor type 4 (CXCR4) co-receptors [4, 6, 7] that will specifically bind circulating HIV particles. The whole process can be divided into four stages. Firstly, hematopoietic stem cells (HSC) can be collected from bone marrow of O-negative (O−/−) healthy person to negate possible future immune reaction. Then, these cells will be stably transduced or transfected with CD4, CCR5 and CXCR4 genes using highly efficient viral (retroviral, lentiviral etc.) [29,30,31] or non-viral (episomal) based vectors [32,33,34,35], cloned from TH-lymphocyte genome, under the control of GATA-1 promoter [36] which can be sorted using over-expressed HIV-receptors (Fig. 1). Secondly, after sorting the in vitro receptor-integrated HSCs (riHSC) will be subjected to treatment with different growth and transformation factors (GM-CSF, M-CSF, IL-3, SCF, TPO, FLT-3L, IL-11) in the medium to finally obtain receptor-integrated burst-forming unit-erythrocyte (riBFU-E) stem cell [37,38,39,40,41,42,43,44,45,46,47,48,49]. Moderate quantities of riBFU-Es will then be selected from the cell pool by FACS using CD45+GPA−IL-3R−CD34+CD36−CD71+-markers [50, 51] and the rest will be treated in the culture medium using EPO (erythropoietin) [39, 43, 47] to yield huge pool of mature erythrocytes or riRBC having membrane integrated CD4, CCR5 and CXCR4 (Fig. 2). Along with the growth factors, certain rejuvenating factors and strategies [52,53,54,55] will be employed throughout the in vitro process to curb stem cell aging which is an evident stem cell therapeutic problem [56]. Third step will employ a combination therapy by transfusing riRBCs along with the riBFU-E stem cells in the peripheral blood of AIDS patient.
HIV receptor integrated hematopoietic stem cell formation. Hematopoietic stem cells can be collected from healthy person having O-negative (O−/−) blood group. HIV receptor-CD4 and co-receptors-CCR5 and CXCR4 will then be transgenically introduced onto the hematopoietic stem cell membranes by stably transducing or transfecting HSC with receptor genes under GATA-1 promoter control to form riHSC using viral or non-viral vectors. These receptor positive stem cells will be sorted using HIV receptors for next treatment. HIV human immunodeficiency virus, HSC hematopoietic stem cell, CD4 cluster of differentiation 4, CCR5 C-C chemokine receptor type 5, CXCR4 C-X-C chemokine receptor type 4, riHSC receptor-integrated hematopoietic stem cell
In vitro formation of riBFU-E and mature riRBC from riHSC. The formed riHSC from the stem cells will then be treated with several in vitro growth and differentiation factors like GM-CSF, M-CSF, IL-3, SCF, TPO etc. to obtain BFU-E having HIV receptor-co-receptor complex. Then, these riBFU-E cells will be selected and isolated from other cell lineages by FACS using CD45+GPA−IL-3R−CD34+CD36−CD71+ markers to finally yield pool of pure riBFU-E cells. Another large population of cells having mixed population of riBFU-E and other lineages like lymphoid and myeloid cells will be treated by EPO to finally obtain only mature riRBC. GM-CSF granulocytemacrophage colony stimulating factor, M-CSF macrophage colony-stimulating factor, IL-3 interleukin-3, IL-11 interleukin-11, SCF stem cell factor, TPO thrombopoietin, FLT-3L Fms-related tyrosine kinase 3 ligand, CMP common myeloid progenitor, MEP megakaryocyte/erythrocyte progenitor, BFU-E burst forming unit-erythroid, riRBC receptor integrated red blood corpuscle, FACS fluorescence-activated cell sorting, riBFU-E receptor integrated burst forming unit-erythroid, EPO erythropoietin
