Abstract
Background
Hypoxic-ischemic encephalopathy (HIE) is a common disease that occurs during the perinatal period. The primary cause of neonatal HIE is related to fetal intrauterine anoxia. Carbamylated erythropoietin (CEPO), a derivative of erythropoietin (EPO), does not exert any erythropoietic effect; however, the neuroprotective effects resemble those of EPO. Previous studies have shown the potential benefits of CEPO on the central nervous system. The present study aimed to investigate the role of CEPO in neuronal apoptosis during intrauterine HIE and the underlying mechanisms.
Results
To validate our hypothesis, we established an intrauterine HIE model by occluding the bilateral utero-ovarian arteries of pregnant Sprague–Dawley rats. Compared to the I/R group, neuronal apoptosis in the CEPO group was significantly lower at 4, 12, 24, and 48 h (P < 0.05). CEPO significantly inhibited CC3 expression (P < 0.05) during the early-stages after ischemia–reperfusion (0.5, 4, 8, 12 and 24 h), upregulated Bcl-2 expression, and downregulated Bax expression at 4, 8, 12, and 24 h (P < 0.05).
Conclusions
Carbamylated erythropoietin pretreatment inhibited the expression of proapoptotic protein CC3 in brain and regulated the Bcl-2/Bax ratio, resulting in reduced neuronal apoptosis and thus resulting in a protective effect on intrauterine HIE.
Similar content being viewed by others
Background
Hypoxic-ischemic encephalopathy (HIE) is one of the major causes of death and disability in children, and is primarily induced by fetal distress and intrapartum asphyxia [1]. HIE not only affects the child’s intellectual level but may also lead to severe neurological dysfunction, as well as perinatal death [2]. Of the 2.8 million neonatal deaths in 2013, 0.64 million deaths (22.9%) were estimated to be caused by intrapartum asphyxia [3]. In recent years, obstetric and neonatal medicine has made progress to improve HIE prognosis; however, effective prophylaxis and treatments are yet lacking.
Erythropoietin (EPO) is the main cytokine involved in erythropoiesis in vivo, and inhibits apoptosis of erythroid progenitors in the bone marrow [4]. Recombinant human erythropoietin (rhEPO), synthesized using recombinant DNA technology, has been widely used in the clinical treatment of anemia caused by various diseases such as cancer [5], premature labor [6], and chronic kidney disease [7]. Recently, studies have shown that EPO exerts a hematopoietic as well as a protective effect on tissues, especially in the central nervous system (CNS).
Erythropoietin and erythropoietin receptor (EPOR) expression in the CNS is significantly increased after ischemia, hypoxia, and other stress conditions, suggesting that EPO might be an endogenous neuroprotective protein [8]. However, endogenous EPO production is limited, indicating that it might be effectively supplied to protect the brain against HIE. In previous studies, we demonstrated that EPO could antagonize intrauterine HIE through the placenta and blood–brain barrier (BBB) [9, 10]. However, high-doses or long-term exposure to EPO may cause an over-stimulation in the bone marrow hematopoietic system leading to polycythemia, hypertension, and thrombosis [11]. This phenomenon is observed especially during pregnancy in the hypercoagulable state in patients, wherein EPO increases the perinatal risk of thrombosis [12], limiting the obstetric applications.
Carbamylated erythropoietin (CEPO), a homolog of EPO, does not exert any erythropoietic effects but is similar to EPO with respect to stability, BBB permeability, and pharmacokinetics [13]. The neuroprotective effects of CEPO resemble that of EPO in cerebral infarction [14], traumatic brain injury [15], experimental autoimmune encephalomyelitis [16], diabetic neuropathy [17], and other models without hematopoietic activity [13]. However, whether administration of CEPO on pregnant mothers exerts a protective effect against fetal neurological damage in the intrauterine hypoxic-ischemic state has not been reported. Hence, in this study, we established an intrauterine HI model using fetal rats to investigate the neuroprotective effects of CEPO on neuronal apoptosis and the underlying mechanisms.
Results
Identification of rhEPO carbamylation reaction
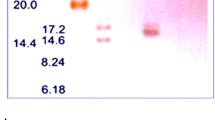
Endoproteinase carboxyl side of lysine (Lys-C) breaks the peptide chains of lysine [18]. The molecular weight of rhEPO is about 34 kDa and, the cleaved chains are approximately 16 kDa. Lysine residues, converted to homocitrulline by carbamylation, cannot be cleaved by endoproteinase Lys-C. Therefore, the CEPO protein chain will remain about 34 kDa. As shown in Fig. 1, the 2nd and 4th lanes are rhEPO and CEPO with a molecular mass of 34 kDa; the 3rd and 5th lanes are reaction products with endoproteinase Lys-C. In the 3rd lane, rhEPO reacted with the endoproteinase Lys-C and the chains were cleaved with a molecular mass of 16 kDa; in the 5th lane, CEPO was not cleaved by endoproteinase Lys-C, and hence, only 34 kDa but not 16 kDa peptides were observed, indicating that EPO was completely converted to CEPO according to our synthesis protocol.
