Abstract
Purpose
While most Achilles tendon ruptures are dramatic and diagnosed quickly, some are missed, with a risk of becoming chronic. A chronic Achilles tendon rupture is defined as a rupture that has been left untreated for more than 4 weeks. By mapping the health economic cost of chronic Achilles tendon ruptures the health-care system might be able to better distribute resources to detect these ruptures at an earlier time.
Method
All patients with a chronic Achilles tendon rupture who were treated surgically at Sahlgrenska University Hospital or Kungsbacka Hospital between 2013 and 2018 were invited to participate in the study. The patients were evaluated postoperatively using the validated Achilles tendon Total Rupture Score (ATRS). The health-care costs were assessed using clinical records. The production-loss costs were extracted from the Swedish Social Insurance Agency. The cost of chronic Achilles tendon ruptures was then compared with the cost of acute ruptures in a previous study by Westin et.al.
Results
Forty patients with a median (range) age of 66 (28–86) were included in the study. The mean total cost (± SD) for the patients with a chronic Achilles tendon rupture was 6494 EUR ± 6508, which is 1276 EUR higher than the mean total cost of acute ruptures. Patients with chronic Achilles tendon ruptures reported a mean (min-max) postoperative ATRS of 73 (14–100).
Conclusion
Missing an Achilles tendon rupture will entail higher health-care costs compared with acute ruptures. Health-care resources can be saved if Achilles tendon ruptures are detected at an early stage.
Similar content being viewed by others
Introduction
The Achilles tendon is the strongest tendon in the human body [6]. It is, however, one of the most commonly injured [12]. The incidence of Achilles tendon rupture is approximately 23–47 per 100,000 person-years for men and 8–12 per 100,000 person-years for women [9, 11]. The incidence has increased over the last few decades [7, 9]. The most probable explanation is that more people exercise and participate in sports at an older age. Due to the strength of the Achilles tendon, the rupture is commonly dramatic and is characterized by a loud “snap” and acute pain [10]. There are also ruptures that have a more discrete debut [20]. The atypical presentations of Achilles tendon ruptures are more frequent in the elderly and sedentary population and they are also the ones that are usually missed and become chronic [14].
A chronic Achilles tendon rupture is by the literature defined as a rupture that has been left untreated for more than 4 weeks after the initial injury [8, 17]. The reason why the rupture remains untreated depends on the event, the patient’s experience of the injury and the clinical examination [16]. Of all Achilles tendon ruptures, 10–25% are missed and therefore risk becoming chronic [3, 20]. Patients with chronic Achilles tendon ruptures more frequently complain about pain, recurrent swelling, an affected gait pattern and an inability to climb stairs [13].
A variety of surgical techniques have been described to treat chronic Achilles tendon ruptures. Examples include augmentations, V-Y tendon reconstruction, free flaps, tendon transfers and turndown flaps [1, 13, 21]. In contrast to an acute Achilles tendon rupture, chronic ruptures, are suggested to require a surgical intervention [17]. In most cases, the surgical intervention of a chronic Achilles tendon rupture is more demanding and is associated with greater risks than the intervention in an acute Achilles tendon rupture [19]. Normal end-to-end sutures are not regarded as an acceptable treatment and some kind of reinforcement is commonly recommended [1, 2, 15].
Many studies have reported different surgical methods after chronic Achilles tendon ruptures [13, 18, 21, 24]. However, there are no studies that have evaluated the economic cost of chronic Achilles tendon ruptures. The purpose of this study was to analyze the economic cost of chronic Achilles tendon ruptures. A secondary aim was to present the pre- and postoperative ankle function in patients with chronic Achilles tendon ruptures using the Achilles tendon Total Rupture Score (ATRS).
Material and methods
Data collection and study population
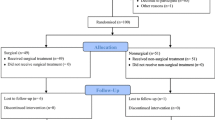
The patients in this study were all presented at Sahlgrenska University Hospital and Kungsbacka Hospital between 2013 and 2018. The included patients were found through identifying all patients with Achilles tendon ruptures that were operatively treated at the designated hospitals during the selected time period. The medical history and clinical evaluation was later examined for all identified patients. The criterion for inclusion was any type of unilateral Achilles tendon rupture that had been left untreated for more than 4 weeks and could therefore be classified as chronic. The diagnosis was based on the trauma described, the clinical examination and, in some cases, inspection with ultrasonography. Due to the rarity of chronic Achilles tendon ruptures, no exclusion criteria were used. Fifty-nine patients were identified. Every patient received a letter with information about the study and two Achilles tendon Total Rupture Score questionnaires (ATRS) to evaluate their pre- and postoperative ankle function. Both ATRS questionnaires were filled out retrospectively at the same time by the patient 1 year after surgical repair. Out of the patients identified, 40 patients chose to participate, and got included in the study. All the included patients gave their written consent to take part in the study. Ethical approval was obtained from the regional ethics review board in Sweden (DNR 554–15).
