Abstract
Background
A number of risk factors have been evaluated in ocular surface squamous neoplasia, but few studies have assessed risk factors specific to the armed forces veteran population.
Methods
We conducted a retrospective case-control study on 55 patients and 55 age-matched controls with biopsy-proven ocular surface squamous neoplasia from the Miami Veterans Administration Hospital Eye Clinic to investigate potential risk factors encountered by veterans, including service-specific exposures. Veteran-specific risk factors included ionizing radiation exposure, Agent Orange exposure, deployment to Southwest Asia, and exposure to the series of biochemical warfare tests known as Project Shipboard Hazard and Defense. Data was analyzed with SPSS (SPSS Inc., Chicago, IL) using t-tests, chi-squared, and logistic regression analysis, with a p-value of < 0.05 considered statistically significant.
Results
The strongest risk factor for ocular surface squamous neoplasia was lifetime sun exposure both directly assessed via historical quantification of exposure by dermatology practitioners (Odds Ratio (OR) 5.4, 95% Confidence Interval (CI) 2.27–12.847, p < 0.005), and using the surrogate markers of basal cell carcinoma (OR 3.157, 95% CI 1.286–7.748, p = 0.010) and pingueculae (OR 5.267, 95% CI 2.104–13.186, p < 0.005). Of the veteran-specific risk factors, Agent Orange exposure and Southwest Asia deployment were not associated with an increased risk of ocular surface squamous neoplasia. Exposure to ionizing radiation and involvement in Project Shipboard Hazard and Defense were not documented among any cases or controls.
Conclusions
The results of our study are consistent with prior established risk factors, namely highlighting the important role of sun exposure in ocular surface squamous neoplasia among veterans.
Similar content being viewed by others
Background
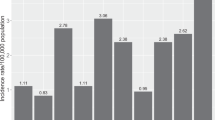
Ocular surface squamous neoplasia (OSSN) represents a range of pathologies of the ocular surface ranging from squamous epithelial dysplasia to invasive squamous cell carcinoma (SCC) arising from the conjunctiva, cornea or both [1]. While large-scale epidemiological studies are lacking as a whole, a study carried out by the United States National Cancer Institute estimated an annual incidence of 0.03/100,000 for SCC arising from the conjunctiva of Caucasian patients [2].
To increase understanding of this relatively uncommon disease, risk factors for the development of OSSN have been researched. Excess ultraviolet (UV) radiation and its sequelae in the eye (pingueculae, pterygia, etc.) remains one of the most thoroughly associated exposures [3]. Other factors associated with OSSN include human immunodeficiency virus (HIV) [4], human papillomavirus (HPV) [5, 6], allergic conjunctivitis [7], and genetic mutations involving impaired DNA repair, such as xeroderma pigmentosum and defects in the tumor suppressor gene TP53 which plays an important role in regulation of the cell cycle [8]. The association between smoking and OSSN has also been researched with mixed results [9, 10].
Two distinct clinical presentations of OSSN have been described in the literature. In developed countries such as the United States and Australia, OSSN tends to be more prevalent amongst elderly white men in their sixties [11]. In contrast, cases of OSSN in developing nations like sub-Saharan Africa tend to be diagnosed in young black patients (male and female) in their mid-to-late 30’s [12, 13]. Patients diagnosed in developing countries also tend to present with much more aggressive disease, which has been hypothesized to be due to the higher prevalence of HIV and HPV [14, 15].
As OSSN typically presents amongst elderly white males in developed countries, a particular population of interest is the aging veteran population. Members of the armed forces are exposed to unique factors during their terms of deployment, and limited research has been done to examine the impact of these exposures on the development of OSSN. A study by McClellan et al. performed in 2015 investigated risk factors for 28 cases of OSSN who presented for evaluation to the Veterans Administration Hospital of Miami from 2007 to 2012, showing that factors associated with UV light exposure predominated [16]. However, this study did not research the impact of veteran-specific risk factors, such as exposure to ionizing radiation, Agent Orange, deployment to Southwest Asia, and involvement in a series of biochemical warfare tests conducted from 1962 to 1973 known as Project Shipboard Hazard and Defense [17], on OSSN. With this in mind, our study aimed to assess the impact of veteran-specific risk factors on the development of OSSN.