CEPO identification using SDS-PAGE electrophoresis. Lane 1: markers; Lane 2: rhEPO, a broad band of 34 kDa (black arrow); Lane 3: rhEPO + endoproteinase Lys-C, 31 kDa (asterisk) and 16 kDa (filled triangle); Lane 4: CEPO, band around 34 kDa (white arrow); Lane 5: CEPO + endoproteinase Lys-C, a broad band around 34 kDa (white triangle) and a thinner band near 31KDA (asterisk). The 31 kDa band present in all lanes may be due to the Lys-C protein
Birth state and death rate of fetal rats for each group
In the sham group, pups had ruddy skin and satisfactory limb movements but no fetal death. In the hypoxic-ischemic reperfusion (I/R) group, body appearances did not show obvious abnormalities at 0.5 h. However, at 4 h, the fetuses appeared violaceous, reflexes were weak and some fetal death occurred. The mortality was increased at 24 h. CEPO pretreatment improved the fetal situation but did not alter neonatal mortality. Compared to the I/R group, a significant difference was observed only at 48 h (Table 1, P = 0.045).
CEPO alleviated brain morphology changes
Hematoxylin–eosin (HE) staining demonstrated that intrauterine ischemia–hypoxia (HI) induced pathological changes in the brain cells. In the sham group, the morphology of the brain was normal and neural degeneration was rarely observed. I/R group showed edema in glial cells, disorders in the pyramidal cell arrangement, reduced cell volume, irregular nuclear chromatin, karyopyknosis, and eosinophilic cytoplasm (Fig. 2). Qualitative analyses demonstrated that CEPO preconditioning reduced these pathological changes.
CEPO administration inhibited apoptosis
Terminal deoxynucleotidyl transferase-mediated dUTP nick end-labeling (TUNEL) staining was used to analyze the apoptotic index. The sham group showed 2.67 ± 0.57% positive cells in brain. The apoptotic index of the I/R and CEPO groups at different time points is shown in Fig. 3. Apoptosis increased gradually and reached a peak at 24 h post-reperfusion. Compared to the I/R group, apoptotic indexes for the CEPO group was significantly lower (one-way ANOVA, P < 0.05) at 4, 12, 24, and 48 h. This demonstrated that CEPO inhibited the intrauterine HI-induced neuronal apoptosis effectively.
Apoptosis levels of brain cells after reperfusion. a Immunoreactive cells after TUNEL staining (400×); b statistics of apoptotic indexes (%). The quantitative results are obtained using Image Pro Plus 6.0 image analysis software. Data are presented as mean ± SD of N = 4; *P < 0.05 compared to I/R group, student’s t-test; #P < 0.05 compared to sham group, ANOVA
CEPO inhibits CC3 expression after reperfusion
The cleaved caspase-3 (CC3) expression increased gradually in the I/R group and peaked levels at 8 h (one-way ANOVA, P < 0.05 vs. sham), followed by a gradual decline (Fig. 4). The CC3 levels in the CEPO + I/R group were significantly lower compared to the I/R group at 0.5, 4, 8, 12 h and 24 h (one-way ANOVA, P < 0.05), which was inconsistent with the levels of apoptosis.
CC3 expression of brain cells after reperfusion. a CC3 expression by Western blotting at different time points; b relative expression of CC3. The quantitative results are obtained using Image J software. Data are presented as mean ± SD of N = 4; *P < 0.05 compared to I/R group, student’s t-test; #P < 0.05 compared to sham group, ANOVA
CEPO pretreatment upregulated Bcl-2 expression and downregulated Bax expression
Immunohistochemistry (IHC) was used to determine the expression levels of B-cell lymphoma 2 (Bcl-2) and Bcl-2 Associated X Protein (Bax) expression levels in the brain cells at different time points after reperfusion. The changes in Bcl-2 and Bax expression are shown in Figs. 5 and 6. Compared to the I/R group, a significant upregulation in Bcl-2 expression was observed in the CEPO + I/R group (P < 0.05) except at 0.5 and 48 h. In addition, Bax expression decreased significantly in the CEPO + I/R group except at 0.5 and 48 h. Furthermore, quantitative analyses demonstrated that CEPO pre-treatment enhanced the I/R-induced Bcl-2 upregulation and suppressed the I/R-induced Bax upregulation. The ratio of relative densities was calculated using Bcl-2/Bax, which indicated anti-apoptotic activity. This ratio was significantly higher in the CEPO + I/R group compared to the I/R group during 4–24 h after reperfusion (Fig. 7, one-way ANOVA, P < 0.05).