Soon after transfusion the riBFU-Es will find its way to the bone marrow by ‘stem-cell homing’ [57,58,59,60] and once in the specific niche the engineered stem cell will proliferate to yield numerous riRBCs naturally from the bone marrow (Fig. 3). Bone marrow derived riRBCs along with the transfused riRBCs in the peripheral blood will then engage in receptor mediated capturing of circulating HIV particles. The fascinating feature of this engineered riRBC is that a single riRBC can confine numerous HIV particles till its natural destruction after 120 days in patient’s body. Once circulating HIVs bind with the receptor and co-receptor associated complex on the riRBC membrane by its envelop glycoproteins gp 120 and gp 41, viral membrane will readily fuse with cell membrane leading to partial core shell uncoating and entry into riRBC cytoplasm [4, 6]. This event would immediately facilitate reverse transcription of genomic HIV-RNA to yield pre-integration complex (PIC) [4, 6, 11, 61]. Up to this event HIV follows its normal path of infection but once PIC has been formed inside riRBC cytoplasm, due to the lack of nucleus it will be unable to complete its replication and life cycle and eventually will stall. Single riRBC will carry numerous of such PICs and eventually be destroyed along with the riRBC by the action of macrophagic lytic enzymes in the spleen [62]. According to this hypothesis the proposed therapeutic strategy will greatly reduce the HIV burden from the AIDS patient abruptly, and effectively (Fig. 4).
Combination therapy to transfuse riBFU-E and riRBC into HIV-positive patient. riBFU-E and riRBCs will be transfused into peripheral blood of HIV patients as combination therapeutic strategy. Once inside patients’ body, riRBCs will be immediately functional to counter circulating HIV particles. On the other hand, riBFU-E from the peripheral blood will find its way to the bone marrow by stem cell homing and will normally differentiate into riRBC that will further amplify the efficiency of the therapy. riRBCs receptor integrated red blood corpuscles, riBFU-E receptor integrated burst forming unit-erythroid
Trapping HIVs within riRBC and destroying them. Once in blood, the riRBCs will engage to bind free HIV particles by the interaction of viral glycoproteins gp 120 and gp 41 with its membrane embedded CD4, CCR5 and CXCR4. After attachment fusion of viral and riRBC membrane will result in uncoating of viral core contents within cell cytoplasm leading to reverse transcription using its own transcriptase to form PIC. A single riRBC will be able to trap numerous HIV-PIC. However, once PIC formed it will remain inert as it will hardly find any genome to integrate and finally will be destroyed along with aged riRBC in spleen. HIVs human immunodeficiency viruses, CD4 cluster of differentiation 4, CCR5 C-C chemokine receptor type 5, riRBC receptor integrated red blood corpuscle, PIC pre integration complex
Conclusions
The credentials of this hypothetical therapeutic strategy will be immense since (i) as the riHSC is a stem cell, once transduced cells are generated they will serve to produce riBFU-E and riRBC for a long period of time, (ii) riBFU-E as a stem cell will proliferate in the bone marrow for a long period of time to produce numerous riRBC naturally without forming lymphoid lineages of cells (modern improved techniques permit successful, efficient and enormous production of RBCs from HSCs [37,38,39,40,41,42,43,44,45,46,47,48,49] and this will enable successful large scale production of riRBCs), (iii) both the riBFU-E and riRBC cells will not elicit any immune reaction as the cells are immunologically non-reactive taken from healthy O−/− person and (iv) the HIV trapping riRBCs will remain effective for around 120 days to continuously carry out its function to entrap circulating viruses. Moreover, early findings of HIV binding to RBCs have been reported that remain bound by Duffy antigen receptor (DARC) and spread infection to T-cells [63,64,65,66]. These findings further strengthen the present method as in presence of overexpressed HIV binding receptors on riRBC, HIV particles will readily enter the cell for their dead end. Another concern may be with the proper alignment of overexpressed receptors facilitating HIV binding. But as T-cells derive from lymphoid lineage from HSCs, hence, it is expected that overexpressing CD4, CCR5 and CXCR4 receptor genes in HSCs will yield homologous receptor like on T cell for HIV binding under specific growth and differentiation factor influence.
