Abstract
Background
Research suggests antihypertensive medications are associated with fractures in older adults, however results are inconsistent and few have examined how the association varies over time. We sought to examine the association between antihypertensive class and incident non-vertebral fractures among older adults initiating monotherapy according to time since initiation.
Methods
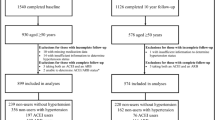
We used a new-user cohort design to identify Medicare beneficiaries (≥ 65 years of age) initiating antihypertensive monotherapy during 2008–2011 using a 20% random sample of Fee-For-Service Medicare beneficiaries enrolled in parts A (inpatient services), B (outpatient services), and D (prescription medication) coverage. Starting the day after the initial antihypertensive prescription, we followed beneficiaries for incident non-vertebral fractures. We used multinomial logistic regression models to estimate propensity scores for initiating each antihypertensive drug class. Using these propensity scores, we weighted beneficiaries to achieve the same baseline covariate distribution as beneficiaries initiating with angiotensin-converting enzyme inhibitors. Lastly, we used weighted Cox proportional hazard models to estimate hazard ratios (HRs) of having an incident fractures according to antihypertensive class and time since initiation.
Results
During 2008–2011, 122,629 Medicare beneficiaries initiated antihypertensive monotherapy (mean age 75, 61% women, 86% White). Fracture rates varied according to days since initiation and antihypertensive class. Beneficiaries initiating with thiazides had the highest fracture rate in the first 14 days following initiation (438 per 10,000 person-years, 95% confidence interval (CI): 294–628; HR: 1.40, 0.78–2.52). However, beneficiaries initiating with calcium channel blockers had the highest fracture rate during the 15–365 days after initiation (435 per 10,000 person-years, 95% CI: 404–468; HR: 1.11, 1.00–1.24). Beneficiaries initiating with angiotensin-receptor blockers had the lowest fracture rates during the initial 14 days (333 per 10,000 person-years, 190–546, HR: 0.92, 0.49–1.75) and during 15–365 days after initiation (321 per 10,000 person-years, 287–358, HR: 0.96, 0.84–1.09).
Conclusion
The association between antihypertensives and fractures varied according to class and time since initiation. Results suggest that when deciding upon antihypertensive therapy, clinicians may want to consider possible fracture risks when choosing between antihypertensive drug classes.
Similar content being viewed by others
Background
Fractures are one of the most common fall-related injuries for adults over the age of 65 (DeGrauw et al. 2016). In older adults, fractures are associated with high medical costs, loss of independence, and an increased risk of mortality (Stevens et al. 2006; Leibson et al. 2002; Tinetti and Williams 1997; Haentjens et al. 2010). Older adults are at greater risk of fractures due to decreased bone mineral density (BMD), decreased physical activity, and increased comorbidities (Marks et al. 2003). Comorbidities such as cardiovascular disease, osteoporosis, Parkinson’s disease, and diabetes can increase fracture risk (Woolf and Åkesson 2003; Lee et al. 2015). Medications increasing the risk of fractures include opioids, benzodiazepines, antidepressants, antiepileptics, and skeletal muscle relaxants (Fraser et al. 2014; By the American Geriatrics Society 2015 Beers Criteria Update Expert Panel 2015; Takkouche et al. 2007). Recently, research suggests antihypertensives may increase the risk of fall-related injury by as much as 11% among older adults (Butt and Harvey 2015; Tinetti et al. 2014).
Antihypertensives are associated with fractures through medication-related adverse events and by interactions with BMD (Berry and Kiel 2014). In the first few weeks after initiation, antihypertensives can increase the risk of falls and subsequent fractures due to medication-related adverse events, such as orthostatic hypotension (Butt and Harvey 2015; Zia et al. 2015). Orthostatic hypotension is defined as a decrease in blood pressure upon standing (Gupta and Lipsitz 2007), and is associated with an elevated risk of falls and fractures among hypertensive adults (Gangavati et al. 2011). Additionally, antihypertensives have been found to impact BMD in observational and clinical studies. For instance, thiazide diuretics reduce urinary calcium secretion and can stimulate osteoblasts potentially providing a protective effect for fractures (Ghosh and Majumdar 2014; Ruths et al. 2015; Solomon et al. 2011). Angiotensin-receptor blockers and angiotensin-converting enzyme inhibitors are believed to impact BMD by inhibiting bone turnover caused by the renin-angiotensin-aldosterone system (Ghosh and Majumdar 2014).