CEPO upregulated Bcl-2 expression of brain cells. a Bcl-2 immunoreactive cells at 0.5–48 h time points (400×); b quantitative analysis of Bcl-2 protein expression. The quantitative results are obtained using Image Pro Plus 6.0 image analysis software. Data are presented as mean ± SD of N = 4; *P < 0.05 compared to I/R group, student’s t-test; #P < 0.05 compared to sham group, ANOVA
CEPO downregulated Bax expression of brain cells. a Bax immunoreactive cells at 0.5–48 h time points (400×); b quantitative analysis of Bax protein expression. The quantitative results are obtained using Image Pro Plus 6.0 image analysis software. Data are presented as mean ± SD of N = 4; *P < 0.05 compared to I/R group, student’s t-test; #P < 0.05 compared to sham group, ANOVA
Discussion
The results of the present study demonstrated that a single dose of CEPO administered intraperitoneally in pregnant rats before intrauterine HI insult decreased apoptosis and apoptosis-related proteins in fetal rats. Notably, CEPO pre-treatment could protect fetal rats from intrauterine hypoxic-ischemic brain injury through its anti-apoptotic effect. However, the underlying molecular mechanism needs further investigation.
Previous studies have demonstrated that CEPO, a derivative of EPO, does not stimulate the bone marrow hematopoietic system but has a similar neuroprotective effect as EPO on tissues. This effect has been demonstrated in various diseases such as cerebral infarction [13, 19], spinal cord injury [13], experimental autoimmune encephalomyelitis [16] and chemotherapy-induced toxicities on peripheral nerves [20]. In addition, CEPO promoted neuronal differentiation in neural stem cells [21]. Collectively these studies demonstrated that CEPO is a novel neuroprotective agent with promising clinical applications.
Only few studies have demonstrated that CEPO exerts protective effect against intrauterine HIE. In the current study, healthy pregnant rats were used to establish the intrauterine HIE model. Transient occlusion of bilateral utero-ovarian vessels can cause ischemia–reperfusion, lead to inadequacy of placental blood flow and mimic the sudden interruption block of fetal–placental circulation. Then, we compared the death rates and pathological changes in the hippocampus of fetal rats. CEPO pretreatment significantly reduced the pathological changes and mortality at 48 h compared to the I/R group. TUNEL assays demonstrated that CEPO protected the fetal rat brain from apoptosis by reducing the apoptotic rates. These results were consistent with our previous findings on EPO [9].
Neuronal death after hypoxia–ischemia injury is associated with cell death and apoptosis. In immature hypoxic-ischemic brains, apoptosis plays a crucial role. Different brain regions showed different sensitivities to hypoxic-ischemic stresses. Cerebral cortex and hippocampus were the two most sensitive areas to hypoxia–ischemia injury [22]. In the current study, TUNEL-positive cells were rarely visible in the hippocampus of the sham group. The number of apoptotic neurons in the I/R or CEPO treatment group increased with reperfusion time and reached a peak at 24 h, demonstrating that intrauterine HIE could cause typical neuronal apoptosis in the hippocampus of the fetal rat. Compared to the I/R group, CEPO pretreatment significantly reduced apoptosis in brain cells measured at similar time points. These results suggested that intrauterine HIE was directly associated with apoptosis, and CEPO played a neuroprotective role by regulating apoptosis.
Apoptosis is a complex process, mediated by the caspase family members including the protease cascades. This family encompasses different death-signal transduction proteins, which in turn, induces apoptosis [23]. Among these, caspase-3 is the core member. CC3 is an active form of caspase-3, which is highly expressed during neuronal apoptosis [24]. It is also a critical molecule that mediates cell necroptosis. Furthermore, detecting CC3 expression is a common approach to study apoptosis during brain damage [25, 26]. In the current study, increased CC3 expression was observed with time and reached peak levels at 8 h after reperfusion in the clamping and reperfusion group, followed by a gradual decrease. However, CC3 expression was not consistent with the apoptosis index, which peaked at 24 h. We speculated that the different detection methods resulted in inconsistent data. CC3 expression levels were detected by Western blot on brain tissues preserved in liquid nitrogen, while apoptosis was assessed using TUNEL staining on paraffin-embedded sections. A previous study [25] also reported that inconsistent data was observed when measuring apoptosis and CC3 expression. Nevertheless, the present study showed that CEPO significantly downregulated the CC3 expression at similar time points compared to the I/R group. The effect of CEPO on CC3 was similar to the findings of previous studies using different animal models [27, 28]. These findings suggest that CEPO might sufficiently provide early beneficial effects for intrauterine HIE.
