Abstract
Background
Epilepsy, a serious chronic neurological condition effecting up to 100 million people globally, has clear genetic underpinnings including common and rare variants. In Saudi Arabia, the prevalence of epilepsy is high and caused mainly by perinatal and genetic factors. No whole-exome sequencing (WES) studies have been performed to date in Saudi Arabian epilepsy cohorts. This offers a unique opportunity for the discovery of rare genetic variants impacting this disease as there is a high rate of consanguinity among large tribal pedigrees.
Results
We performed WES on 144 individuals diagnosed with epilepsy, to interrogate known epilepsy-related genes for known and functional novel variants. We also used an American College of Medical Genetics (ACMG) guideline-based variant prioritization approach in an attempt to discover putative causative variants. We identified 32 potentially causative pathogenic variants across 30 different genes in 44/144 (30%) of these Saudi epilepsy individuals. We also identified 232 variants of unknown significance (VUS) across 101 different genes in 133/144 (92%) subjects. Strong enrichment of variants of likely pathogenicity was observed in previously described epilepsy-associated loci, and a number of putative pathogenic variants in novel loci are also observed.
Conclusion
Several putative pathogenic variants in known epilepsy-related loci were identified for the first time in our population, in addition to several potential new loci which may be prioritized for further investigation.
Similar content being viewed by others
Background
Epilepsy is a group of chronic neurological diseases characterized by unprovoked seizures due to abnormal neuronal firing in the brain. It is one of the most frequently encountered medical problems in neurology clinics. Epilepsy affects up to 1 in 26 individuals in the USA and approximately 5–7 per 1000 individuals worldwide with reports indicating that at least 50 to 100 million people in the world suffer from this disease, with approximately 85% of these cases living in developing countries [1,2,3]. However, 20–30% of all epilepsy cases are due to acquired factors, such as infection, stroke, trauma, neoplasms, and autoimmunity, while the remaining cases are thought to be due to genetic factors [4]. Epidemiological studies have observed an increased risk of epilepsy development in the relatives of epileptic individuals [5].
Genome-wide association studies (GWAS) of epilepsy phenotypes using genome-wide genotyping (GWG) arrays have discovered many single-nucleotide polymorphisms (SNPs) associated with the disease. A meta-analysis conducted by the International League Against Epilepsy in 2014 identified SNPs associated with the development of epilepsy in the sodium voltage-gated channel alpha subunit 1 (SCN1A), Protocadherin 7 (PCDH7), FA Complementation Group L (FANCL) and Vaccinia Related Kinase 2 (VRK2) genes [6]. A subsequent large GWAS encompassing over 15,200 epilepsy subjects and 29,600 controls revealed 16 genome-wide significant signals reaching statistical significance. Genes in these loci have diverse roles in histone modification, ion-channels, pyridoxine metabolism, synaptic transmission as well as transcription factors. Interestingly, functional annotation of almost 500 SNPs, that were observed to be significant at a genome-wide statistical threshold, found that most are in intronic (46%) or intergenic (29%) regions, with only 4 non-synonymous SNP associations observed, of which 2 were missense variants [7]. Furthermore, approximately half of the SNPs were implicated to impact gene transcription from gene regulation database analyses [7].
Second-generation sequencing technologies including whole-exome sequencing (WES) have been used in the diagnostic or research settings to identify genetic mutation(s) which may cause highly variable phenotypic expression in epileptic subjects [8,9,10]. The very nature of the WES approach favors detection of rarer highly penetrant gene-coding variants which are often hard to find in GWG-based GWAS approaches.
Performing WES in Saudi Arabian epilepsy populations offer a unique opportunity for the discovery of rare genetic variants impacting this disease as there is a high rate of consanguinity among large tribal pedigrees. A study in the Eastern province of Saudi Arabia has reported the prevalence of epilepsy to be around 6–7 per 1000 individuals [11]. In the present study, WES was performed on 144 individuals diagnosed with epilepsy with varying age-of-onset. An American College of Medical Genetics (ACMG) guideline-based variant prioritization approach followed WES which allowed for the discovery of potentially causative variants in our cohort of epilepsy subjects.