Prior research has found inconsistent results regarding the strength and direction of the association between antihypertensives and fractures (Butt and Harvey 2015; Zang 2013). Some studies have found antihypertensives increase the risk of fractures (Tinetti et al. 2014; Choi et al. 2015; Butt et al. 2012), while others have found no association (Fraser et al. 2014), or a protective association with fractures (Ruths et al. 2015; Solomon et al. 2011; Rejnmark et al. 2006). Few studies have examined the initial increased risk of fractures associated with starting antihypertensive therapy, and how the association between antihypertensives and fractures varies time. Therefore, we sought to examine the association between antihypertensives and incident non-vertebral fractures within the first year of initiation among Medicare beneficiaries. Specifically, we hypothesized that fractures in the first 2 weeks would be due to medication-related adverse events and fractures that occurred between 2 weeks and 1 year of use would be due to possible BMD effects.
Methods
Data source
We used a 20% nationwide, random sample of fee-for-service Medicare beneficiaries who were enrolled at least 1 month in Medicare Parts A (inpatient care), B (outpatient care), and D (prescription drugs) coverage between 2007 and 2011. Data were obtained under a data use agreement established with the Centers for Medicaid and Medicare Services (CMS) and the University of North Carolina at Chapel Hill (UNC-CH). The study protocol was approved by UNC’s Non-Biomedical Institutional Review Board.
New users of antihypertensive monotherapy
The study cohort consisted of all new users of antihypertensive medication initiating during 2008–2011 who were continuously enrolled in Medicare Parts A, B, and D for at least 12 months prior to initiation. New use was defined as not having a prior prescription of the following antihypertensive medications in the last 12 months: angiotensin-converting enzyme inhibitors (ACE), angiotensin-receptor blockers (ARB), beta blockers (BB), calcium channel blockers (CCB), or thiazide diuretics (THZ). We limited the cohort to beneficiaries initiating with monotherapy (e.g., one class of antihypertensive drug) since we were interested in examining differences in effect by drug class. Loop diuretics were excluded from the exposure definition since these drugs are typically prescribed for different indications and are a marker of increased short-term mortality in to older adults (Glynn et al. 2001).
We excluded beneficiaries who were originally eligible for Medicare due to end stage renal disease or disability and those beneficiaries with prior nursing home stays since not all medications dispensed in the nursing home are captured in Part D data. Additionally, we excluded beneficiaries who had a previous diagnoses for tremors or congestive heart failure since these health conditions could result in being prescribed antihypertensives. Since we were interested in capturing incident fractures and since prior falls can increase future fall and fracture risk (Pohl et al. 2014), we excluded beneficiaries who had prior falls or fractures. Finally, we required a second antihypertensive fill within 30 days of the end of the index drug’s days supply to exclude those beneficiaries who filled the first prescription and never returned (Additional file 1: Figure S1). We did not exclude beneficiaries with chronic kidney disease or diabetes, despite these being indications for certain antihypertensive drug classes, however we did conduct sub-analyses excluding these beneficiaries (see Statistical Analysis).
Initiation of antihypertensive therapy
Prescription medication data were identified using Medicare Part D. Using fill dates, we identified the date of the initial prescription for antihypertensive therapy (index date). Antihypertensive medications were identified using National Drug Codes and generic drug names (Additional file 1: Table S1). These specific drug classes were chosen based on the current recommendations for hypertension treatment in older adults (James et al. 2014).
Incident non-vertebral fractures
Incident non-vertebral fractures within 12 months of initiating antihypertensive monotherapy were our primary outcome. Starting the day after the index date, we followed beneficiaries until the first fracture event. Fractures were identified using validated diagnostic and procedure codes in Medicare Parts A and B (Additional file 1: Table S2) (Ray et al. 1992). We chose to examine fractures instead of falls since the accuracy of fall reporting varies by state and has low specificity in claims data (Annest et al. 2008). We excluded fractures that had a corresponding external cause-of-injury relating to motor vehicle crashes (E810-E825) and those that occurred on the index date.
In sub-analyses, we grouped fractures according to the anatomical location to distinguish between fractures that were likely related to low BMD. Low BMD fractures, or osteoporotic fractures, are typically defined as fractures occurring at the hip, radius, or vertebrae (Johnell and Kanis 2005). Since incident vertebral fractures are not well captured in claims data (Curtis et al. 2009), we defined probable low BMD fractures as any fracture event involving the hip or radius. All other non-vertebral fractures were classified as probable normal BMD fractures.