The health-economic cost was calculated as the sum of the surgical costs, other health-care costs related to hospital stays and complications, and the production loss due to sick leave. The health-care costs were extracted from the accounting database at Sahlgrenska University Hospital and the production loss (sick leave) was collected from the Swedish Social Insurance Agency. The health-care costs used in this study are presented in Table 1. The data was later compared with statistics from the economic study performed by Westin et al. [27]. In that study, the economic cost of the operative and nonoperative treatment of acute Achilles tendon ruptures at the same Sahlgrenska University Hospital between 2009 and 2010 were analyzed. The extracted data were collected from the randomized controlled study performed by Olsson et al. [23]. The health-care and production-loss cost of chronic Achilles tendon ruptures in the present study were examined in comparison with the cost of both the operative and nonoperative treatment of acute Achilles tendon ruptures. The costs of physical therapy visits were excluded due to a high number of patients going to privately financed physiotherapists. The function was evaluated using the ATRS.
Treatment method
All the patients included in the study were treated operatively. The surgical method used was the surgical technique described by Nilsson-Helander et al. [21] The method is based on the augmentation of the ruptured tendon with a free gastrocnemius aponeurosis flap. Following surgery, the patient’s foot was placed in an equinus position with a below-the-knee plaster cast. This cast was worn for 3 weeks, followed by 3 weeks in a more natural position. After 6 weeks the patients were able to start range-of-motion training in an adjustable ankle brace (DonJoy ROM Walker) for a further 2 weeks. Weight-bearing was successively increased during this period. The total number of days with ankle immobilization was thus 8 weeks.
Economic costs
The economic costs were classified as either health-care costs or production losses. The direct health-care costs were based on costs extracted from the accounting database at Sahlgrenska University Hospital. The expenses included the cost of administration, hospital wages, surgeon salaries, anesthesia and inpatient nights. Table 1 shows the health-care costs that were considered in the study. The economic costs associated with the production loss depend on the number of sick-leave days and the gross wage of the patient. All the costs were converted from SEK to EUR using the 2013 exchange rate (1 EUR = 8.86 SEK = 1.33 USD).
Patient-reported outcomes
This study uses the validated Achilles tendon Total Rupture Score (ATRS) [22] to evaluate functional outcomes among patients with a chronic Achilles tendon rupture.
Statistical analysis
The economic costs were expressed in euros and analyzed as continuous variables summarized in the arithmetic mean and standard deviation and 95% confidence intervals. Parametric statistical tests for significant differences in economic costs between chronic and acute ruptures were based on the assumption of normally distributed data. Sensitivity checks of statistical significance tests were performed using non-parametric bootstrapping. P-values below 0.05 were considered statistically significant.
Results
Demographics
A total of 40 consecutive patients decided to participate in the study (29 males and 11 females). The median age (range) was 66 (28–86). Table 2 presents a summary of the demographic and clinical variables. The demographic and clinical variables of patients who did not choose to participate (non-response) are also presented. There were no evident demographic differences between the two groups.
Economic cost
Table 3 presents the mean (CI 95%; lower-upper) economic cost per patient for chronic Achilles tendon ruptures in terms of health-care, production losses and total costs. The mean (± SD) health-care cost of chronic Achilles tendon ruptures in the study was 3821 EUR ± 752. When combined with the production-loss cost of chronic Achilles tendon ruptures, this equals a mean (± SD) total cost of 6494 EUR ± 6508. The production-loss cost presented here includes both working patients and patients that have retired from work. When working patients (n = 22) were analyzed exclusively, the mean (± SD) production-loss cost was 6831 EUR ± 4861 instead of 2673 EUR ± 6625. The total cost of chronic Achilles tendon ruptures is therefore considerably higher when it affects working patients.
