Abstract
Background
Consumption of baked egg by raw egg allergic children is associated with immune changes suggesting development of tolerance. However, causation has not been tested using a double blind randomized controlled trial (RCT). We aimed to compare clinical and immunological outcomes after baked egg (BE) consumption in young BE tolerant egg allergic children.
Methods
In a double blind RCT, BE tolerant egg allergic children consumed 10 g BE (1.3 g protein) 2 to 3 times per week for 6 months (n = 21 intervention group) or similar egg free baked goods (n = 22 control group) while maintaining an otherwise egg free diet. The final assessment was a raw egg oral food challenge (OFC) 1 month after ceasing the intervention product. Egg specific IgE and IgG4 were assessed at baseline and 7 months.
Results
After the intervention there was no difference in raw egg tolerance between groups, (23.5% (4/17) intervention group and 33.3% (6/18) control group). This was independent of age and amount of BE consumed (aOR 0.50 CI 0.11–2.40 p = 0.39). Both groups demonstrated decreased egg specific serum IgE titres and decreased whole egg specific IgE/IgG4 ratios.
Discussion
We conducted this trial because inclusion of baked egg protein in the diet of egg allergic children appears to move children towards a more tolerant immune profile. Strengths of our study include design of the blinded intervention, the consistent dosing protocol and the regular monitoring of symptoms and intake. However, the study was limited by small sample size resulting in insufficient power to show statistically significant results.
Conclusion
Our study suggests that short term, regular consumption of BE by BE tolerant 1 to 5 year old children with IgE mediated raw egg allergy may not induce, accelerate or slow development of tolerance to raw egg in this selected population. Trials with larger sample sizes are required to further test this hypothesis.
Trial Registration
The trial was registered on 7th February 2012 with the Australian New Zealand Clinical Trials Registry (ACTRN 12612000173897).
Similar content being viewed by others
Background
Many egg allergic children tolerate baked egg (BE) before less well-cooked forms of egg as heating causes structural changes in some egg epitopes and there is a matrix effect when egg is baked with wheat that may also be important [1,2,3,4]. Inclusion of BE in the diet of egg allergic children, when tolerated, has become accepted clinical practice [5,6,7,8] and it is reported that individuals consuming BE tolerate lightly cooked egg earlier than those not consuming BE [9, 10]. Regular consumption of BE is associated with increases in specific IgG4, and decreases in specific IgE [1, 11], immunological changes similar to those observed during specific oral tolerance induction (SOTI) [12]. From this it was hypothesised consumption of BE could promote tolerance to uncooked egg protein [13].
It remains unclear, in children with raw egg allergy tolerant to BE if ingestion of BE accelerates tolerance acquisition to raw egg as randomised controlled clinical trials (RCT) have not been undertaken. It is also not clear from observational studies whether BE tolerant children who gain raw egg tolerance earlier than those not tolerant to BE were moving towards natural resolution of their egg allergy, or if this was due to changes with time or other unidentified confounders [1, 11].
Our study’s primary aim was to determine whether raw egg allergy is better resolved by regular consumption of BE (intervention group) compared with an egg free diet (control group). We also examined the effect of regular BE exposure on immunity, particularly patterns of evolving allergen-specific responses.
Methods
Study design
Six month old to five year old children with IgE mediated egg allergy following egg free diets were recruited from the Women’s and Children’s Hospital Allergy Clinic. Following recruitment all children had egg allergen SPT (see Appendix 1). Egg allergy was defined as children with a convincing clinical reaction to egg within the past 12 months and evidence of current sensitisation on the basis of positive SPT to egg white or evidence of current sensitisation consistent with a >95% likelihood of clinical reactivity (SPT to egg white ≥ 5 mm if aged under 2yo, or ≥ 8 mm in children aged 2 to 5yo) [14, 15]. To assess BE tolerance, all children had an open, medically supervised BE oral food challenge (OFC) (10 g of egg in a muffin) [16]. BE tolerant children with EW SPT <5 mm (6 months to 2yo) or <8 mm (2 to 5yo), who reported no clinical reactions to raw egg in the previous 12 months had an open pasteurised raw egg OFC [17] to confirm they still had a raw egg allergy.