Cell apoptosis is regulated by both pro- and anti-apoptotic proteins. In addition to CC3 expression, the Bcl-2 family is a major regulator of apoptosis. Two proteins in this family (Bcl-2 and Bax) are crucial for the regulation of apoptosis [29, 30]. Bcl-2 is an anti-apoptotic protein that blocks the release of cytochrome C from the mitochondria to the cytoplasm [31]. Bax is a pro-apoptotic member of the Bcl-2 family. Under apoptotic stimulus, Bax translocates from the cytoplasm to the mitochondrial outer membrane, inducing cytochrome C release and caspase-9 activation (by self-cleavage), which results in caspase-3 activation and ultimately apoptosis [32]. Bcl-2 and Bax antagonize each other to determine the cell fate [30]. When the ratio of Bcl-2/Bax is reduced, apoptosis is induced and vice versa when increased [33]. Our results demonstrated that Bcl-2 and Bax levels were increased in fetal rats after intrauterine ischemia and hypoxia, indicating that the expression of protective proteins was initiated along with apoptosis. However, Bcl-2/Bax ratio gradually declined over time, which indicated that cells were still in the apoptotic stage. Compared to the I/R group, Bcl-2 expression in the CEPO group was significantly increased; with a simultaneous increase in Bcl-2/Bax ratios. Taken together, these findings suggested that CEPO regulated neuronal apoptosis by increasing Bcl-2 expression and inhibiting Bax expression. The current results are in agreement with previously published studies [28].
The present study has some limitations. First, we administered a single dose of 50 μg/kg CEPO before intrauterine HI insult. Although not appropriate for potential clinical use, this time point was selected to investigate the protective effects of CEPO in the developing rat brain with HI, as described previously for EPO [9, 10]. In animals with brain injury, CEPO has been shown to be effective within a therapeutic window of at least 6 h [34, 35], and a triple dose of CEPO further reduced lesion volume and improved neurological functional recovery compared to a single dose of CEPO [34]. Whether repeated doses of CEPO or a delayed timing of treatment are equally effective in the developing rat brain with HI is yet to be deciphered. Second, the cellular mechanisms of HI injury demonstrated sexual dimorphism and the male gender was vulnerable to neonatal HIE during the perinatal period [36, 37]. Due to the lack of recognition of sexual dimorphism, we did not verify the pup’s gender during the study. Although the gender of the animals used in the previous study exploring cellular mechanisms of HI [38] was not mentioned, all litters should be gender-typed in the follow-up studies. Third, although the current experimental design had several time points, the association between brain injury and reperfusion time was not explored further. In addition, due to the intraperitoneal maternal body approach, the permeability of CEPO through placenta barrier was not measured in our study. Thus, whether permeability of CEPO was similar to that of EPO is yet to be determined.
Conclusions
Carbamylated erythropoietin pretreatment inhibited neuronal apoptosis in the hippocampus after intrauterine HI by inhibiting the expression of pro-apoptotic protein CC3 and upregulating the ratio of Bcl-2/Bax, thus inducing a neuroprotective effect. However, the signaling pathways involved in this CEPO neuroprotective effect were not explored in our animal models. To understand the detailed molecular mechanisms, further investigations using in vivo and in vitro studies are needed.
Methods
Experimental animals
A total of 52 healthy pregnant Sprague–Dawley (SD) rats (240–260 g) were purchased from Dashuo Experimental Animal Co., Ltd (Chengdu, China). Animals were fed breeding-stage special pelleted fodder at room temperature (22 °C) and 85% humidity. Sichuan University Committee on Animal Research approved all animal studies that were carried out in accordance with the approved guidelines.
CEPO preparation and identification
Carbamylated erythropoietin was prepared as described previously [13]. Briefly, 1 mL rhEPO (Merck, German) was mixed with 1 mol/L sodium borate (pH 8.8) and 162.22 mg potassium cyanate (KOCN) for a final concentration of KOCN at 1 mol/L. The mixture was incubated in a water bath (37 °C) for 24 h and then transferred into a dialysis bag. The contents were stirred to accelerate dialysis to remove excess KOCN at 4 °C in Milli-Q water followed by dialysis at 4 °C in 1000 mL solution (20 mmol/L sodium citrate and 0.1 mol/L NaCl, pH 6.0). The dialyzed solution was ultrafiltered (Ultrafiltration device, 10 kDa, Millipore) to a concentration > 20 μg/mL. CEPO concentration was measured using an ultramicro-spectrophotometer (Thermo Scientific Nanodrop 2000). Powder was obtained by using the freeze-dry method and stored at − 20 °C for subsequent use. The lysine digestion method [13] was used to confirm whether rhEPO was completely transformed to CEPO. 200 μg powder was solubilized in 200 μL of 6 mol/L guanidine hydrochloride or 250 mmol/L of Tris (pH 9.5). A volume of 25 μL of 0.1 mol/L dithiothreitol (DTE) was added to each solution and then incubated in the dark at 37 °C for 30 min. Then, 25 μL of 0.6 mol/L iodide acetamide was added, followed by incubation at room temperature for 60 min. Finally, 750 μL of 50 mmol/L ammonium bicarbonate and 0.4 mol/L urea were added, and the total volume of 1 mL was dialyzed against 50 mmol/L ammonium bicarbonate and 0.4 mol/L urea solution overnight, during which the dialysate was regularly changed. Concentration was measured using an ultramicro-spectrophotometer (Nanodrop 2000). Concurrently, 20 μg rhEPO or CEPO powder was added to 0.8 μg endoproteinase Lys-C (Calbiochem, Germany), and incubated for 20 h at 37 °C. The digested solution was electrophoresed using a 12% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE), and subsequently, the gel was analyzed by silver staining.