Risk factors for fractures
Covariates were selected based on the previous literature (Woolf and Åkesson 2003; Lee et al. 2015; By the American Geriatrics Society 2015 Beers Criteria Update Expert Panel 2015; Zia et al. 2015; Nurminen et al. 2013) and were defined based on claims during the 12 months prior to initiation (Additional file 1: Table S3). Covariates included: demographics (age, gender, and race), concurrent medication use and prior use of medications associated with fractures (loop diuretics, antiarrhythmics, antidepressants, antiepileptics, anxiolytics, benzodiazepines, bisphosphonates, antipsychotics, skeletal muscle relaxants, opioids, and hypnotics), codes for chronic comorbidities associated with fracture risk (diabetes, chronic kidney disease, Parkinson’s disease, Alzheimer’s disease, osteoporosis, arrhythmia, osteoarthritis, rheumatoid arthritis, stroke, myocardial infarction, hypertension, orthostatic hypotension, syncope, dementia, urinary incontinence, dyslipidemia, and obesity), frailty predictors, and prior hospital admissions. Concurrent medication use was defined as the number of distinct drug prescriptions filled in the 14 days prior to antihypertensive initiation. As a proxy for sociodemographic status, we identified whether beneficiaries were eligible for the Medicare low-income subsidy (LIS) program. LIS offers medication at a reduced cost for beneficiaries that are eligible due to income, family size, and household resources. We included the frailty index score as a proxy measure of frailty (Faurot et al. 2015). Additionally, we examined the prevalence of factors positively (ambulance transfer, wheelchair/walker use, home oxygen use, hospital bed, difficulty walking, and vertigo) and inversely (cancer screenings) associated with limitations in activities of daily living (Faurot et al. 2015).
Statistical analysis
Descriptive statistics were used to compare baseline covariates according to antihypertensive class initiated on the index date. We estimated propensity scores (PS) using multinomial logistic regression models. PSs estimated the probability of receiving an ACE vs. other classes of antihypertensive drugs adjusting for all baseline covariates. Standardized mortality ratio (SMR) weighting was used to control for confounding due to differences in propensity scores. We weighed beneficiaries of each drug class to achieve the same baseline covariate distribution as beneficiaries receiving an ACE. Therefore, beneficiaries initiating with ACEs were assigned a weight of one and all others were assigned a weight that was the ratio of the PS to one minus the PS (Stürmer et al. 2006). ACEs were used as the referent since they were the most commonly prescribed drug class (Li et al. 2014). To examine the effectiveness of PSs and SMR weights to correctly balance baseline covariates between beneficiaries, we examined the means and proportions of baseline covariates before vs. after SMR weighting. If the PSs are correctly specified, there should be little difference between the mean and proportion of baseline covariates across antihypertenisves classes.
Incident fracture rates and corresponding 95% confidence intervals (CIs) were defined as the total number of incident fractures by the total person-years at risk. Person-years at risk was defined as the total number of days at risk for fractures divided by 365.25. To account for censoring, we used SMR-weighted Cox proportional hazard models to estimate hazard ratios (HRs) and 95% CIs of incident fractures for each drug class initiated on the index date versus receiving an ACE according to days since initiation of therapy, 1–14 days and 15–365 days. We separated time since initiation to distinguish between fractures likely related orthostatis and fractures that may be the result of possible BMD effects. CIs were calculated using robust standard errors to account for SMR weights. We used a ‘first-treatment-carried-forward’ analysis to avoid introducing confounding by indication since antihypertensive adherence varies, and beneficiaries who remain adherent may differ from the majority of hypertensive patients (Hargrove et al. 2017). Using this analysis, beneficiaries contributed person-time at risk until they had an incident fracture or until the end of the follow-up (death, disenrollment from Medicare, or December 31, 2012), whichever came first. SMR weighted Kaplan-Meier curves were used to graph the proportion of beneficiaries without fracture events according to time since initiation. For our secondary analysis when we classified fractures according to probable low vs. normal BMD fractures, if a beneficiary had a fracture event before the event of interest (e.g., normal BMD fracture before a low BMD fracture), beneficiaries were censored at the date of the first fracture event.
Sensitivity analyses
To assess the robustness of our analysis decisions, we performed sensitivity analyses. First, we repeated the analysis using an ‘As-treated’ analysis design. In the ‘As-treated’ analysis, follow-up additionally ended when beneficiaries switched antihypertensive therapy (e.g., switched to another antihypertensive class or started combination therapy), or discontinued use (e.g., failed to fill another prescription 30 days after the end of the last drugs’ days supply). Second, we repeated the analysis extending the first follow-up period to 30 days since the time it takes for blood pressure to stabilize after antihypertensive initiation is not known. Third, we repeated the primary analysis excluding beneficiaries who initiated therapy using a brand antihypertensive medication versus a generic antihypertensive medication. Generic medications are less prone to sample use and are thus less prone to have started antihypertensive therapy before the first dispensed prescription (Hampp et al. 2016). Fourth, since chronic kidney disease and diabetes can impact physicians’ choice of antihypertensive class prescribed, we repeated the analysis removing any beneficiaries with these chronic conditions. Lastly, we repeated the analysis removing beneficiaries prescribed loop diuretics during the baseline period since these medications may be a marker for overall worse health and greater risk of morality (Glynn et al. 2001).