The study was conducted using a double-blind, randomised, placebo controlled trial design. Baseline characteristics including demographics, allergy history and anthropometrics (weight and length or height) were gathered. For those children with eczema the clinical severity was scored using the SCORAD assessment [18]. A peripheral blood sample was collected to measure baseline whole egg (WE), egg white (EW), ovalbumin (OVA) and ovomucoid (OVM) specific IgE (sIgE), WE specific IgG4 (sIgG4) and functional cell response profiles. Written informed consent was obtained before trial participation. Approval was granted by the local institutional review board (Human Research Ethics Committee; REC2400/9/14) of the Women’s and Children’s Health Network Adelaide, Australia, and the trial registered with the Australian New Zealand Clinical Trials Registry (ACTRN 12612000173897).
Randomisation and concealment allocation
Each child was randomly assigned to the intervention group or the control group using a computerised randomisation schedule stratified by age (6 months to 2.5 years and 2.6 years to 5 years). A research assistant (with no involvement in the outcome assessments) was responsible for baking and coding the dietary products for the trial.
Dietary intervention
The study compared the effects of inclusion of baked egg containing (intervention group) or egg free (control group) products in the diet of raw egg allergic children for 6 months after randomisation. Both groups maintained an otherwise egg free diet with study muffins, biscuits (cookies) or cake offered to the child for consumption 2 to 3 times per week for 6 months. The intervention group consumed 10 g BE (1.3 g egg protein) per serve. The control group consumed egg free products tested for similarity in terms of appearance, taste, and texture. Intervention products were offered 2 to 3 times a week (consistent with the Australian Dietary Guidelines for inclusion of ‘discretionary foods’ in a child’s diet [19]).
To assess compliance with the intervention, care givers maintained an intake and symptom diary, participants were reviewed 1 month after randomisation and telephoned monthly for the study duration.
After 6 months the intervention was stopped and children continued an egg free diet for an additional month, to differentiate between desensitisation and development of sustained unresponsiveness to egg [20].
Adverse events were defined as flares in eczema, urticaria, angioedema or vomiting associated with intake of the intervention product or hospitalisation for any reason greater than 24 h. Serious adverse events (defined as any death, admission to intensive care, or anaphylactic reaction) were reported to the institutional review board.
Outcome assessments
The primary outcome was raw egg allergy 1 month after the intervention ended, assessed by an open medically supervised, graded pasteurised raw whole egg OFC [17, 21]. A positive reaction to an OFC was defined by symptoms within 2 hours of the OFC according to the PRACTALL Guidelines [22, 23]. SPT to EW was performed prior to the OFC.
Analysis of immune outcomes
To assess sensitisation egg allergen (WE, EW, OVA and OVM) sIgE levels were measured. WE sIgG4 was used as a marker of tolerance. The sIgE and sIgG4 were analysed at the end of the trial (maintaining blinding of the sample ID). T cell surface markers and Th1/Th2 cytokines were also analysed (see Appendix 2).
Statistical analysis
A sample size estimate was calculated based on the known natural history of egg allergy expecting after 6 months of management with an egg free diet 90% of children would still be egg allergic [2]. We hypothesized regular exposure to BE would result in 30% absolute reduction (ie from 90 to 60%) of egg allergy. To detect such a difference with 90% power and p = 0.05, we estimated we would need 49 children per group (total n = 98) and aimed to recruit 55 children to each group to allow for withdrawals from the study. However, after screening 83 children for BE tolerance over 20 months, and enrolling 43 participants, screening for the study ceased due to resource constraints.
Analyses were performed according to the randomized group using STATA 13.1 (StataCorp LP) or the InStat program v 6.05 (Graph Pad software, USA). Statistical significance was assessed at the 0.05 level. The proportion of children tolerant to egg at the study’s end was compared between groups. Secondary comparisons between groups included changes in sIgE and sIgG4 results and other immune outcomes. For sIgE and sIgG4 results, standard linear regression was performed including the baseline level as a covariate to ensure estimated differences between groups were not biased due to differences in baseline wheal size and/or regression to the mean effects. For ‘adjusted’ analyses, age stratum was also included. In all cases, sensitivity analyses (removal of outlying/influential observations) were undertaken, and did not affect the conclusions. Change between groups was assessed using the Wilcoxon Rank-Sum Test.