Pregnancy determination
Sprague–Dawley rats that had no prior mating were breed during the estrus phase (female:male = 2:1), and at 9:00 a.m. on the following day, the vaginal swabs were smeared. The detection of sperm in the vaginal smear was defined as pregnancy day 1. Rats were transferred to new cages until pregnancy day 19.
Intrauterine HI model
Intrauterine HI model was made based on the procedure used in Tanaka et al. [39]. 19-day pregnant rats were anesthetized with 1% pentobarbital sodium intraperitoneally (40 mg/kg, i.p.). A midline incision was performed in the lower abdomen that exposed both the uterine and ovarian arteries. The intrauterine hypoxic-ischemic state was induced using four artery clamps that restricted the bilateral uterine arteries for 30 min. During the clamping process, saline gauzes were frequently changed. The uterus and abdomen were kept warm using a heating lamp. After 30 min, the clamps were removed and the abdomen was sutured, and then transferred back to clean cages.
Animal grouping and treatment
A total of 52 pregnant SD rats were randomly divided into three groups: the sham operation group (sham, n = 4), the intrauterine hypoxic-ischemic reperfusion group (I/R, n = 4 at each time point, total 24 animals), and the CEPO pretreatment group before initiation of intrauterine hypoxic-ischemic operation (CEPO + I/R, n = 4 at each time point, total 24 animals). The I/R and CEPO + I/R groups were injected with 1 mL normal saline or CEPO (50 µg/kg) through the tail vein 30 min before the operation. The sham group underwent only an abdominal exposure operation without bilateral uterine artery ligation. Similar to the I/R and CEPO + I/R groups, the sham group was injected with 1 mL saline 30 min before the operation, and pups were delivered after 24 h by cesarean section. I/R and CEPO + I/R groups were observed for 6 time points, 0.5, 4, 8, 12, 24, and 48 h after intrauterine hypoxic-ischemic operation. At the corresponding time points above, the uterus horns of pregnant rats were opened, the pups were removed by cesarean section and sacrificed quickly on an ice table to obtain sample of the whole brain tissues for each time point. Some of the brains were frozen in liquid nitrogen, and then, stored at − 80 °C for Western blotting, while others were sliced into 5-μm paraffin-embedded sections for IHC staining, HE staining, and TUNEL staining. Sham group was designed to set only a time point for control compared with I/R group and CEPO + I/R group based on previous studies [25, 26].
Determining fetal mortality
The number of fetuses from each pregnant rat was recorded at the time of surgery, and the number of dead fetuses from each litter was recorded at the time of cesarean section. Fetal mortality was calculated as the number of dead fetuses divided by the total number of fetuses for each group. Results were expressed as percentages.
TUNEL staining
TUNEL staining was performed using the FragEL™ DNA Fragmentation Detection Kit, Colorimetric-terminal deoxynucleotidyl transferase (TdT) Enzyme (Merck). Briefly, sections were deparaffinized and permeabilized with 20 µg/mL proteinase K (pH 7.4–8.0) for 20 min at room temperature. Then, the sections were incubated with 3% H2O2 for 5 min at room temperature, followed by incubation with 1× TdT equilibrium buffer for 10 min at room temperature. After washing, the sections were incubated with TdT enzyme for 60 min at 37 °C. The reaction was terminated by incubation in a blocking/wash buffer for 10 min at room temperature. Subsequently, the sections were incubated with 100 μL of 1× conjugate for 30 min at room temperature and stained with 3,3-diaminobenzidine (DAB) solution in the dark for 10 min. Negative controls without TdT enzyme were also included for each assay. Cells were defined as TUNEL-positive if the nuclei were stained brown. For quantification, the number of TUNEL-positive cells was counted for every 100 cells using five view fields per section at 400× magnification using Image-Pro Plus 6.0 image analysis software. Apoptotic index was calculated as the number of TUNEL-positive cells divided by 100 cells and averaged.
Western blot analysis
Brain tissue was homogenized in radioimmunoprecipitation (RIPA) lysis buffer supplemented with phenylmethylsulfonylfluoride (PMSF) solution, a protease inhibitor. The homogenates were centrifuged (12,000×g for 10 min at 4 °C), and the total protein in the supernatant was measured using the BCA Protein Assay kit (Beyotime Biotechnology). An equivalent of 80 μg protein was analyzed by 15% SDS-PAGE and transferred to polyvinylidene difluoride (PVDF) membrane (Roche). Membranes were blocked with 5% (w/v) bovine serum albumin (Millipore, USA) in 10 mM Tris-buffered saline with 0.1% Tween 20 (TBS-T) for 2 h, and then probed overnight at 4 °C with specific primary antibodies: CC3 (1:500, Cell Signaling Technology) and β-actin (1:2000, Beijing Zhongshan Jinqiao Biological Technology Co. China). Subsequently, the membranes were incubated with HRP-conjugated goat anti-rabbit secondary antibody (1:3000, Beijing Zhongshan Jinqiao Biological Technology Co., China) for 1.5 h at room temperature. The specific protein bands were detected using enhanced chemiluminescence (ECL) Western blotting detection kit (Millipore), and the immunoreactive bands were digitally scanned and analyzed using Image J software. The band intensity of the target proteins was normalized against β-actin that was used as a loading control.