Safety is a big issue in genetically modified therapy so, proper safety measures and precautions should be taken [67,68,69,70] and whole procedure must be critically followed to prevent any accidental transmission of modified stem cells. Finally, it should be noted that effective strategies must combine this one to cope up inactive hidden latent viruses to completely remove HIV from human body and these strategic riRBCs not only serve as a vehicle to fight HIV but little modification will enable it to battle numerous other infections too.
Abbreviations
- HIV:
-
human immunodeficiency virus
- HSC:
-
hematopoietic stem cell
- CD4:
-
cluster of differentiation 4
- CCR5:
-
C-C chemokine receptor type 5
- CXCR4:
-
C-X-C chemokine receptor type 4
- riHSC:
-
receptor-integrated hematopoietic stem cell
- GM-CSF:
-
granulocytemacrophage colony stimulating factor
- M-CSF:
-
macrophage colony-stimulating factor
- IL-3:
-
interleukin-3
- IL-11:
-
interleukin-11
- SCF:
-
stem cell factor
- TPO:
-
thrombopoietin
- FLT-3L:
-
Fms-related tyrosine kinase 3 ligand
- CMP:
-
common myeloid progenitor
- MEP:
-
megakaryocyte/erythrocyte progenitor
- BFU-E:
-
burst forming unit-erythroid
- riRBC:
-
receptor integrated red blood corpuscle
- FACS:
-
fluorescence-activated cell sorting
- riBFU-E:
-
receptor integrated burst forming unit-erythroid
- EPO:
-
erythropoietin
- riRBCs:
-
receptor integrated red blood corpuscles
- riBFU-E:
-
receptor integrated burst forming unit-erythroid
- HIVs:
-
human immunodeficiency viruses
- CD4:
-
cluster of differentiation 4
- CCR5:
-
C-C chemokine receptor type 5
- riRBC:
-
receptor integrated red blood corpuscle
- PIC:
-
pre integration complex
- DARC:
-
Duffy antigen receptor
References
Barré-Sinoussi F, Chermann JC, Rey F, Nugeyre MT, Chamaret S, Gruest J, et al. Isolation of a T-lymphotropic retrovirus from a patient at risk for acquired immune deficiency syndrome (AIDS). Science. 1983;220:868–71.
Barré-Sinoussi F, Ross AL, Delfraissy JF. Past, present and future: 30 years of HIV research. Nat Rev Microbiol. 2013;11:877–83.
Campbell EM, Hope TJ. HIV-1 capsid: the multifaceted key player in HIV-1 infection. Nat Rev Microbiol. 2015;13:471–83.
Engelman A, Cherepanov P. The structural biology of HIV-1: mechanistic and therapeutic insights. Nat Rev Microbiol. 2012;10:279–90.
Fackler OT, Murooka TT, Imle A, Mempel TR. Adding new dimensions: towards an integrative understanding of HIV-1 spread. Nat Rev Microbiol. 2014;12:563–74.
Freed EO. HIV-1 assembly, release and maturation. Nat Rev Microbiol. 2015;13:484–96.
Galvin SR, Cohen MS. The role of sexually transmitted diseases in HIV transmission. Nat Rev Microbiol. 2004;2:33–42.
Martin-Serrano J, Neil SJ. Host factors involved in retroviral budding and release. Nat Rev Microbiol. 2011;9:519–31.
Ayinde D, Casartelli N, Schwartz O. Restricting HIV the SAMHD1 way: through nucleotide starvation. Nat Rev Microbiol. 2012;10:675–80.
Doyle T, Goujon C, Malim MH. HIV-1 and interferons: who’s interfering with whom? Nat Rev Microbiol. 2015;13:403–13.
Malim MH, Bieniasz PD. HIV restriction factors and mechanisms of evasion. Cold Spring Harb Perspect Med. 2012;2:a006940.
Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365:493–505.
Kitahata MM, Gange SJ, Abraham AG, Merriman B, Saag MS, Justice AC, et al. Effect of early versus deferred antiretroviral therapy for HIV on survival. N Engl J Med. 2009;360:1815–26.