All statistical analyses were conducted using SAS Version 9.4 (Cary, NC).
Results
Between 2008 and 2011, 122,629 Medicare beneficiaries initiated antihypertensive monotherapy. On average beneficiaries were 75 years old, 61% were women, and the majority were White (86%). The most common classes of antihypertensives prescribed were ACEs (33%), BBs (30%), and CCBs (15%). Before SMR weighting, demographics, diabetes, chronic kidney disease, cardiovascular disease (e.g., arrhythmia, stroke, hypertension, and dyslipidemia), ambulance transfers, cancer screenings, and prior hospitalizations differed across beneficiaries according to antihypertensive class. After SMR weighting, there was little difference between baseline characteristics according to antihypertensive class (Table 1).
During the first year after initiation of antihypertensive monotherapy, beneficiaries experienced 4430 incident non-vertebral fractures over 115,991 person-years (rate = 382 per 10,000 person-years, 95%CI: 371–393). Fractures most commonly occurred at the hip (79%), foot (17%), radius (15%), and hand (14%). Just over three-quarters of fractures resulted in a single-bone break (77%).
Rates of incident fracture varied according to antihypertensive class and by time since initiation (Table 2, Additional file 1: Figure S2). During the first 14 days, beneficiaries who initiated with THZs (438 per 10,000 person-years, 95%CI: 294–628) and BBs (410 per 10,000 person-years, 95%CI: 314–526) had the highest rate of fractures. Beneficiaries initiating with CCBs had the highest rate of fractures during the 15–365 days after initiation (435 per 10,000 person-years, 95%CI: 404–468), but a low rate in the first 14 days (383 per 10,000 person-years, 95%CI: 258–550). Initiators of ARBs had the lowest rate of fractures during the initial 14 days (333 per 10,000 person-years, 95%CI: 190–546) and during the 15–365 days after initiation (321 per 10,000 person-years, 95%CI: 287–358).
After controlling for differences in baseline characteristics, beneficiaries who initiated with THZs had the highest rate of fractures in the first 14 days after initiation compared to beneficiaries who initiated with ACEs (SMR-HR: 1.40, 95%CI: 0.78–2.52). After the first 14 days, beneficiaries who initiated with CCBs (SMR-HR: 1.11, 95%CI: 1.00–1.24) and BBs (SMR-HR: 1.09, 95% CI: 1.00–1.19) had slightly higher fractures rates compared to the beneficiaries who initiated with ACEs.
When we stratified results according to fracture location (probable low BMD fractures vs. normal BMD fractures), results were similar for all the antihypertensive classes except THZs (Table 3). During the 1 year following initiation, beneficiaries who initiated with THZs had a lower hazard ratio of probable low BMD fractures (SMR-HR: 0.85, 95%CI: 0.68–1.06), but a slightly higher hazard ratio of normal BMD fractures (SMR-HR: 1.12, 95%CI: 0.98–1.29) compared to beneficiaries who initiated with ACEs.
In sensitivity analyses, results were similar when we 1) used an ‘as-treated’ analysis, 2) excluded beneficiaries with a previous diagnosis of chronic kidney disease or diabetes, and 3) excluded beneficiaries who initiated with brand antihypertensive drugs (Fig. 1, Additional file 1: Table S4). When we extended the initial follow-up period to 30 days, beneficiaries who initiated with THZs (SMR-HR: 1.15, 95%CI: 0.75–1.76) and BBs (SMR-HR: 1.36, 95%CI: 1.01–1.83) still had the highest rate of fractures compared to beneficiaries who initiated with other antihypertensive classes (results not shown).
Discussion
We found incident fracture rates in the year following initiation of antihypertensive therapy differ depending on antihypertensive class, and these patterns were affected by the time since initiation. Medicare beneficiaries who initiated with THZs or BBs had slightly higher fracture rates during the first 2 weeks compared to beneficiaries who initiated with other antihypertensives. However, during the first year beneficiaries who initiated with CCBs had the highest fracture rate. Similar to previous research, we found beneficiaries who initiated with ACEs or ARBs had the lowest rate of fractures (Butt and Harvey 2015; Choi et al. 2015; Wong et al. 2013).