IHC
The paraffin-embedded brain sections were measured for Bax and Bcl-2 protein expression levels using ChemMate™ Envision + HRP/DAB Rabbit/Mouse Detection Kit (Gene Technology Shanghai Co., China) according to the manufacturer’s instructions. Briefly, coronal sections were deparaffinized and rehydrated. Antigen retrieval was performed by boiling the sections in 10 mM citrate buffer (pH 6.0) for 45 min. After washing with phosphate-buffered saline (PBS), the sections were incubated with 3% H2O2 in PBS in the dark for 15 min, followed by incubation with the following primary antibodies at 4 °C overnight: anti-Bcl-2 (1:200, Abcam) and anti- Bax (1:200, Abcam). Then, the sections were then incubated with ChemMate™ Envision + HRP for 45 min at room temperature, stained with 3,3-diaminobenzidine (DAB), and counterstained with hematoxylin. For negative controls, additional sections were treated similarly, albeit the primary antibody was omitted. Cells were defined as positive if the cytoplasm was stained brown. Images were obtained for five view fields per section at 400× magnification using an Olympus microscope. The integrated optical density (IOD) and the area of positively-stained tissues were obtained using Image-Pro Plus 6.0 software. The mean density (IOD/area) was calculated and averaged.
Statistical analysis
Data was expressed as mean ± standard deviation. Differences between the groups were analyzed by one-way ANOVA or Student’s t-test. The counting differences were analyzed by Fisher’s exact test. P < 0.05 was considered statistically significant.
Abbreviations
- HIE:
-
hypoxic-ischemic encephalopathy
- EPO:
-
erythropoietin
- rhEPO:
-
recombinant human erythropoietin
- CEPO:
-
carbamylated erythropoietin
- CNS:
-
central nervous system
- EPOR:
-
erythropoietin receptor
- BBB:
-
blood–brain barrier
- Lys-C:
-
carboxyl side of lysine
- HI:
-
ischemia–hypoxia
- I/R:
-
hypoxic-ischemic reperfusion
- CC3:
-
cleaved caspase-3
- IHC:
-
immunohistochemistry
- Bcl-2:
-
B cell lymphoma
- Bax:
-
Bcl-2 Associated X Protein
- SD:
-
Sprague–Dawley
- i.p.:
-
intraperitoneal
- KOCN:
-
potassium cyanate
- DTE:
-
dithiothreitol
- HE:
-
hematoxylin–eosin
- SDS-PAGE:
-
sodium dodecyl sulfate-polyacrylamide gel electrophoresis
- TUNEL:
-
terminal deoxynucleotidyl transferase-mediated dUTP nick end-labeling
- TdT:
-
terminal deoxynucleotidyl transferase
- RIPA:
-
radioimmunoprecipitation
- PMSF:
-
phenylmethylsulfonylfluoride
- PVDF:
-
polyvinylidene difluoride
- TBST:
-
tween 20
- ECL:
-
chemiluminescence
- PBS:
-
phosphate-buffered saline
- DAB:
-
3,3-diaminobenzidine
- IOD:
-
integrated optical density
References
Ambalavanan N, Carlo WA, Shankaran S, Bann CM, Emrich SL, Higgins RD, et al. Predicting outcomes of neonates diagnosed with hypoxemic-ischemic encephalopathy. Pediatrics. 2006;118(5):2084–93.
Verklan MT. The chilling details: hypoxic-ischemic encephalopathy. J Perinat Neonatal Nurs. 2009;23(1):59–68 (quiz 69-70).
Oza S, Lawn JE, Hogan DR, Mathers C, Cousens SN. Neonatal cause-of-death estimates for the early and late neonatal periods for 194 countries: 2000–2013. Bull World Health Organ. 2015;93(1):19–28.
Koury MJ, Bondurant MC. The molecular mechanism of erythropoietin action. Eur J Biochem. 1992;210(3):649–63.
Gilreath JA, Stenehjem DD, Rodgers GM. Diagnosis and treatment of cancer-related anemia. Am J Hematol. 2014;89(2):203–12.
Ohls RK, Christensen RD, Kamath-Rayne BD, Rosenberg A, Wiedmeier SE, Roohi M, et al. A randomized, masked, placebo-controlled study of darbepoetin alfa in preterm infants. Pediatrics. 2013;132(1):e119–27.