Maenza J, Flexner C. Combination antiretroviral therapy for HIV infection. Am Fam Physician. 1998;57:2789–98.
Palmisano L, Vella S. A brief history of antiretroviral therapy of HIV infection: success and challenges. Ann Ist Super Sanita. 2011;47:44–8.
Shen L, Peterson S, Sedaghat AR, McMahon MA, Callender M, Zhang H, et al. Dose-response curve slope sets class-specific limits on inhibitory potential of anti-HIV drugs. Nat Med. 2008;14:762–6.
Weller IV, Williams IG. ABC of AIDS. Antiretroviral drugs. BMJ. 2001;322:1410–2.
Archin NM, Sung JM, Garrido C, Soriano-Sarabia N, Margolis DM. Eradicating HIV-1 infection: seeking to clear a persistent pathogen. Nat Rev Microbiol. 2014;12:750–64.
Coiras M, López-Huertas MR, Pérez-Olmeda M, Alcamí J. Understanding HIV-1 latency provides clues for the eradication of long-term reservoirs. Nat Rev Microbiol. 2009;7:798–812.
Razooky BS, Pai A, Aull K, Rouzine IM, Weinberger LS. A hardwired HIV latency program. Cell. 2015;160:990–1001.
Barouch DH, Picker LJ. Novel vaccine vectors for HIV-1. Nat Rev Microbiol. 2014;12:765–71.
Dosenovic P, von Boehmer L, Escolano A, Jardine J, Freund NT, Gitlin AD, et al. Immunization for HIV-1 broadly neutralizing antibodies in human Ig knockin mice. Cell. 2015;161:1505–15.
Kwong PD, Mascola JR, Nabel GJ. Broadly neutralizing antibodies and the search for an HIV-1 vaccine: the end of the beginning. Nat Rev Immunol. 2013;13:693–701.
Wibmer CK, Moore PL, Morris L. HIV broadly neutralizing antibody targets. Curr Opin HIV AIDS. 2015;10:135–43.
Saayman SM, Lazar DC, Scott TA, Hart JR, Takahashi M, Burnett JC, et al. Potent and targeted activation of latent HIV-1 using the CRISPR/dCas9 activator complex. Mol Ther. 2016;24:488–98.
Wang Z, Pan Q, Gendron P, Zhu W, Guo F, Cen S, et al. CRISPR/Cas9-derived mutations both inhibit HIV-1 replication and accelerate viral escape. Cell Rep. 2016;15:481–9.
Wang G, Zhao N, Berkhout B, Das AT. CRISPR-Cas9 can inhibit HIV-1 replication but NHEJ repair facilitates virus escape. Mol Ther. 2016;24:522–6.
Damon R, Asher AMC, Robert WF. The erythrocyte viral trap: transgenic expression of viral receptor on erythrocytes attenuates coxsackievirus B infection. Proc Natl Acad Sci USA. 2005;102:12897–902.
Cao F, Xie X, Gollan T, Zhao L, Narsinh K, Lee RJ, et al. Comparison of gene-transfer efficiency in human embryonic stem cells. Mol Imaging Biol. 2010;12:15–24.
Shakhbazau AV, Sevyaryn IN, Goncharova NV, Grinev VV, Kosmacheva SM, Potapnev MP. Viral vectors for stable transduction of human mesenchymal stem cells: systems based on adeno-associated viruses and lentiviruses. Bull Exp Biol Med. 2008;146:531–3.
Vargas JE, Chicaybam L, Stein RT, Tanuri A, Delgado-Cañedo A, Bonamino MH. Retroviral vectors and transposons for stable gene therapy: advances, current challenges and perspectives. J Transl Med. 2016;14:288.
Abdul Halim NS, Fakiruddin KS, Ali SA, Yahaya BH. A comparative study of non-viral gene delivery techniques to human adipose-derived mesenchymal stem cell. Int J Mol Sci. 2014;15:15044–60.