Methods
Patient population
The study population included 55 cases of biopsy-proven OSSN who were treated at the Miami Veterans Administration Hospital Eye Clinic between 2010 and 2018. Fifty-five age- (within 5 years), gender- and race-matched controls without OSSN were selected from individuals seen in the Miami Veterans Administration Hospital Eye Clinic on the same dates as the cases.
Data collection
The Miami Veterans Administration Institutional Review Board approved this retrospective case-control study. The methods adhered to the tenets of the Declaration of Helsinki and were Health Insurance Portability and Accountability Act (HIPAA)-compliant. Data were acquired from the Veterans Administration Hospital electronic medical record system. Demographic information included age, gender and race. Past medical history included diagnoses of type 2 diabetes mellitus, head and neck cancer and xeroderma pigmentosum. General risk factors investigated included tobacco exposure (current or previous vs. none), infection with HPV or infection with HIV. Ultraviolet-related exposures included history of significant lifetime sun exposure (coded as yes or no based on dermatology note documentation); history of outdoor occupation outside of military service (coded as yes or no; primary care notes documented occupations, those we considered outdoor were construction workers, fishermen, boat workers, gardeners and farmers); skin pathologies (actinic keratosis, basal cell carcinoma (BCC), SCC, melanoma); and diagnoses of pingueculae or pterygia. Veteran-specific risk factors were also extracted, including exposure to ionizing radiation, Agent Orange, Southwest Asia deployment [18]; and involvement in Project Shipboard Hazard and Defense (all coded as yes or no based on documentations in the medical record).
Statistical analysis
Descriptive statistics were used to summarize our patient population. Statistical analyses were performed using Microsoft Excel Version 16.12 and SPSS Version 25 (SPSS Inc., Chicago, IL). Analysis was performed on 55 biopsy-proven cases of OSSN and their corresponding controls. Continuous variables were compared between cases and controls using an independent t-test and categorical variables were compared using Chi squared or Fisher exact tests, as appropriate. Logistic regression analysis was used to evaluate the effect of risk factors on OSSN, as represented by an odds ratio (OR). A 95% confidence interval (CI) was determined with a p-value < 0.05 being considered statistically significant.
Results
Demographics
The mean age of the cases on chart review was 73.2 ± 8.7 years with OSSN being diagnosed at a mean age of 69.1 ± 9.2 years. The mean age of the control population was 72.9 ± 8.0 years. Nearly all patients were male (98%) and Caucasian (85.5%). No statistically significant association with OSSN was found in relation to age, gender or race (Table 1).
Medical conditions
Among the medical factors examined, no significant association with OSSN was found for type 2 diabetes mellitus, head/neck cancer or xeroderma pigmentosum (Table 1).
General risk factors
No significant association with OSSN was found for general risk factors including history of current or former tobacco exposure, infection with HPV or infection with HIV.
UV-related risk factors
Among UV-related risk factors, a history of significant sun exposure (as documented by dermatology) (OR 5.40, 95% CI 2.27–12.85, p = < 0.005), history of outdoor occupation as a boat worker (OR 1.08, 95% CI 1.01–1.16, p = 0.04) as well as diagnoses of BCC (OR 3.16, 95% CI 1.29–7.75, p = 0.01) and pingueculae (OR 5.27, 95% CI 2.10–13.19, p = < 0.005) were all significantly associated with OSSN. History of any of the outdoor occupations investigated (OR 1.92, 95% CI 0.76–4.86, p = 0.17) as well as diagnoses of actinic keratosis (OR 1.24, 95% CI 0.59–2.63, p = 0.57), melanoma (OR 4.24, 95% CI 0.46–39.2, p = 0.17) and pterygia (OR 2.29, 95% CI 0.92–5.71, p = 0.07) also exhibited elevated risk of OSSN but did not reach statistical significance (Table 1).