For other immune outcomes a non-parametric approach was used for analysis because of highly skewed distributions of all variables and small sample sizes.
Results
Randomization occurred from 22 May 2012 to 20 January 2014. The final follow up appointment was completed on 8 October 2014. While we intended to screen from 6 months of age many babies could not tolerate the texture of baked egg, so screening challenges were scheduled from 1 year of age. The outcomes of the screening BE OFCs are in Appendix 3.
We randomised 43 children (n = 21 intervention group; n = 22 control group), aged 1.0 to 5.3 years. Both groups had similar family and clinical backgrounds (Table 1). Four parents withdrew consent and 38 children (19 from each group) attended primary outcome assessments (Fig. 1).
Clinical outcomes
Tolerance to raw egg after the intervention
Thirty-five children had raw egg OFCs (n = 17 intervention group; n = 18 control group), (Fig. 1). 23% (4/17) children from the intervention group and 33% (6/18) control group passed the raw egg OFC and were therefore egg tolerant. There was no difference between groups in likelihood of tolerating raw egg (Odds Ratio [OR], 0.62; 95% CI, 0.14–2.73; p = 0.52), even after age adjustment (OR 0.50; CI, 0.11–2.40; p = 0.39).
Per protocol analysis comparing children consuming 2 to 3 serves per week of study product 42% (4/19, intervention group), 68% (13/19, control group) demonstrated no difference between groups in the proportion passing the raw egg OFC (OR, 1.2; CI, 0.185–7.77; p = 0.85). Adjusted analysis was not performed because of small numbers.
There were three protocol deviations due to clinical decisions not to proceed with the end of study raw egg OFC. Two children who had refused to eat the study product had high EW SPT values (intervention group n = 1, 12.5 mm wheal; control group n = 1, 24.5 mm wheal) and instead of raw egg OFCs had BE OFCs (passed). It is not known if these children would have passed the raw egg OFC if given. One child (intervention group) did not have a raw egg OFC due to an accidental reaction to semi-cooked egg the week prior to the appointment, and would have reacted to the raw egg OFC. Inclusion of this child in the analysis would not change the final outcome of the trial.
Compliance with the intervention
Participants were offered 2324 serves of intervention product during the study. Intervention group children were offered fewer (1065) serves, consuming a median of 1.6 (IQR 0.7–2.6) serves per week, compared with the control group offered 1259 serves, consuming 2.3 (IQR 1.4–2.7) serves per week. The differences between groups were not significant.
Compliance with the egg free diet
One child (intervention group) had several accidental exposures to egg during the course of the study. This child did not have the end of study raw egg OFC due to a recent reaction to semi-cooked egg. No other accidental exposures to egg were reported by participants in the study.
Adverse events
Nine children in the intervention group and eight children in the control group reported adverse events (Table 2). One child (control, egg free group) was diagnosed with Eosinophilic Oesophagitis during the study. Three serious adverse events were reported (anaphylaxis treated with adrenaline during the raw egg OFC [n = 2 intervention group; n = 1 control group]).
Immunological outcomes
Egg allergen specific IgE results
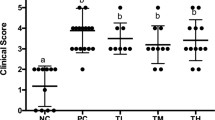
Egg allergen sIgE levels did not differ between intervention groups from baseline to end of the intervention when compared using linear regression analysis for effect of group allocation on outcome, adjusted for age stratum. For both groups we observed significant reductions with time in median specific IgE levels (kUA/L) to WE, (BE group 3.33 (0.75–11.62) to 2.20 (0.47–8.01), p = 0.04; control group 1.71 (0.19–6.94) to 1.26 (0.19–6.01), p = 0.01), EW (BE group 3.72 (0.82–11.62) to 1.61 (0.42–8.17), p = 0.04; control group 1.95 (0.28–11.60) to 1.66 (0.14–8.55), p < 0.01) and OVA sIgE (BE group 2.57 (0.64–7.40) to 1.23 (0.29–5.23), p = 0.01; control group 1.48 (0.33–5.29) to 0.75 (0.15–4.05), p < 0.01) (Fig. 2).