Hohenstein KA, Pyle AD, Chern JY, Lock LF, Donovan PJ. Nucleofection mediates high-efficiency stable gene knockdown and transgene expression in human embryonic stem cells. Stem Cells. 2008;26:1436–43.
Liu Y, Judd K, Lakshmipathy U. Stable transfection using episomal vectors to create modified human embryonic stem cells. Methods Mol Biol. 2013;997:263–72.
Wilber A, Montoya FU, Hammer L, Moriarity BS, Geurts AM, Largaespada DA, et al. Efficient non-viral integration and stable gene expression in multipotent adult progenitor cells. Stem Cells Int. 2011;2011:717069.
Wakabayashi A, Ulirsch JC, Ludwig LS, Fiorini C, Yasuda M, Choudhuri A, et al. Insight into GATA1 transcriptional activity through interrogation of cis elements disrupted in human erythroid disorders. Proc Natl Acad Sci USA. 2016;113:4434–9.
Baek EJ, Kim HO. In-vitro production of functional RBCs from hematopoietic stem cells. In: Kim H, Greenburg A, editors. Hemoglobin-based oxygen carriers as red cell substitutes and oxygen therapeutics. Berlin: Springer; 2013. p. 359–66.
Besarab A, Coyne DW. Iron supplementation to treat anemia in patients with chronic kidney disease. Nat Rev Nephrol. 2010;6:699–710.
Dzierzak E, Philipsen S. Erythropoiesis: development and differentiation. Cold Spring Harb Perspect Med. 2013;3:a011601.
Bouhassira EE. Concise review: production of cultured red blood cells from stem cells. Stem Cells Transl Med. 2012;1:927–33.
Hattangadi SM, Wong P, Zhang L, Flygare J, Lodish HF. From stem cell to red cell: regulation of erythropoiesis at multiple levels by multiple proteins, RNAs, and chromatin modifications. Blood. 2011;118:6258–68.
Kim HO. In-vitro stem cell derived red blood cells for transfusion: are we there yet? Yonsei Med J. 2014;55:304–9.
Koury MJ, Haase VH. Anaemia in kidney disease: harnessing hypoxia responses for therapy. Nat Rev Nephrol. 2015;11:394–410.
Miharada K, Nakamura Y. In vitro production of enucleated red blood cells from hematopoietic stem and progenitor cells. Methods Mol Biol. 2012;879:505–12.
Migliaccio AR, Whitsett C, Papayannopoulou T, Sadelain M. The potential of stem cells as an in vitro source of red blood cells for transfusion. Cell Stem Cell. 2012;10:115–9.
Caminal M, Labrozzi JP, Oliver-Vila I, Alzaga-Gragera M, Marín-Gállen S, Pla A, et al. Ex vivo production of red blood cells from human cord blood. BMC Proc. 2015;9:P67.
Sankaran VG, Weiss MJ. Anemia: progress in molecular mechanisms and therapies. Nat Med. 2015;21:221–30.
Xi J, Li Y, Wang R, Wang Y, Nan X, He L, et al. In vitro large scale production of human mature red blood cells from hematopoietic stem cells by coculturing with human fetal liver stromal cells. Biomed Res Int. 2013;2013:807863.
Zhang CC, Lodish HF. Cytokines regulating hematopoietic stem cell function. Curr Opin Hematol. 2008;15:307–11.
Koury MJ. Tracking erythroid progenitor cells in times of need and times of plenty. Exp Hematol. 2016;44:653–63.
Li J, Hale J, Bhagia P, Xue F, Chen L, Jaffray J, et al. Isolation and transcriptome analyses of human erythroid progenitors: BFU-E and CFU-E. Blood. 2014;124:3636–45.
Denu RA. SIRT3 enhances mesenchymal stem cell longevity and differentiation. Oxid Med Cell Longev. 2017;2017:5841716.