Akizawa T, Saito A, Gejyo F, Suzuki M, Nishizawa Y, Tomino Y, et al. Impacts of recombinant human erythropoietin treatment during predialysis periods on the progression of chronic kidney disease in a large-scale cohort study (Co-JET study). Ther Apher Dial. 2014;18(2):140–8.
Siren AL, Knerlich F, Poser W, Gleiter CH, Bruck W, Ehrenreich H. Erythropoietin and erythropoietin receptor in human ischemic/hypoxic brain. Acta Neuropathol. 2001;101(3):271–6.
Ma YS, Zhou J, Liu H, Du Y, Lin XM. Protection effect of recombiant human erythropoietin preconditioning against intrauterine hypoxic-ischemic brain injury and its influence on expression of caspase-3 protein in brain tissue. Sichuan Da Xue Xue Bao Yi Xue Ban. 2013;44(3):397–401.
Zhou J, Ma YS, Liu H, Lin XM. Permeability of exogenetic recombine human erythropoietin through placenta barrier to fetal rats with transient uteroplacental ischemia. Sichuan Da Xue Xue Bao Yi Xue Ban. 2010;41(3):445–7.
Coleman TR, Westenfelder C, Togel FE, Yang Y, Hu Z, Swenson L, et al. Cytoprotective doses of erythropoietin or carbamylated erythropoietin have markedly different procoagulant and vasoactive activities. Proc Natl Acad Sci USA. 2006;103(15):5965–70.
Oron G, Ben-Haroush A, Hod M, Orvieto R, Bar J. Serum-soluble CD40 ligand in normal pregnancy and in preeclampsia. Obstet Gynecol. 2006;107(4):896–900.
Leist M, Ghezzi P, Grasso G, Bianchi R, Villa P, Fratelli M, et al. Derivatives of erythropoietin that are tissue protective but not erythropoietic. Science. 2004;305(5681):239–42.
Lapchak PA, Kirkeby A, Zivin JA, Sager TN. Therapeutic window for nonerythropoietic carbamylated-erythropoietin to improve motor function following multiple infarct ischemic strokes in New Zealand white rabbits. Brain Res. 2008;1238:208–14.
Adembri C, Massagrande A, Tani A, Miranda M, Margheri M, De Gaudio R, et al. Carbamylated erythropoietin is neuroprotective in an experimental model of traumatic brain injury. Crit Care Med. 2008;36(3):975–8.
Savino C, Pedotti R, Baggi F, Ubiali F, Gallo B, Nava S, et al. Delayed administration of erythropoietin and its non-erythropoietic derivatives ameliorates chronic murine autoimmune encephalomyelitis. J Neuroimmunol. 2006;172(1–2):27–37.
Schmidt RE, Green KG, Feng D, Dorsey DA, Parvin CA, Lee JM, et al. Erythropoietin and its carbamylated derivative prevent the development of experimental diabetic autonomic neuropathy in STZ-induced diabetic NOD-SCID mice. Exp Neurol. 2008;209(1):161–70.
Ding J, Li QY, Yu JZ, Wang X, Lu CZ, Ma CG, et al. Carbamylated erythropoietin ameliorates hypoxia-induced cognitive and behavioral defects with the generation of choline acetyltransferase-positive neurons. J Neurosci Res. 2013;91(1):73–82.
Villa P, van Beek J, Larsen AK, Gerwien J, Christensen S, Cerami A, et al. Reduced functional deficits, neuroinflammation, and secondary tissue damage after treatment of stroke by nonerythropoietic erythropoietin derivatives. J Cereb Blood Flow Metab. 2007;27(3):552–63.
Bianchi R, Brines M, Lauria G, Savino C, Gilardini A, Nicolini G, et al. Protective effect of erythropoietin and its carbamylated derivative in experimental Cisplatin peripheral neurotoxicity. Clin Cancer Res. 2006;12(8):2607–12.
Wu CL, Chen SD, Yin JH, Hwang CS, Yang DI. Erythropoietin and sonic hedgehog mediate the neuroprotective effects of brain-derived neurotrophic factor against mitochondrial inhibition. Neurobiol Dis. 2010;40(1):146–54.
Bernal F, Saura J, Ojuel J, Mahy N. Differential vulnerability of hippocampus, basal ganglia, and prefrontal cortex to long-term NMDA excitotoxicity. Exp Neurol. 2000;161(2):686–95.
Fan TJ, Han LH, Cong RS, Liang J. Caspase family proteases and apoptosis. Acta Biochim Biophys Sin. 2005;37(11):719–27.
Young C, Roth KA, Klocke BJ, West T, Holtzman DM, Labruyere J, et al. Role of caspase-3 in ethanol-induced developmental neurodegeneration. Neurobiol Dis. 2005;20(2):608–14.