Whole egg serum specific IgG4 and IgE to IgG4 ratio results
There was no significant difference in WE sIgG4 levels within the intervention and control groups or between the groups from baseline to end of the intervention. [BE group (0.16 (0.02-1.5) to 0.64 (0.10-1.88), p = 0.3); control group (0.16 (0.01–0.79) to 0.27 (0.09–0.99), p = 0.3)] (Fig. 3).
No difference in median WE specific IgE/IgG4 ratio was observed between groups during the intervention. However, a significant decrease in the median WE IgE/IgG4 ratio (indicative of evolving tolerance to egg) was observed with time in both BE intervention (15.63 (3.51–35.00) to 2.91 (0.88–9.21), p = 0.02) and control groups (17.50 (3.86–50.18) to 8.28 (0.74–14.13), p = 0.04) (Fig. 4).
Cellular immune analysis
We assessed Th1/Th2 cytokines and T cell phenotypes, with no significant difference observed between groups (data not shown).
Discussion
This double blind, placebo controlled RCT compares the effect of consumption of BE (with avoidance of all other forms of egg) in 1 to 5 year old BE tolerant, raw egg allergic children on the development of tolerance to raw egg. In our study group, development of tolerance to raw egg was independent of consumption of BE. We conducted this trial because inclusion of baked egg protein in the diet of egg allergic children appears to move children towards a more tolerant immune profile [13]. In addition inclusion of baked proteins in the diet, when tolerated, improves quality of life.
Strengths of our study include design of the blinded intervention, the consistent dosing protocol and the regular monitoring of symptoms and intake. Randomized groups were of similar age, allergy background and egg allergy phenotype, and the timing of assessments for clinical and immunological outcomes add additional strength to our results. We acknowledge that the small sample size is a major limitation because of the resulting insufficient power to show statistically significant results. Over 200 families of egg allergic children were approached regarding the trial, and of the children screened for the trial, only half tolerated BE, which was less than expected [1, 24]. There are several potential explanations for the lack of difference between the two trial arms:
-
Small sample size, and thus the lack of difference may be due to chance. Whilst our study was underpowered, we did not see trends suggesting any effects on either clinical or immunological outcomes.
-
The time period of the intervention may have been too short. However, decreased SPT wheal sizes and egg sIgE, and increased sIgG4 have been reported after 3 to 6 months exposure to BE [1, 11], leading to conjecture that inclusion of BE, when tolerated, in the diets of egg allergic children may modulate the immune system [8, 13, 25, 26]. In our group of BE tolerant children, there was no difference between groups in reduction in egg allergen sIgE levels or increase in WE sIgG4 levels. Our results are consistent with Tey et al. [27], who reported no difference in the rate of decline in EW SPT wheal size in 3 to 6 year old egg allergic children consuming BE compared with an egg free diet indicating that this change may be independent of consumption of BE.
-
The dose of BE may have been too low, or too infrequent. To comply with Australian healthy eating guidelines related to consumption of ‘discretionary foods’ [19] we asked the children to consume the study foods 2 or 3 times per week. This dose rate is consistent with the maintenance phase of several egg SOTI studies [28,29,30], but less frequent than Lemon-Mule et al. [1] who dosed 1 to 3 times daily. In our study, three children (6%) (n = 2 intervention group; n = 1 control group), refused to consume intervention products possibly due to finicky eating, or related to the texture of the study products. Poor compliance has also been reported in other immunotherapy trials [31, 32], including other BE trials [33], and also was recently reported in the EAT study[34]. It is possible that some children in our study may have lost tolerance to BE, reflected by refusal to consume the study product. Development of symptoms when consuming BE and subsequent refusal to consume BE has been reported in children passing BE OFCs [16]. Participants in our study kept an intake and symptom diary (including signs of abdominal pain and other non IgE mediated allergies). Abdominal pain was only reported by one child in the BE group. Adjusting for total consumption of BE in our final analysis made no difference to the outcome.
-
As was common practise when we designed this trial, to test for sustained unresponsiveness, participants in the trial had a 4-week break from BE prior to the end of study PE challenge. This may have affected the outcome of the trial compared with an OFC at the end of the 6 month period of BE ingestion.
-
Ingestion of BE does not alter the resolution of raw egg allergy (i.e. the study finding of no effect is true). A population based study of 2 year-old BE tolerant, egg allergic children demonstrated frequent ingestion of BE was associated with earlier resolution of egg allergy [24]. Once BE intolerant children developed BE tolerance they were as likely to gain tolerance to regular egg as children initially tolerant to BE [24]. This may reflect a phenotype outgrowing their egg allergy more quickly than those self-limiting their BE intake.