Table 3 also shows a comparison between the cost per patient of chronic Achilles tendon ruptures and acute Achilles tendon ruptures. All the results are adjusted for gender and age. The results demonstrate a higher health-care cost for chronic Achilles tendon ruptures than both the operative and nonoperative treatment of acute Achilles tendon ruptures. The mean difference in health-care costs between chronic ruptures and the nonoperative treatment of an acute rupture was 3079 EUR and between chronic ruptures and the operative repair of an acute rupture 675 EUR. All differences regarding health-care costs were statistically significant (P < 0.01). Table 3 also presents production-loss and total costs per patient for each group. There were no significant differences in production-loss costs between the three groups (Fig. 1).
When comparing the total cost, regardless of treatment, of chronic Achilles tendon ruptures and acute Achilles tendon ruptures, a non-significant mean cost difference of 1276 EUR (P-value = 0.11) is seen.
Patient-reported outcome
Patients with a chronic Achilles tendon rupture reported an improvement in the ATRS from initial injury to 1 year after treatment. The mean (± SD) preoperative ATRS was 16.2 ± 13.0 and the mean (± SD) postoperative ATRS was 73.2 ± 22.7, (P < 0.001). The scores are presented in Table 4.
Discussion
The most important finding of this study is that chronic Achilles tendon ruptures are more expensive than acute Achilles tendon ruptures. Another important finding was that patients with chronic Achilles tendon ruptures reported improved ankle function 1 year after operative repair and rehabilitation. This indicates that the treatment of chronic Achilles tendon ruptures is effective, even though it requires more resources than the treatment of acute Achilles tendon ruptures. The direct health-care costs were higher for chronic Achilles tendon ruptures, regardless of whether the acute Achilles tendon ruptures were treated operatively or nonoperatively. It can be assumed that the reason for the higher costs is the more complicated surgical technique required when treating chronic Achilles tendon ruptures. The more difficult procedure results in longer operating times and higher costs.
When analyzing the health-economic cost of an injury, it is important to consider the patient-reported outcome. The mean postoperative ATRS reported by patients with chronic Achilles tendon ruptures was 73 points of 100. The mean preoperative ATRS was 16. This indicates that the surgical repair of chronic Achilles tendon ruptures will result in significantly improved ankle function. In comparison, patients surgically treated for an acute Achilles tendon rupture at the same hospitals reported a slightly higher ATRS of 82 points 12 months after the initial injury [23]. The non-surgically treated patients scored 80 in the same trial. This means that, in addition to a higher economic cost, chronic Achilles tendon ruptures may be associated with more patient-reported limitations in ankle function than acute Achilles tendon ruptures. There is no official MCID (Minimal Clinically Important Difference) for ATRS. However, earlier studies have defined the MCID as 8–10 points [5, 26]. Both the preoperative and the postoperative ATRS were filled out retrospectively. This entails an immense recall bias. This is a notable drawback of the study.
Prior to this study, there have only been a few health-economic studies that have evaluated the economic cost of Achilles tendon ruptures. Truntzer et al. [25] and Westin et al. [27] have evaluated whether operative or nonoperative treatment is economically favorable when it comes to Achilles tendon ruptures. Moreover, Carmont et al. [4] compared the economic impact of the open and percutaneous repair of Achilles tendon ruptures.
The study performed by Truntzer et al. [25] showed that the cost of a nonoperative approach to acute Achilles tendon ruptures was significantly lower than that of an operative approach. However, the study was limited to direct costs and did not consider the economic impact of performance loss and costs related to quality of life. As a result, the costs that were considered were only analyzed from the perspective of health-care and not of the patient. Westin et al. [27] therefore conducted a health-economic study where production-loss costs (indirect costs) and the cost per gained QALY were examined. The study reported that operative treatments are more expensive, but that they could be regarded as equally cost effective if there is a willingness to pay 50,000 EUR/QALY. The cost of re-ruptures was not included. Carmont et al. [4] reported that the percutaneous repair of the Achilles tendon is a cost-effective alternative to open repair of the tendon. Chronic Achilles tendon ruptures are still thought to require an open repair, as described in the study by Nilsson-Helander et al. [21]. They evaluated the functional- and patient-reported outcome of a surgical method applied to both chronic Achilles tendon ruptures and re-ruptures. They did not, however, consider economic costs and did not analyze chronic Achilles tendon ruptures exclusively.