Zhao F, Qu Y, Xiong T, Duan Z, Ye Q, Mu D. The neuroprotective role of TERT via an antiapoptotic mechanism in neonatal rats after hypoxia–ischemia brain injury. Neurosci Lett. 2012;515(1):39–43.
Chen H, Xiong T, Qu Y, Zhao F, Ferriero D, Mu D. mTOR activates hypoxia-inducible factor-1alpha and inhibits neuronal apoptosis in the developing rat brain during the early phase after hypoxia–ischemia. Neurosci Lett. 2012;507(2):118–23.
Millet A, Bouzat P, Trouve-Buisson T, Batandier C, Pernet-Gallay K, Gaide-Chevronnay L, et al. Erythropoietin and its derivates modulate mitochondrial dysfunction after diffuse traumatic brain injury. J Neurotrauma. 2016;33(17):1625–33.
He H, Qiao X, Wu S. Carbamylated erythropoietin attenuates cardiomyopathy via PI3K/Akt activation in rats with diabetic cardiomyopathy. Exp Ther Med. 2013;6(2):567–73.
Tsujimoto Y. Cell death regulation by the Bcl-2 protein family in the mitochondria. J Cell Physiol. 2003;195(2):158–67.
Martinou JC, Youle RJ. Mitochondria in apoptosis: Bcl-2 family members and mitochondrial dynamics. Dev Cell. 2011;21(1):92–101.
Adams JM, Cory S. Bcl-2-regulated apoptosis: mechanism and therapeutic potential. Curr Opin Immunol. 2007;19(5):488–96.
Murphy KM, Streips UN, Lock RB. Bcl-2 inhibits a Fas-induced conformational change in the Bax N terminus and Bax mitochondrial translocation. J Biol Chem. 2000;275(23):17225–8.
Rong YP, Bultynck G, Aromolaran AS, Zhong F, Parys JB, De Smedt H, et al. The BH4 domain of Bcl-2 inhibits ER calcium release and apoptosis by binding the regulatory and coupling domain of the IP3 receptor. Proc Natl Acad Sci USA. 2009;106(34):14397–402.
Wang Y, Zhang ZG, Rhodes K, Renzi M, Zhang RL, Kapke A, et al. Post-ischemic treatment with erythropoietin or carbamylated erythropoietin reduces infarction and improves neurological outcome in a rat model of focal cerebral ischemia. Br J Pharmacol. 2007;151(8):1377–84.
Xiong Y, Mahmood A, Zhang Y, Meng Y, Zhang ZG, Qu C, et al. Effects of posttraumatic carbamylated erythropoietin therapy on reducing lesion volume and hippocampal cell loss, enhancing angiogenesis and neurogenesis, and improving functional outcome in rats following traumatic brain injury. J Neurosurg. 2011;114(2):549–59.
Netto CA, Sanches EF, Odorcyk F, Duran-Carabali LE, Sizonenko SV. Pregnancy as a valuable period for preventing hypoxia–ischemia brain damage. Int J Dev Neurosci. 2018;70:12–24.
Charriaut-Marlangue C, Besson VC, Baud O. Sexually dimorphic outcomes after neonatal stroke and hypoxia–ischemia. Int J Mol Sci. 2017;19(1):61.
Xiong T, Qu Y, Wang H, Chen H, Zhu J, Zhao F, et al. GSK-3beta/mTORC1 couples synaptogenesis and axonal repair to reduce hypoxia ischemia-mediated brain injury in neonatal rats. J Neuropathol Exp Neurol. 2018;77(5):383–94.
Tanaka M, Natori M, Ishimoto H, Miyazaki T, Kobayashi T, Nozawa S. Experimental growth retardation produced by transient period of uteroplacental ischemia in pregnant Sprague–Dawley rats. Am J Obstet Gynecol. 1994;171(5):1231–4.
Authors’ contributions
MD and HL helped in designing and conducting the study, extracting the data, and writing the manuscript. YQ helped in designing the study. YM helped in editing the manuscript and also provided statistical support. XL helped in designing the study and editing the manuscript. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to thank the Key Laboratory of Birth Defects and Related Diseases of Women and Children for supporting this study.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
All data generated or analyzed for this study are included in the article.
Consent of publication
All the authors listed have approved the manuscript for publication.
Ethics approval and consent to participate
This study was conducted with the approval of the Institutional Animal Ethics Committee of Sichuan University (2016059A).
Funding
This study was supported by the National Science Foundation of China (No. 81871192, No. 81330016), the Grants from Science and Technology Bureau of Sichuan Province (2016SZ0048), and the Grant from Chengdu Science and Technology Bureau (2014-HM01-00059-SF).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Diao, M., Qu, Y., Liu, H. et al. Effect of carbamylated erythropoietin on neuronal apoptosis in fetal rats during intrauterine hypoxic-ischemic encephalopathy. Biol Res 52, 28 (2019). https://doi.org/10.1186/s40659-019-0234-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40659-019-0234-7