There are no reports of controlled studies considering the effects of BE in the diets of older cohorts of egg allergic children, and such studies are warranted as BE may modulate the immune system in children with more resistant phenotypes of egg allergy.
Conclusion
Our study suggests that short term, regular consumption of BE by BE tolerant 1 to 5 year old children with IgE mediated raw egg allergy may not induce, accelerate or slow development of tolerance to raw egg in this selected population. Trials with larger sample sizes are required to further test this hypothesis.
Abbreviations
- BE:
-
Baked egg
- EW:
-
Egg white
- EY:
-
Egg yolk
- Ig:
-
Immunoglobulin
- OFC:
-
Oral food challenge
- OVA:
-
Ovalbumin
- OVM:
-
Ovomucoid
- SOTI:
-
Specific oral tolerance induction
- SPT:
-
Skin prick test
- WE:
-
Whole egg
References
Lemon-Mulé H, Sampson HA, Sicherer SH, Shreffler WG, Noone S, Nowak-Wegrzyn A. Immunologic changes in children with egg allergy ingesting extensively heated egg. J Allergy Clin Immunol. 2008;122:977–83. e971.
Clark A, Islam S, King Y, Deighton J, Szun S, Anagnostou K, Ewan P. A longitudinal study of resolution of allergy to well-cooked and uncooked egg. Clin Exp Allergy. 2011;41:706–12.
Alessandri C, Zennaro D, Zaffiro A, Mari A. Molecular allergology approach to allergic diseases in the paediatric age. Ital J Pediatr. 2009;35:29.
Martos G, Lopez-Exposito I, Bencharitiwong R, Berin MC. Mechanisms underlying differential food allergy response to heated egg. J Allergy Clin Immunol. 2011;127:990–7.
Clark AT, Skypala I, Leech SC, Ewan PW, Dugué P, Brathwaite N, Huber PAJ, Nasser SM, Immunology BsfAaC. British Society for Allergy and Clinical Immunology guidelines for the management of egg allergy. Clin Exp Allergy. 2010;40:1116–29.
American College of Allergy A, Immunology. Food allergy: a practice parameter. Ann Allergy Asthma Immunol. 2006;96:S1–S68.
Allen CW, Campbell DE, Kemp AS. Food allergy: Is strict avoidance the only answer? Pediatr Allergy Immunol. 2008;20:415–22.
Konstantinou GN, Kim JS. Paradigm shift in the management of milk and egg allergy: baked milk and egg diet. Immunol Allergy Clin North Am. 2012;32:151–64.
Caubet JC, Bencharitiwong R, Moshier E, Godbold JH, Sampson HA, Nowak-Wegrzyn A. Significance of ovomucoid- and ovalbumin-specific IgE/IgG(4) ratios in egg allergy. J Allergy Clin Immunol. 2012;129:739–47.
Leonard SA, Martos G, Wang W, Nowak-Wegrzyn A, Berin MC. Oral immunotherapy induces local protective mechanisms in the gastrointestinal mucosa. J Allergy Clin Immunol. 2012;129:1579–87. e1571.
Konstantinou GN, Giavi S, Kalobatsou A, Vassilopoulou E, Douladiris N, Saxoni-Papageorgiou P, Papadopoulos NG. Consumption of heat-treated egg by children allergic or sensitized to egg can affect the natural course of egg allergy: hypothesis-generating observations. J Allergy Clin Immunol. 2008;122:2008. JACI2414-2005.
Wisniewski J, Agrawal R, Woodfolk JA. Mechanisms of tolerance induction in allergic disease: integrating current and emerging concepts. Clin Exp Allergy. 2013;43:164–76.
Netting M, Makrides M, Gold M, Quinn P, Penttila I. Heated allergens and induction of tolerance in food allergic children. Nutrients. 2013;5:2028–46.
Sporik R, Hill DJ, Hosking CS. Specificity of allergen skin testing in predicting positive open food challenges to milk, egg and peanut in children. Clin Exp Allergy. 2000;30:1540–6.