We found older adults initiating with THZs or BBs had the highest fracture rates during the first 2 weeks following initiation. Similar to our results, Berry et al. found that THZ initiators had an increased odds of hip fracture in the first days following initiation compared to periods of no use (Berry et al. 2013). Butt et al. found that the use of any antihypertensive was associated with an increased risk of hip fracture in the first 45 days following initiation, and that this risk was most elevated for older adults initiating with ACEs (Butt et al. 2012). However, Ruths et al. found that only loop diuretics were associated with an initial increased risk of hip fractures during the first 2 weeks of use when comparing the initial fracture risk among antihypertensive class (Ruths et al. 2015). This initial increase in fracture rates may be due to orthostatic hypotension. Among the classes of antihypertensives, THZs are most strongly associated with orthostatic hypotension (Zia et al. 2015). Given that orthostatic hypotension can be asymptomatic (Butt and Harvey 2015; Gupta 2012), results suggest that clinicians and older adults need to be aware of this potential increased risk of fractures when starting antihypertensive therapy, especially when starting therapy with THZs.
Gangavati et al. found that the risk of falls associated with orthostatic hypotension was lower among older adults with controlled hypertension compared to older adults with uncontrolled hypertension (Gangavati et al. 2011). This suggests that increases in fracture rates once hypertension is controlled may be due to other mechanisms besides orthostatic hypotension. One mechanism that may influence the association between antihypertensives and fractures could be antihypertensives interactions with BMD (Berry and Kiel 2014; Ghosh and Majumdar 2014). We found older adults initiating with THZs had a decreased rate of probable low BMD (hip and radius) fractures in the year following initiation. THZs can impact the risk of low BMD fractures by promoting osteoblast activity and reducing calcium urinary excretion (Ghosh and Majumdar 2014; Aung and Htay 2011). A 2011 Cochrane review found that THZs were associated with as much as a 24% reduction in hip fractures when comparing THZ users vs. non-users (Aung and Htay 2011). Results suggest older adults at elevated risk of fractures may potentially benefit from receiving THZs compared to other classes of antihypertensives. However, research featuring clinical BMD measurements is needed to confirm these findings.
Older adults initiating with CCBs had slightly elevated fracture rates compared with ACE initiators. Previous studies have found inconsistent results regarding the association between CCBs and fractures. Ruths et al. found that CCBs were associated with a decreased risk of hip fractures when comparing periods of use and non-use (Ruths et al. 2015). However, this study was limited to hip fractures and results were unadjusted for comorbidities associated with fractures (Ruths et al. 2015). In another study, Choi et al. found that compared to non-users of antihypertensives, adults prescribed CCBs had a slightly elevated rate of non-vertebral fractures (Choi et al. 2015). In our study, beneficiaries who initiated with CCBs were frailer than beneficiaries who initiated with other antihypertensives. Although we included frailty predictors in the propensity scores, we cannot eliminate the possibility that residual confounding remained after adjustment, given that frailty is multi-dimensional and is difficult to capture with claims data alone (Fried et al. 2004).
Despite conducting sensitivity analyses, this study does have limitations. First, results may be subject to residual confounding. We used SMR weights to limit confounding by indication but it is possible that residual confounding remained due to physical activity, visual impairment, baseline BMD, and alcohol use. Some research suggests removing outlier SMR weights to better control for residual confounding. However, we did not exclude outlier SMR weights since excluding these observations resulted in little difference in the results, suggesting that variations in weights were most likely random. Second, fracture effects observed in our study may have been influenced by other factors such as concurrent medication use, other chronic conditions, or previously undiagnosed hypertension. However, results remained the same in sensitivity analyses excluding beneficiaries with diabetes, chronic kidney disease, and those previously taking loop diuretics suggesting that any residual confounding due to side effects from other chronic conditions or medications is minimal. We were unable to distinguish between newly diagnosed hypertension vs. uncontrolled hypertension treated for the first time using claims data. It is possible that beneficiaries were at elevated risk of fracture due to uncontrolled hypertension prior to starting antihypertensive medication. Third, despite controlling for race in propensity scores, it is likely that we were unable to control for all possible race/ethnicity effects due to limitations in the Medicare race/ethnicity data (McBean 2004). Given that the majority of our study population was White, more research is needed featuring more diverse ethnic/racial population to see if the same results would hold true across racial populations. Fourth, our results are limited to the 1 year period following initiation and only included older adults initiating antihypertensives between 2008 and 2011. Antihypertensives impact BMD in as little as 5–8 weeks in animal studies (Birocale et al. 2016; Kang et al. 2013), however less is known about the time it takes for antihypertensives to have clinical BMD effects in humans (Ghosh and Majumdar 2014). One year may not have been long enough to identify all possible BMD affects. Additionally, it is possible that since the time of our study new hypertensive medications have been added to the individual drug classes, however the overall effects of the drug classes would likely remain unchanged. Lastly, our results did not take into account antihypertensive dose. Previous research suggests that the relationship between antihypertensives and fractures is linearly associated with increasing dose (Butt and Harvey 2015; Lipsitz et al. 2015). Results may be underestimated for older adults on higher doses of antihypertensives.