Veteran-specific risk factors
Among the veteran-specific risk factors studied, none significantly affected the risk of OSSN. Agent Orange exposure (OR 1.37, p = 0.5) had an OR greater than 1 but was not statistically significant. Exposure to ionizing radiation and involvement in Project Shipboard Hazard and Defense were not documented among any cases or controls, and Southwest Asia condition was only documented in a handful of controls and no cases (Table 1).
Discussion
While the study by McClellan et al. investigated well-researched risk factors for OSSN in the veteran population of South Florida [16], our study sought to continue this work by investigating the effect of veteran-specific factors on OSSN. Of these veteran-specific risk factors, no statistically significant associations with OSSN were found. On the other hand, our results confirm that factors associated with increased UV exposure (history of significant lifetime sun exposure, occupation as a boat worker, BCC and pinguecula) were significantly associated with an increased risk of OSSN. Other factors associated with increased UV exposure (history of any outdoor occupation, actinic keratosis, melanoma, pterygia) also exhibited increased risk of OSSN but did not reach statistical significance. Similar to the study by McClellan, we showed a paradoxically decreased risk of developing OSSN with a history of type 2 diabetes mellitus but our association did not reveal any statistical significance.
UV exposure has a strong association with the development of OSSN and our findings supported this [3]. Longer wavelengths of UV radiation (particularly UV-B) are absorbed by DNA strands leading to the production of cyclobutene pyrimidine dimers via the formation of carbon-carbon double bonds in the nucleotide’s associated nitrogenous bases [19]. These pyrimidine dimers have been shown to inhibit the function of DNA polymerases, and failure of cells to repair UV-induced damage to DNA can lead to misreading of the genetic code, leading to mutations and neoplasia [20]. Other DNA-damaging reactions that occur as a result of UV exposure include hydrolytic deamination of bases (which in turn alter the genetic code at that segment) and the generation of reactive oxygen species [21]. The skin and eyes are both superficial structures and have the greatest exposure to UV, leading a spectrum of benign (thinning of the skin, cataracts) and neoplastic (SCC, melanoma) conditions [22, 23].
Many veterans are exposed to UV radiation. Unique exposures for veterans include service in regions and armed forces branches with increased sun exposure, such as aboard waterboard vessels. A survey of active service men and women showed that less than 30% of soldiers had regular access to sunscreen and that as a result their skin was unprotected 70% or more of the time [24]. Large scale systematic reviews have shown that US military personnel have higher rates of skin cancer than civilians along with lower rates of skin cancer awareness and dermatologic care [25]. In addition to service, occupational exposure while not deployed represents another route for UV irradiation. In our population, 22% of individuals had a career that required outdoor sun exposure with those serving as boat workers having a significantly higher risk of developing OSSN.
We additionally focused on other veteran-specific risk factors because there is biological plausibility that some of these may increase the risk of eye malignancy. Exposure to ionizing radiation has long been shown to be carcinogenic. After the discovery of X-rays in the late nineteenth century, the development of SCC in exposed skin was recognized by early radiologists [26]. Some members of the armed forces, such as nuclear weapon technicians, have increased exposure to ionizing radiation, increasing their risk for malignancy. A case study by Nelson et al. details a veteran patient exposed to radioactive debris during salvage of material from a failed atmospheric weapon launch who subsequently went on to develop over 300 BCC’s and 2 SCC’s over a 30-year period, hypothesized to be due to ionizing radiation exposure from the atomic weapon [27]. In addition to skin cancers, a large scale study performed in Australia showed that exposure to low-dose ionizing radiation via computed tomography in childhood led to an increased incidence of a variety of cancers later in life including brain, thyroid, urinary tract, genital organs, and hematologic malignancies [28]. However, none of the individuals in our cohort had documentation of exposure to ionizing radiation.