Turner PJ, Mehr S, Joshi P, Tan J, Wong M, Kakakios A, Campbell DE. Safety of food challenges to extensively heated egg in egg-allergic children: a prospective cohort study. Pediatr Allergy Immunol. 2013;24:450–5.
Lee E, Mehr S, Turner PJ, Joshi P, Campbell DE. Adherence to extensively heated egg and cow’s milk after successful oral food challenge. J Allergy Clin Immunol Pract. 2015;3:125–7. e124.
Palmer DJ, Metcalfe J, Makrides M, Gold MS, Quinn P, West CE, Loh R, Prescott SL. Early regular egg exposure in infants with eczema: A randomized controlled trial. J Allergy Clin Immunol. 2013;132:387–92. e381.
Kunz B, Oranje AP, Labreze L, Stalder JF, Ring J, Taieb A. Clinical validation and guidelines for the SCORAD index: consensus report of the European Task Force on Atopic Dermatitis. Dermatology. 1997;195:10–9.
National Health and Medical Research Council. Australian Dietary Guidelines. Canberra: NHMRC; 2013.
Moran TP, Vickery BP, Burks AW. Oral and sublingual immunotherapy for food allergy: current progress and future directions. Curr Opin Immunol. 2013;25:781–7.
Netting M, Donato A, Makrides M, Gold M, Quinn P, Penttila I. Allergenicity of pasteurized whole raw Hen’s egg compared with fresh whole raw Hen’s egg. Pediatr Allergy Immunol. 2015;26:234–8.
Sampson HA, Gerth van Wijk R, Bindslev-Jensen C, Sicherer S, Teuber SS, Burks AW, Dubois AE, Beyer K, Eigenmann PA, Spergel JM, et al. Standardizing double-blind, placebo-controlled oral food challenges: American Academy of Allergy, Asthma & Immunology-European Academy of Allergy and Clinical Immunology PRACTALL consensus report. J Allergy Clin Immunol. 2012;130:1260–74.
Nowak-Wegrzyn A, Assa’ad AH, Bahna SL, Bock SA, Sicherer SH, Teuber SS, on behalf of the Adverse Reactions to Food Committee of the American Academy of Allergy, Asthma and Immunology. Work Group report: oral food challenge testing. J Allergy Clin Immunol. 2009;123:S365–83.
Peters RL, Dharmage SC, Gurrin LC, Koplin JJ, Ponsonby AL, Lowe AJ, Tang ML, Tey D, Robinson M, Hill D, et al. The natural history and clinical predictors of egg allergy in the first 2 years of life: a prospective, population-based cohort study. J Allergy Clin Immunol. 2014;133:485–91.
Huang F, Nowak-Wegrzyn A. Extensively heated milk and egg as oral immunotherapy. Curr Opin Allergy Clin Immunol. 2012;12:283–92.
Leonard SA, Caubet JC, Kim JS, Groetch M, Nowak-Wegrzyn A. Baked milk- and egg-containing diet in the management of milk and egg allergy. J Allergy Clin Immunol Pract. 2015;3:13–23. quiz 24.
Tey D, Dharmage SC, Robinson MN, Allen KJ, Gurrin LC, Tang ML. Frequent baked egg ingestion was not associated with change in rate of decline in egg skin prick test in children with challenge confirmed egg allergy. Clin Exp Allergy. 2012;42:1782–90.
Meglio P, Giampietro PG, Carello R, Gabriele I, Avitabile S, Galli E. Oral food desensitization in children with IgE-mediated hen’s egg allergy: a new protocol with raw hen’s egg. Pediatr Allergy Immunol. 2013;24:75–83.
Patriarca G, Nucera E, Pollastrini E, Roncallo C, De Pasquale T, Lombardo C, Pedone C, Gasbarrini G, Buonomo A, Schiavino D. Oral specific desensitization in food-allergic children. Dig Dis Sci. 2007;52:1662–72.
Itoh N, Itagaki Y, Kurihara K. Rush specific oral tolerance induction in school-age children with severe egg allergy: one year follow up. Allergol Int. 2010;59:43–51.
Sanchez-Garcia S, Rodriguez del Rio P, Escudero C, Garcia-Fernandez C, Ramirez A, Ibanez MD. Efficacy of oral immunotherapy protocol for specific oral tolerance induction in children with cow’s milk allergy. Isr Med Assoc J. 2012;14:43–7.