The limitation of this study is that the age of patients with chronic Achilles tendon ruptures is considerably higher than that of patients with acute Achilles tendon ruptures. Consequently, more patients have retired from work and therefore lack information about loss of income due to sick leave and fewer working hours. This results in lower production-loss costs and thereby a lower total cost for these ruptures. When exclusively analyzing the production-loss cost for working patients, the cost was considerably higher. Older age may potentially also have affected the patient-reported outcome and ATRS. This is the reason why no direct comparison regarding ATRS, between chronic Achilles tendon ruptures and acute Achilles tendon ruptures, was made. To determine the total cost difference between acute and chronic Achilles tendon ruptures and their patient-reported outcome, a larger cohort is required. The persistent challenge is that chronic Achilles tendon ruptures are relatively uncommon and thereby difficult to recruit for studies on a larger scale. Another limitation is that physiotherapy costs had to be excluded. Patients with chronic Achilles tendon ruptures often need an extensive time to rehabilitate. However, due to the age difference between the groups, the patients with chronic Achilles tendon ruptures may have lower functional requirements than the younger group of patients with acute Achilles tendon rupture. Therefore, the exclusion of physiotherapy visits, might affect the result in both ways. For a more precise analysis, an inclusion of physiotherapy costs would be eligible.
The health-economic costs analyzed in this study are based on the Swedish health-care system and may not be applicable to other countries with different health-care structures. Due to the limited number of females included in the study, no gender comparison was performed. The strength of the study is, however, that it analyzes chronic Achilles tendon ruptures exclusively.
Conclusion
The treatment of patients with a chronic Achilles tendon rupture is more expensive than the treatment of acute Achilles tendon ruptures. The main reason is the significantly higher costs of operative intervention. Moreover, the operative repair of chronic Achilles tendon ruptures improved the ankle function among patients. Patients with chronic Achilles tendon ruptures might, however, still have an inferior patient-reported outcome compared to patients with acute Achilles tendon ruptures. This indicates that patients with chronic Achilles tendon ruptures have persistent limitations after surgery and that more resources are required to detect these ruptures at an earlier stage.
Availability of data and materials
Data will not be shared. All data used is presented in the manuscript.
References
Abraham E, Pankovich AM (1975) Neglected rupture of the Achilles tendon. Treatment by VY tendinous flap. J Bone Joint Surg Am 57(2):253–255
Barnes MJ, Hardy AE (1986) Delayed reconstruction of the calcaneal tendon. J Bone Joint Surg Br 68(1):121–124
Carden DG, Noble J, Chalmers J, Lunn P, Ellis J (1987) Rupture of the calcaneal tendon. The early and late management. J Bone Joint Surg Br 69(3):416–420
Carmont MR, Heaver C, Pradhan A, Mei-Dan O, Gravare SK (2013) Surgical repair of the ruptured Achilles tendon: the cost-effectiveness of open versus percutaneous repair. Knee Surg Sports Traumatol Arthrosc 21(6):1361–1368
Costa M, Achten J, Marian I, Dutton S, Lamb S, Ollivere B et al (2020) Plaster cast versus functional brace for non-surgical treatment of Achilles tendon rupture (UKSTAR): a multicentre randomised controlled trial and economic evaluation. Lancet 395(10222):441–448
Doral MN, Alam M, Bozkurt M, Turhan E, Atay OA, Donmez G et al (2010) Functional anatomy of the Achilles tendon. Knee Surg Sports Traumatol Arthrosc 18(5):638–643
Egger AC, Berkowitz MJ (2017) Achilles tendon injuries. Curr Rev Musculoskelet Med 10(1):72–80
Gabel S, Manoli A 2nd. (1994) Neglected rupture of the Achilles tendon. Foot Ankle Int 15(9):512–517
Ganestam A, Kallemose T, Troelsen A, Barfod KW (2016) Increasing incidence of acute Achilles tendon rupture and a noticeable decline in surgical treatment from 1994 to 2013. A nationwide registry study of 33,160 patients. Knee Surg Sports Traumatol Arthrosc 24(12):3730–3737
Gross CE, Nunley JA 2nd. (2016) Acute Achilles tendon ruptures. Foot Ankle Int 37(2):233–239