Agent Orange’s role as a risk factor for malignancy has also been researched extensively. A contaminant in the production of Agent Orange, 2,3,7,8-tetrachlorodibenzo-p dioxin (TCDD), is a known human carcinogen [29]. The proposed mechanism of TCDD involves stimulation of the aryl hydrocarbon receptor (AhR), which upregulates cellular signaling, DNA binding and transcriptional activation leading to tumor-promoting activities [30]. Evidence for this mechanism has been strengthened by studies showing that AhR-deficient mice show resistance to TCDD-induced toxicity [31]. Beginning in 1994, the Institute of Medicine has issued periodic reports on Agent Oranges effects on both cancerous and non-cancerous health conditions. As of the latest report, exposure to Agent Orange has shown sufficient evidence of association to the development of soft tissue sarcomas, Non-Hodgkin’s and Hodgkin’s lymphoma and chronic lymphocytic lymphoma in the veteran population [32]. While some studies suggested that TCDD could affect squamous cells as well [33, 34], exposure to Agent Orange was not found to be a significant risk factor for OSSN in our study.
Involvement in Project Shipboard Hazard and Defense represents another avenue that veterans could be exposed to possibly carcinogenic chemicals. In the 1960’s, the U.S. Department of Defense conducted a series of tests to investigate vulnerabilities of U.S. Navy ships to chemical and biological agents, such as the nerve gases sarin and venomous agent X (commonly referred to as “VX”). It was believed that approximately 5900 veterans were involved in the testing. Long-term follow up studies on mortality in veterans involved in Project Shipboard Hazard and Defense showed no increased mortality associated with malignancies but did demonstrate an increased overall mortality due to heart disease [35]. Since none of our patients took part in Project Shipboard Hazard and Defense, we were unable to evaluate if there is any association with OSSN.
A number of limitations were present within our study that must be considered when interpreting the study results. Our data is limited to that available within the VA electronic medical records. OSSN has a relatively low incidence and our study population was limited to fifty five cases of OSSN over eight years of review. Exposure to veteran-specific risk factors of interest, such as ionizing radiation and Project Shipboard Hazard and Defense, was not found during chart review, limiting our ability to assess their role in OSSN. Future studies specifically including patients exposed to ionizing radiation and Project Shipboard Hazard and Defense can better delineate if these exposures are significant risk factors for OSSN development. Collaboration between multiple institutions could also increase the size of the study population and power of future studies. We also did not assess the effect of newly appreciated veteran exposures such as uranium or petroleum as these information were not readily available within the medical records.
Conclusions
Despite the limitations discussed, our study corroborates the impact UV light has on OSSN. Further research into risk factors in specific populations will help identify new risk factors and allow for evidence-guided screening protocols in appropriate populations.
Abbreviations
- BCC:
-
Basal cell carcinoma
- CI:
-
Confidence interval
- HIV:
-
Human immunodeficiency virus
- HPV:
-
Human papilloma virus
- OR:
-
Odds ratio
- OSSN:
-
Ocular surface squamous neoplasia
- SCC:
-
Squamous cell carcinoma
- TCDD:
-
tetrachlorodibenzo-p dioxin
- UV:
-
Ultraviolet
References
Basti S, Macsai MS. Ocular surface squamous neoplasia: a review. Cornea. 2003;22(7):687–704.
Emmanuel B, Ruder E, Lin SW, Abnet C, Hollenbeck A, Mbulaiteye S. Incidence of squamous-cell carcinoma of the conjunctiva and other eye cancers in the NIH-AARP Diet and Health Study. Ecancermedicalscience. 2012;6:254.
Lee GA, Williams G, Hirst LW, Green AC. Risk factors in the development of ocular surface epithelial dysplasia. Ophthalmology. 1994;101(2):360–4.
Rathi SG, Ganguly Kapoor A, Kaliki S. Ocular surface squamous neoplasia in HIV-infected patients: current perspectives. HIV AIDS (Auckl). 2018;10:33–45.