Khatiwala R, Cai C. Strategies to enhance the effectiveness of adult stem cell therapy for ischemic heart diseases affecting the elderly patients. Stem Cell Rev. 2016;12:214–23.
Khorraminejad-Shirazi M, Farahmandnia M, Kardeh B, Estedlal A, Kardeh S, Monabati A. Aging and stem cell therapy: AMPK as an applicable pharmacological target for rejuvenation of aged stem cells and achieving higher efficacy in stem cell therapy. Hematol Oncol Stem Cell Ther. 2017. https://doi.org/10.1016/j.hemonc.2017.08.001.
Piccinato CA, Sertie AL, Torres N, Ferretti M, Antonioli E. High OCT4 and low p16(INK4A) expressions determine in vitro lifespan of mesenchymal stem cells. Stem Cells Int. 2015;2015:369828.
Schultz MB, Sinclair DA. When stem cells grow old: phenotypes and mechanisms of stem cell aging. Development. 2016;143:3–14.
Chute JP. Stem cell homing. Curr Opin Hematol. 2006;13:399–406.
Doan PL, Chute JP. The vascular niche: home for normal and malignant hematopoietic stem cells. Leukemia. 2012;26:54–62.
Lapidot T, Dar A, Kollet O. How do stem cells find their way home? Blood. 2005;106:1901–10.
Srour EF, Jetmore A, Wolber FM, Plett PA, Abonour R, Yoder MC, et al. Homing, cell cycle kinetics and fate of transplanted hematopoietic stem cells. Leukemia. 2001;15:1681–4.
Jayappa KD, Ao Z, Yao X. The HIV-1 passage from cytoplasm to nucleus: the process involving a complex exchange between the components of HIV-1 and cellular machinery to access nucleus and successful integration. Int J Biochem Mol Biol. 2012;3:70–85.
Mebius RE, Kraal G. Structure and function of the spleen. Nat Rev Immunol. 2005;5:606–16.
Beck Z, Brown BK, Wieczorek L, Peachman KK, Matyas GR, Polonis VR, et al. Human erythrocytes selectively bind and enrich infectious HIV-1 virions. PLoS ONE. 2009;4:e8297.
Hess C, Klimkait T, Schlapbach L, Del Zenero V, Sadallah S, Horakova E, et al. Association of a pool of HIV-1 with erythrocytes in vivo: a cohort study. Lancet. 2002;359:2230–4.
Lachgar A, Jaureguiberry G, Le Buenac H, Bizzini B, Zagury JF, Rappaport J, et al. Binding of HIV-1 to RBCs involves the Duffy antigen receptors for chemokines (DARC). Biomed Pharmacother. 1998;52:436–9.
Olinger GG, Saifuddin M, Spear GT. CD4-Negative cells bind human immunodeficiency virus type 1 and efficiently transfer virus to T cells. J Virol. 2000;74:8550–7.
Freitag J, Bates D, Boyd R, Shah K, Barnard A, Huguenin L, et al. Mesenchymal stem cell therapy in the treatment of osteoarthritis: reparative pathways, safety and efficacy - a review. BMC Musculoskelet Disord. 2016;17:230.
Leventhal A, Chen G, Negro A, Boehm M. The benefits and risks of stem cell technology. Oral Dis. 2012;18:217–22.
Mousavinejad M, Andrews PW, Shoraki EK. Current biosafety considerations in stem cell therapy. Cell J. 2016;18:281–7.
Nagpal A, Choy FC, Howell S, Hillier S, Chan F, Hamilton-Bruce MA, et al. Safety and effectiveness of stem cell therapies in early-phase clinical trials in stroke: a systematic review and meta-analysis. Stem Cell Res Ther. 2017;8:191.
Acknowledgements
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Not applicable.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Not applicable.
Funding
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Halder, U.C. Bone marrow stem cells to destroy circulating HIV: a hypothetical therapeutic strategy. J of Biol Res-Thessaloniki 25, 3 (2018). https://doi.org/10.1186/s40709-018-0075-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40709-018-0075-5