Bender BG, Oppenheimer J. The special challenge of nonadherence with sublingual immunotherapy. J Allergy Clin Immunol Pract. 2014;2:152–5.
Saifi M, Clark A, Arneson A, Feldman M, Bird JA. Baked egg oral immunotherapy (OIT) for baked egg (BE) allergic children. J Allergy Clin Immunol. 2015;135:AB26.
Perkin MR, Logan K, Tseng A, Raji B, Ayis S, Peacock J, Brough H, Marrs T, Radulovic S, Craven J, et al. Randomized Trial of Introduction of Allergenic Foods in Breast-Fed Infants. N Engl J Med. 2016;374:1733–43.
ASCIA Skin Prick Testing for the diagnosis of allergic disease. A manual for practitioners [https://www.allergy.org.au/health-professionals/papers/skin-prick-testing]. Accessed 6 Feb 2013.
Acknowledgements
We thank the families who participated and the following research staff who supported the study: Daniella Calderisi, Heather Garreffa, Luiza Duszynski, Wendy Hackett, Irene Kanter, Anna Strachan, Sue Hewitt and Dr Karen Best. We also thank Dr Jennie Louise (Data Management and Analysis Centre, the University of Adelaide) for the statistical analysis.
Funding
The study was supported by grant funding from the Women’s and Children’s Hospital Foundation, The Ilhan Food Allergy Foundation and the Australian Egg Corporation Limited. The Link Group/Stallergenes donated the skin prick test reagents and the IgE/IgG4 analysis was supported by Phadia. The funding bodies had no role in the design of the study, interpretation of the data or in writing the manuscript. MN was supported by a MS McLeod Research Trust PhD scholarship, and a Centre for Food and Allergy Research NHMRC CRE top up scholarship. MM is an NHMRC Principal Research Fellow.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to privacy reasons but are available from the corresponding author on reasonable request.
Authors’ contributions
MN conceived, designed and conducted the study including acquisition of data, analysis and interpretation of data. MN also prepared first draft of the manuscript and subsequent revisions. MG and PQ contributed to the study design and were responsible for clinical supervision of the trial and interpretation of clinical results. AE-M provided technical advice regarding study design, and contributed to interpretation of results. IP contributed to the conception and design of the study and supervised the immunological investigations and interpretation of immunological results. MM supervised the conception and design of the study, and was responsible for overall supervision of the trial and interpretation of results. All authors critically reviewed and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Approval was granted by the Human Research Ethics Committee of the Women’s and Children’s Health Network Adelaide, Australia (REC2400/9/14).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Appendices
Appendix 1: Methods
Skin prick testing
To assess sensitisation to egg allergens, the children were skin prick tested to the common egg allergens, according to standard methods [35]. The allergen extracts used were egg white (Alyostal # 143, AUST R32582)(1:20 w/v), egg yolk (Alyostal # 144, AUST R32582)(1:20 w/v), (The Link Group/Stallergenes, Suburb, NSW), whole egg (ALK-Abello USA) (1:100 w/v), ovalbumin (ALK–Abello Spain; Allergen # 6.22)(1:20 w/v), and ovomucoid (ALK-Abello Spain; Allergen # 6.23)(1:20 w/v), (Australasian Medical and Scientific Ltd, Suburb, NSW). The negative control used was 50% (w/v) glycerin/saline (Holister-Steir Laboratories, Spokane, WA, USA) and the positive control was histamine phosphate (10 mg/ml, B 0911308) supplied by The Department of Pharmacy, Royal Adelaide Hospital, Adelaide, South Australia. A positive skin prick test to an allergen was defined as a mean of two perpendicular wheal diameters of 3 mm or greater in size than the mean wheal of the negative control site at 15 min.
Measurement of antigen specific ige
Serum whole egg, egg white, ovalbumin and ovomucoid specific IgE and whole egg specific IgG4 concentrations in plasma were measured using the Phadia CAP system by the Department of Immunopathology, SA Pathology at the Women’s and Children’s Hospital, using NATA accredited methodologies as per SA Pathology protocols.