Egawa N, Egawa K, Griffin H, Doorbar J. Human papillomaviruses; epithelial tropisms, and the development of neoplasia. Viruses. 2015;7(7):3863–90.
Galor A, Garg N, Nanji A, Joag M, Nuovo G, Palioura S, et al. Human papilloma virus infection does not predict response to interferon therapy in ocular surface squamous neoplasia. Ophthalmology. 2015;122(11):2210–5.
Gichuhi S, Macharia E, Kabiru J, Zindamoyen AM, Rono H, Ollando E, et al. Risk factors for ocular surface squamous neoplasia in Kenya: a case-control study. Tropical Med Int Health. 2016;21(12):1522–30.
Ateenyi-Agaba C, Dai M, Le Calvez F, Katongole-Mbidde E, Smet A, Tommasino M, et al. TP53 mutations in squamous-cell carcinomas of the conjunctiva: evidence for UV-induced mutagenesis. Mutagenesis. 2004;19(5):399–401.
Gichuhi S, Sagoo MS, Weiss HA, Burton MJ. Epidemiology of ocular surface squamous neoplasia in Africa. Tropical Med Int Health. 2013;18(12):1424–43.
Napora C, Cohen EJ, Genvert GI, Presson AC, Arentsen JJ, Eagle RC, et al. Factors associated with conjunctival intraepithelial neoplasia: a case control study. Ophthalmic Surg. 1990;21(1):27–30.
Sun EC, Fears TR, Goedert JJ. Epidemiology of squamous cell conjunctival cancer. Cancer Epidemiol Biomarkers Prev. 1997;6(2):73–7.
Newton R, Ziegler J, Ateenyi-Agaba C, Bousarghin L, Casabonne D, Beral V, et al. The epidemiology of conjunctival squamous cell carcinoma in Uganda. Br J Cancer. 2002;87(3):301–8.
Kaimbo Wa Kaimbo D, Parys-Van Ginderdeuren R, Missotten L. Conjunctival squamous cell carcinoma and intraepithelial neoplasia in AIDS patients in Congo Kinshasa. Bull Soc Belge Ophtalmol. 1998;268:135–41.
Kamal S, Kaliki S, Mishra DK, Batra J, Naik MN. Ocular surface squamous neoplasia in 200 patients: a case-control study of immunosuppression resulting from human immunodeficiency virus versus immunocompetency. Ophthalmology. 2015;122(8):1688–94.
Ateenyi-Agaba C. Conjunctival squamous-cell carcinoma associated with HIV infection in Kampala, Uganda. Lancet. 1995;345(8951):695–6.
McClellan AJ, McClellan AL, Pezon CF, Karp CL, Feuer W, Galor A. Epidemiology of ocular surface squamous neoplasia in a veterans affairs population. Cornea. 2013;32(10):1354–8.
Assessing health outcomes among veterans of project SHAD (Shipboard Hazard and Defense). Mil Med. 2018;183(5–6):96–7.
Gulf War Service. https://www.publichealth.va.gov/exposures/gulfwar/military-service.asp. Accessed 13 June 2018.
Yoon JH, Lee CS, O'Connor TR, Yasui A, Pfeifer GP. The DNA damage spectrum produced by simulated sunlight. J Mol Biol. 2000;299(3):681–93.
Sinha RP, Hader DP. UV-induced DNA damage and repair: a review. Photochem Photobiol Sci. 2002;1(4):225–36.
Lindahl T. Instability and decay of the primary structure of DNA. Nature. 1993;362(6422):709–15.
Ichihashi M, Ueda M, Budiyanto A, Bito T, Oka M, Fukunaga M, et al. UV-induced skin damage. Toxicology. 2003;189(1–2):21–39.
van Kuijk FJ. Effects of ultraviolet light on the eye: role of protective glasses. Environ Health Perspect. 1991;96:177–84.
Powers JG, Patel NA, Powers EM, Mayer JE, Stricklin GP, Geller AC. Skin cancer risk factors and preventative behaviors among United States military veterans deployed to Iraq and Afghanistan. J Invest Dermatol. 2015;135(11):2871–3.