Conclusions
It is important that researchers and clinicians identify modifiable factors that may reduce the risk of fractures among older adults. We found certain classes of antihypertensive medications may impact the rate of fractures in older adults. Specifically, we found slightly increased fracture rates among older adults initiating with THZs and BBs during the first 2 weeks after initiation. Results suggest older adults taking these medications should be aware of this possible increased risk of fractures, particularly in the first few weeks after starting therapy. Also, we found older adults initiating with ACEs and ARBs had slightly lower fracture rates after initiation. However, given that our results may be due to chance variation in effects, more research is needed to verify if these same results hold true across various racial/ethnic populations and across longer periods of follow-up. Results suggest that when deciding upon antihypertensive therapy, clinicians may want to consider possible fracture risks when choosing between antihypertensive drug classes.
Abbreviations
- ACE:
-
Angiotensin-converting enzyme inhibitors
- ARB:
-
Angiotensin-receptor blockers
- BB:
-
Beta blockers
- BMD:
-
Bone mineral density
- CCB:
-
Calcium channel blockers
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- LIS:
-
Low income subsidy
- PS:
-
Propensity score
- SMR:
-
Standardized mortality ratio
- THZ:
-
Thiazide diuretics
References
Annest JL, Fingerhut LA, Gallagher SS, Grossman DC, Hedegaard H, Johnson RL, Trent RB. Strategies to improve external cause-of-injury coding in state-based hospital discharge and emergency department data systems: recommendations of the CDC workgroup for improvement of external cause-of-injury coding. MMWR Recomm Rep. 2008;57(RR-1):1–15.
Aung K, Htay T. Thiazide diuretics and the risk of hip fracture. Cochrane Libr. 2011;(10).
Berry SD, Kiel DP. Treating hypertension in the elderly: should the risk of falls be part of the equation? JAMA Intern Med. 2014;174(4):596–7.
Berry SD, Zhu Y, Choi H, Kiel DP, Zhang Y. Diuretic initiation and the acute risk of hip fracture. Osteoporos Int. 2013;24(2):689–95.
Birocale AM, Medeiros ARS, Ruffoni LDG, Takayama L, de Oliveira JM, Nonaka KO, et al. Bone mineral density is reduced by telmisartan in male spontaneously hypertensive rats. Pharmacol Rep. 2016;68(6):1149–53.
Butt D, Harvey P. Benefits and risks of antihypertensive medications in the elderly. J Intern Med. 2015;278(6):599–626.
Butt DA, Mamdani M, Austin PC, Tu K, Gomes T, Glazier RH. The risk of hip fracture after initiating antihypertensive drugs in the elderly. Arch Intern Med. 2012;172(22):1739–44.
By the American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227–46.
Choi HJ, Park C, Lee Y, Ha Y, Jang S, Shin CS. Risk of fractures in subjects with antihypertensive medications: a nationwide claim study. Int J Cardiol. 2015;184:62–7.
Curtis JR, Mudano AS, Solomon DH, Xi J, Melton ME, Saag KG. Identification and validation of vertebral compression fractures using administrative claims data. Med Care. 2009;47(1):69–72.
DeGrauw X, Annest JL, Stevens JA, Xu L, Coronado V. Unintentional injuries treated in hospital emergency departments among persons aged 65 years and older, United States, 2006–2011. J Saf Res. 2016;56:105–9.
Faurot KR, Jonsson Funk M, Pate V, Brookhart MA, Patrick A, Hanson LC, et al. Using claims data to predict dependency in activities of daily living as a proxy for frailty. Pharmacoepidemiol Drug Saf. 2015;24(1):59–66.
Fraser LA, Adachi JD, Leslie WD, Goltzman D, Josse R, Prior J, et al. Effect of Anticholinergic medications on falls, fracture risk, and bone mineral density over a 10-year period. Ann Pharmacother. 2014;48(8):954–61.
Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: implications for improved targeting and care. J Gerontol A Biol Sci Med Sci. 2004;59(3):255–63.