Appendix 2 Immunological methodology
Immune memory development was assessed by CD45RA/CD45RO, and staining with CCR7 allowed assessment of changes in effector and central memory to be detected. To further assess immune activation peripheral blood mononuclear cells (PBMCs) sampled at baseline and the end of the intervention were incubated with OVA or OVM and assessed for T cell CD69 expression and cytokine excretion from the PBMCs was also measured to assess changes in the Th1/Th2 balance.
Peripheral blood samples were collected at the screening and 7 month visits and processed immediately. Plasma was collected after centrifugation and stored at −80C for determination of serum specific IgE/IgG4 levels. Peripheral blood mononuclear cells (PBMCs) were isolated by Ficoll-Hypaque (Alexis-Shield, Oslo, Norway) gradient centrifugation and isolated cells cryopreserved in 80% heat inactivated FCS (Sigma-Aldrich, Sydney, Australia) and 20% dimethyl sulfoxide (Ajax Finechem, Taren Point, NSW, Australia). Cell number and viability was assessed by Trypan Blue.
For the cell culture experiments, PBMCs (106 cells/ml) were cultured with 100 μg/ml egg allergens OVA and OVM (Sigma-Aldrich, Sydney, Australia) for 5 days at 37 °C and 5% CO2. Cells cultured with AIM-V medium (Invitrogen, Life Technologies Sydney, Australia) alone served as a no-antigen control, and phytohemagglutinin-L (PHA-L) (1 ug/ml) (Roche Diagnostics, Australia or Remel, KS, USA) was used as the positive control. At day 3 (for PHA-L stimulated cells) and day 5 (for OVA, OVM and no antigen control) all available cells were harvested and analysed. Cells were centrifuged at 300xg for 5 min and the resulting supernatants collected and stored at −80 °C for cytokine analysis. The cell pellet was then equally divided into FACS tubes for labelling with mouse anti human conjugated monoclonal antibodies specific for cell surface antigens. Combinations of fluorophores PE, PE-Cy7, FITC, APC, APC-Cy7 or PerCP were used to assess the phenotype of the cells. All antibodies (except CCR7) were purchased from BD Biosciences (San Jose, CA, USA). CCR7 was purchased from (Miltenyi Biotec, Auburn, SD, USA). Cells were acquired on a BD Biosciences FACS Canto flow cytometer (Becton Dickinson, CA, USA). Isotype controls were used to set up the instrument and the positive gating, and these settings were maintained throughout. After selecting a lymphocyte gate based on forward and side-scatter characteristics, events within the lymphocyte gate were analysed using BD FacsDiva™ software version 6.1.3 (BD Biosciences, San Jose, CA, USA).
For the immunophenotyping cells were stained at baseline for CD4, CD8, CD14, CD19 and HLA DR. To assess activation, cells were stained with CD69 at baseline and after incubation with OVA and OVM and to assess memory markers cells were stained with CD45RO, CCR7, CD27 and CD28.
The cytokine concentration in supernatants collected on days 3 and 5 after incubation with OVA or OVM was assessed using a BD Cytometric Bead Array Human Inflammatory Cytokine Kit (IL-8, Il-1, IL-6, TNF, IL-12 and IL-10) and individual cytokines IL-4, IL-5 and IFNγ were measured using the BD Biosciences enhanced sensitivity flex sets for Human IL-4, Human IL-5 and Human IFNγ and a BD Cytometric Bead Array (CBA) Human enhanced Sensitivity Master Buffer Kit (BD Biosciences, San Jose, CA, USA). (Minimum levels of detection: IL-8, 2.6 pg/ml; IL-1, 7.2 pg/ml; IL-6 2.5 pg/ml; IL-10 3.3 pg/ml; TNF, 3.7 pg/ml; IL-12, 1.9 pg/ml). Beads were acquired on a BD Biosciences FACS Canto flow cytometer (Becton Dickinson, San Jose, CA, USA) and analysed using BD FacsDivaTM software version 6.1.3 (BD Biosciences, San Jose, CA, USA).
Appendix 3: Results of screening baked egg oral food challenges
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Netting, M., Gold, M., Quinn, P. et al. Randomised controlled trial of a baked egg intervention in young children allergic to raw egg but not baked egg. World Allergy Organ J 10, 22 (2017). https://doi.org/10.1186/s40413-017-0152-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40413-017-0152-5