Riemenschneider K, Liu J, Powers JG. Skin cancer in the military: a systematic review of melanoma and nonmelanoma skin cancer incidence, prevention, and screening among active duty and veteran personnel. J Am Acad Dermatol. 2018;78(6):1185–92.
Yoshinaga S, Hauptmann M, Sigurdson AJ, Doody MM, Freedman DM, Alexander BH, et al. Nonmelanoma skin cancer in relation to ionizing radiation exposure among U.S. radiologic technologists. Int J Cancer. 2005;115(5):828–34.
Nelson KL, Randle HW. Skin cancer in an atomic veteran: cause or coincidence? Dermatol Surg. 2003;29(11):1100–4.
Mathews JD, Forsythe AV, Brady Z, Butler MW, Goergen SK, Byrnes GB, et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ. 2013;346:f2360.
Frumkin H. Agent orange and cancer: an overview for clinicians. CA Cancer J Clin. 2003;53(4):245–55.
IARC working group on the evaluation of carcinogenic risks to humans: Polychlorinated dibenzo-Para-dioxins and polychlorinated dibenzofurans. Lyon, France, 4-11 February 1997. IARC Monogr Eval Carcinog Risks Hum. 1997;69:1–631.
Fernandez-Salguero PM, Hilbert DM, Rudikoff S, Ward JM, Gonzalez FJ. Aryl-hydrocarbon receptor-deficient mice are resistant to 2,3,7,8-tetrachlorodibenzo-p-dioxin-induced toxicity. Toxicol Appl Pharmacol. 1996;140(1):173–9.
Council NR. Veterans and agent orange: update 2000. Washington (DC): National Academies Press (US); 2001.
Sorg O. Association between agent orange exposure and nonmelanotic invasive skin cancer: a pilot study. Plast Reconstr Surg. 2015;135(1):233e–4e.
Hébert CD, Cao QL, Birnbaum LS. Inhibition of high-density growth arrest in human squamous carcinoma cells by 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD). Carcinogenesis. 1990;11(8):1335–42.
Kang HK, Bullman T. Mortality follow-up of veterans who participated in military chemical and biological warfare agent testing between 1962 and 1972. J Toxicol Environ Health A. 2009;72(23):1550–2.
Acknowledgements
Not applicable.
Funding
Supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Clinical Sciences Research EPID-006-15S (Dr. Galor), R01EY026174 (Dr. Galor), NIH Center Core Grant P30EY014801 and Research to Prevent Blindness Unrestricted Grant, The Ronald and Alicia Lepke Grant, The Lee and Claire Hager Grant, The Jimmy and Gaye Bryan Grant, The H. Scott Huizenga Grant, The Grant and Diana Stanton-Thornbrough,The Robert Baer Family Grant, The Emilyn Page and Mark Feldberg Grant, and the Richard Azar Family Grant (institutional grants).
Availability of data and materials
The datasets generated during and/or analyzed in the current study are not publicly available due to confidentiality of information extracted from the Computerized Personal Records System of the Veterans Administration Hospital system.
Author information
Authors and Affiliations
Contributions
LS analyzed and interpreted the de-identified patient data while serving as the primary writer of the manuscript. SL assisted in writing the Introduction of the final manuscript. CK provided valuable feedback in the final revisions of the manuscript. AG oversaw the IRB approval process, assisted in compiling the set of cases and controls and provided extensive feedback in the writing of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The methods adhered to the tenets of the Declaration of Helsinki and were Health Insurance Portability and Accountability Act (HIPAA)-compliant. The Miami Veterans Administration Institutional Review Board approved this retrospective case-control study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Smith, L.M., Lamba, S., Karp, C.L. et al. Epidemiology of ocular surface squamous neoplasia in veterans: a retrospective case-control study. Eye and Vis 6, 14 (2019). https://doi.org/10.1186/s40662-019-0138-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40662-019-0138-1