Gangavati A, Hajjar I, Quach L, Jones RN, Kiely DK, Gagnon P, et al. Hypertension, orthostatic hypotension, and the risk of falls in a community-dwelling elderly population: the maintenance of balance, independent living, intellect, and zest in the elderly of Boston study. J Am Geriatr Soc. 2011;59(3):383–9.
Ghosh M, Majumdar SR. Antihypertensive medications, bone mineral density, and fractures: a review of old cardiac drugs that provides new insights into osteoporosis. Endocrine. 2014;46(3):397–405.
Glynn RJ, Knight EL, Levin R, Avorn J. Paradoxical relations of drug treatment with mortality in older persons. Epidemiology. 2001;12(6):682–9.
Gupta A. Medical management of hip fractures and the role of the orthogeriatrician. Rev Clin Gerontol. 2012;22(4):261–73.
Gupta V, Lipsitz LA. Orthostatic hypotension in the elderly: diagnosis and treatment. Am J Med. 2007;120(10):841–7.
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B, et al. Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med. 2010;152(6):380–90.
Hampp C, Greene P, Pinheiro SP. Use of prescription drug samples in the USA: a descriptive study with considerations for Pharmacoepidemiology. Drug Saf. 2016;39(3):261–70.
Hargrove JL, Pate V, Casteel CH, Golightly YM, Loehr LR, Marshall SW, Stürmer T. Antihypertensive adherence trajectories among older adults in the first year after initiation of therapy. Am J Hypertens. 2017;30(10):1015–23.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth joint National Committee (JNC 8). JAMA. 2014;311(5):507–20.
Johnell O, Kanis J. Epidemiology of osteoporotic fractures. Osteoporos Int. 2005;16(2):S3–7.
Kang KY, Kang Y, Kim M, Kim Y, Yi H, Kim J, et al. The effects of antihypertensive drugs on bone mineral density in ovariectomized mice. J Korean Med Sci. 2013;28(8):1139–44.
Lee RH, Pieper CF, Colón-Emeric C. Functional impairments mediate association between clinical fracture risk and type 2 diabetes mellitus in older women. J Am Geriatr Soc. 2015;63(8):1546–51.
Leibson CL, Tosteson AN, Gabriel SE, Ransom JE, Melton LJ. Mortality, disability, and nursing home use for persons with and without hip fracture: a population-based study. J Am Geriatr Soc. 2002;50(10):1644–50.
Li X, Camelo Castillo W, Stürmer T, Pate V, Gray CL, Simpson RJ, et al. Use of combination antihypertensive therapy initiation in older americans without prevalent cardiovascular disease. J Am Geriatr Soc. 2014;62(9):1729–35.
Lipsitz LA, Habtemariam D, Gagnon M, Iloputaife I, Sorond F, Tchalla AE, et al. Reexamining the effect of antihypertensive medications on falls in old age. Hypertension. 2015;66(1):183–9.
Marks R, Allegrante JP, MacKenzie CR, Lane JM. Hip fractures among the elderly: causes, consequences and control. Ageing Res Rev. 2003;2(1):57–93.
McBean M. Medicare race and ethnicity data. Minneapolis: National Academy of Social Insurance; 2004.
Nurminen J, Puustinen J, Piirtola M, Vahlberg T, Lyles A, Kivela SL. Opioids, antiepileptic and anticholinergic drugs and the risk of fractures in patients 65 years of age and older: a prospective population-based study. Age Ageing. 2013;42(3):318–24.
Pohl P, Nordin E, Lundquist A, Bergström U, Lundin-Olsson L. Community-dwelling older people with an injurious fall are likely to sustain new injurious falls within 5 years-a prospective long-term follow-up study. BMC Geriatr. 2014;14(1):120.
Ray WA, Griffin MR, Fought RL, Adams ML. Identification of fractures from computerized Medicare files. J Clin Epidemiol. 1992;45(7):703–14.
Rejnmark L, Vestergaard P, Mosekilde L. Treatment with beta-blockers, ACE inhibitors, and calcium-channel blockers is associated with a reduced fracture risk: a nationwide case-control study. J Hypertens. 2006;24(3):581–9.
Ruths S, Bakken MS, Ranhoff AH, Hunskaar S, Engesæter LB, Engeland A. Risk of hip fracture among older people using antihypertensive drugs: a nationwide cohort study. BMC Geriatr. 2015;15(1):1.
Solomon DH, Mogun H, Garneau K, Fischer MA. Risk of fractures in older adults using antihypertensive medications. J Bone Miner Res. 2011;26(7):1561–7.
Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and non-fatal falls among older adults. Inj Prev. 2006;12(5):290–5.
Stürmer T, Rothman KJ, Glynn RJ. Insights into different results from different causal contrasts in the presence of effect-measure modification. Pharmacoepidemiol Drug Saf. 2006;15(10):698–709.
Takkouche B, Montes-Martinez A, Gill SS, Etminan M. Psychotropic medications and the risk of fracture: a meta-analysis. Drug Saf. 2007;30(2):171–84.
Tinetti ME, Han L, Lee DS, McAvay GJ, Peduzzi P, Gross CP, et al. Antihypertensive medications and serious fall injuries in a nationally representative sample of older adults. JAMA Intern Med. 2014;174(4):588–95.
Tinetti ME, Williams CS. Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med. 1997;337(18):1279–84.
Wong AK, Lord SR, Sturnieks DL, Delbaere K, Trollor JN, Close JC. Angiotensin system–blocking medications are associated with fewer falls over 12 months in community-dwelling older people. J Am Geriatr Soc. 2013;61(5):776–81.
Woolf AD, Åkesson K. Preventing fractures in elderly people. Br Med J. 2003;327(7406):89–95.
Zang G. Antihypertensive drugs and the risk of fall injuries: a systematic review and meta-analysis. J Int Med Res. 2013;41(5):1408–17.
Zia A, Kamaruzzaman SB, Myint PK, Tan MP. The association of antihypertensives with postural blood pressure and falls among seniors residing in the community: a case–control study. Eur J Clin Investig. 2015;45(10):1069–76.
Funding
The database infrastructure used for this project was funded by the Pharmacoepidemiology Gillings Innovation Lab (PEGIL) for the Population-Based Evaluation of Drug Benefits and Harms in Older US Adults (GIL200811.0010), the Center for Pharmacoepidemiology, Department of Epidemiology, UNC Gillings School of Global Public Health, the CER Strategic Initiative of UNC’s Clinical Translational Science Award (UL1TR001111), the Cecil G. Sheps Center for Health Services Research, UNC, and the UNC School of Medicine.
Availability of data and materials
Data cannot be made available to the public due to data restrictions.
Author information
Authors and Affiliations
Contributions
Study design and concept: YMG, CHC, LRL, TS, SWM, and JLH. Data acquisition and analysis: JLH, VP. Interpretation of the data: YMG, CHC, LRL, TS, SWM, and JLH. Preparation of the manuscript: YMG, CHC, LRL, TS, SWM, and JLH. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Medicare data were obtained under a data use agreement established with the Centers for Medicaid and Medicare Services (CMS) and the University of North Carolina at Chapel Hill (UNC-CH). The study protocol was approved by UNC’s Non-Biomedical Institutional Review Board (# 15-1704).
Consent for publication
Not applicable.
Competing interests
TS receives investigator-initiated research funding and support as Principal Investigator from the National Institute on Aging (NIA), and as Co-Investigator, National Institutes of Health (NIH). He also receives salary support as Director of the Comparative Effectiveness Research (CER) Strategic Initiative, NC TraCS Institute, UNC Clinical and Translational Science Award and as Director of the Center for Pharmacoepidemiology (current members: GlaxoSmithKline, UCB BioSciences, Merck) and research support from pharmaceutical companies (Amgen, AstraZeneca) to the Department of Epidemiology, University of North Carolina at Chapel Hill. Dr. Stürmer does not accept personal compensation of any kind from any pharmaceutical company. He owns stock in Novartis, Roche, BASF, AstraZeneca, and Novo Nordisk.
The authors declare that they have no competing interests.
Additional file
Additional file 1: Table S1.
List of antihypertensive drugs included in study. Table S2. Definitions of fractures identified in Medicare Claims. Table S3. List of chronic conditions and frailty indicators identified using ICD-9 or CPT Codes. Table S4. Sensitivity analysis results examining the rates of incident non-vertebral fractures in the first year after initiation among Medicare beneficiaries initiating antihypertensive monotherapy from 2008 to 2011 according to duration of use. Figure S1. Eligibility criteria for Medicare beneficiaries initiating antihypertensive monotherapy between 2008 and 2011. Figure S2. Weighted Kaplan-Meier curves for incident fractures according duration of use and antihypertensive drug class. (DOCX 134 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hargrove, J.L., Golightly, Y.M., Pate, V. et al. Initiation of antihypertensive monotherapy and incident fractures among Medicare beneficiaries. Inj. Epidemiol. 4, 27 (2017). https://doi.org/10.1186/s40621-017-0125-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40621-017-0125-8