Huttunen TT, Kannus P, Rolf C, Fellander-Tsai L, Mattila VM (2014) Acute achilles tendon ruptures: incidence of injury and surgery in Sweden between 2001 and 2012. Am J Sports Med 42(10):2419–2423
Jozsa L, Kvist M, Balint BJ, Reffy A, Jarvinen M, Lehto M et al (1989) The role of recreational sport activity in Achilles tendon rupture. A clinical, pathoanatomical, and sociological study of 292 cases. Am J Sports Med 17(3):338–343
Kraeutler MJ, Purcell JM, Hunt KJ (2017) Chronic Achilles tendon ruptures. Foot Ankle Int. 38(8):921–929
Lantto I, Heikkinen J, Flinkkila T, Ohtonen P, Leppilahti J (2015) Epidemiology of Achilles tendon ruptures: increasing incidence over a 33-year period. Scand J Med Sci Sports 25(1):e133–e138
Leslie HD, Edwards WH (2005) Neglected ruptures of the Achilles tendon. Foot Ankle Clin 10(2):357–370
Maffulli N (1999) Rupture of the Achilles tendon. J Bone Joint Surg Am 81(7):1019–1036
Maffulli N, Ajis A, Longo UG, Denaro V (2007) Chronic rupture of tendo Achillis. Foot Ankle Clin 12(4):583–596 vi
Maffulli N, Oliva F, Costa V, Del Buono A (2015) The management of chronic rupture of the Achilles tendon: minimally invasive peroneus brevis tendon transfer. Bone Joint J 97-b(3):353–357
Maffulli N, Via AG, Oliva F (2015) Chronic Achilles tendon disorders: Tendinopathy and chronic rupture. Clin Sports Med 34(4):607–624
Maffulli N, Via AG, Oliva F (2017) Chronic Achilles tendon rupture. Open Orthop J 11:660–669
Nilsson-Helander K, Sward L, Silbernagel KG, Thomee R, Eriksson BI, Karlsson J (2008) A new surgical method to treat chronic ruptures and reruptures of the Achilles tendon. Knee Surg Sports Traumatol Arthrosc 16(6):614–620
Nilsson-Helander K, Thomee R, Silbernagel KG, Thomee P, Faxen E, Eriksson BI et al (2007) The Achilles tendon Total rupture score (ATRS): development and validation. Am J Sports Med 35(3):421–426
Olsson N, Silbernagel KG, Eriksson BI, Sansone M, Brorsson A, Nilsson-Helander K et al (2013) Stable surgical repair with accelerated rehabilitation versus nonsurgical treatment for acute Achilles tendon ruptures: a randomized controlled study. Am J Sports Med 41(12):2867–2876
Restuccia G, Lippi A, Casella F, Citarelli C, Sacchetti F, Benifei M (2017) Chronic Achilles tendon rupture treated with allograft: a case report. Surg Technol Int 30:321–324
Truntzer JN, Triana B, Harris AHS, Baker L, Chou L, Kamal RN (2017) Cost-minimization analysis of the Management of Acute Achilles Tendon Rupture. J Am Acad Orthop Surg 25(6):449–457
Westin O, Sjögren T, Svedman S, Horvath A, Hamrin Senorski E, Samuelsson K et al (2020) Treatment of acute Achilles tendon rupture – a multicentre, non-inferiority analysis. BMC Musculoskelet Disord 21(1):358
Westin O, Svensson M, Nilsson Helander K, Samuelsson K, Gravare Silbernagel K, Olsson N et al (2018) Cost-effectiveness analysis of surgical versus non-surgical management of acute Achilles tendon ruptures. Knee Surg Sports Traumatol Arthrosc 26(10):3074–3082
Acknowledgements
No other acknowledgements than the authors listed above.
Funding
No external funding was used in the study. Open access funding provided by University of Gothenburg.
Author information
Authors and Affiliations
Contributions
All authors contributed by collecting data and writing this article. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All patients included in the study gave their written consent to participate. Ethical approval was obtained from the regional ethics review board in Sweden (DNR 554–15).
Consent for publication
Not applicable.
Competing interests
Niklas Nilsson has no financial conflicts of interest to disclose. Mikael Svensson has no financial conflicts of interest to disclose. Katarina Nilsson Helander has no financial conflicts of interest to disclose. Anna Holm has no financial conflicts of interest to disclose. Eric Hamrin Senorski has no financial conflicts of interest to disclose. Jón Karlsson has no financial conflicts of interest to disclose. Olof Westin has no financial conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nilsson, N., Nilsson Helander, K., Hamrin Senorski, E. et al. The economic cost and patient-reported outcomes of chronic Achilles tendon ruptures. J EXP ORTOP 7, 60 (2020). https://doi.org/10.1186/s40634-020-00277-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40634-020-00277-z