Materials and methods
Patient sampling and ethical approval
Over a period spanning 2018–2020, samples and data from consecutive subjects with epilepsy attending the Neurosurgery Clinics, King Fahd Hospital of the University, Al-Khobar, and King Fahd Hospital, Alhafof, Saudi Arabia, were collected for inclusion in this study. Participants ranged in age from 13–51 and were clinically diagnosed with epilepsy at the point of recruitment. The phenotype data of all subjects were reviewed by a consultant committee to verify uniformity among sites and eligibility consistent with International League Against Epilepsy [12]. In this study, the diagnosis of epilepsy was made by a consultant specializing in epilepsy based on the patients’ clinical history. Moreover, cases with moderate-to-severe intellectual disability, or cancer, were excluded from the study. If there was doubt regarding a patient’s phenotypic eligibility, the individual cases were reviewed by the consultant committee and if needed, additional data were requested prior to a decision being made by the committee regarding inclusion of the patient. However, on completion of the project the medical records of all patients were reviewed again. Among all our epileptic patients included in the study, eight patients also had type 2 diabetes, five patients had hypertension, one patient had cardiovascular disease and stroke, one patient had polycystic ovarian syndrome, and two patients had muscular dystrophy. Table 1 outlines the subjects’ demographic and clinical characteristics.
Ethical approval for the study was obtained from the local Institutional Review Board (IRB) committees (IRB-2015-01-063), and the study was conducted according to the ethical principles of the Declaration of Helsinki and Good Clinical Practice guidelines. All patients included in the study signed a written informed consent.
DNA sequencing, read alignment, variant calling and quality control
Blood samples were collected from subjects in EDTA vacutainers and after collection were immediately stored at − 80 °C. Standard DNA preparation was performed using DNeasy Blood kits (Qiagen, MD, USA). Whole-exome sequencing libraries were generated using the Agilent SureSelect Human All Exon Kit V5 (Agilent, CA, USA) and sequenced on a HiSeq 2500 instrument (Illumina, CA, USA) using standard paired-end sequencing protocol. Raw sequencing reads were stored as FASTQ files and then aligned to the human reference genome (GRCh37) using Illumina’s Dynamic Read Analysis for GENomics (DRAGEN) Pipeline. Resultant BAM files were position-sorted and duplicate reads marked. Single-sample gVCF files were generated by the DRAGEN Germline Pipeline, and joint calling of all samples in the study cohort were performed by DRAGEN Joint Genotyping.
Principal components analysis (PCA) and Kinship
KING was used for relatedness inference based on the genotype of exome SNPs (MAF > 0.01) [13]. Estimated kinship coefficient and number of SNPs with zero shared alleles (IBS0) between a pair of individuals were plotted. Parent–offspring, sibling pairs, and unrelated pairs can be distinguished as separate clusters on the scatterplot. Ancestry and kinship toolkit (AKT) was used to calculate PCAs and plot the results [14].
Variant annotation, filtering and prioritization
Variants were annotated with SnpEff to predict the effects of variants [15]. Rare variants were defined as minor allele frequency (MAF) < 1% in the Genome Aggregation Database (GnomAD) [16]. Intronic, synonymous, 3’ and 5’ UTR, up- and downstream variants were identified and excluded from the analysis. The remaining rare variants were considered to be potentially deleterious variants. Genetic variants classified in ClinVar as “Likely pathogenic” or “Pathogenic”, and in Human Gene Mutation Database (HGMD) as disease-causing mutations (DM) for epilepsy or seizures were collected and curated together with research literatures to server as the knowledgebase for variant prioritization and classification [17, 18].
Results
Principal component analysis
The common genetic variants of these Saudi epilepsy individuals show a unique cluster when compared to the world’s major populations based on principal component analysis (Fig. 1). The samples demonstrated a genetically matched background which avoided false attribution of associations due to population stratification.
The x-axis and y-axis denote the value of two components of PCA (PC1, PC2), with each dot in the figure representing one individual. The color for individuals belonging to the Epilepsy Disease study group is illustrated in black. The color for individuals from 1000 genome projects, Europeans (EUR), East Asians (EAS), Admixed Americans (AMR), South Asians (SAS), and Africans (AFR) is red, blue, green, purple and orange, respectively
Potentially pathogenic rare variants identified in 44 epilepsy subjects
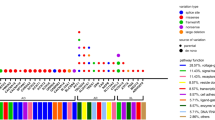
Based on a combination of variant filtering, and integration of variant databases in ClinVar, and HGMD, we identified a total of 32 potentially causative pathogenic variants across 30 different genes in 44/144 (30%) epilepsy subjects as shown in Table 2. Additional file 1: Supplementary Table S1 outlines additional minor allele frequencies in additional databases and further annotation of these putative pathogenic variants.
The 30 genes harboring the likely pathogenic variants observed in these 44 Saudi epilepsy subjects were then assessed for overlap with 102 previously collated monogenic epilepsy genes [7]. Likely pathogenic variants in 12 of these 102 monogenic epilepsy genes were observed in 44 epileptic subjects: CHRNA4, CLN3, CLN8, DEPDC5, KCNJ10, KCNMA1, POLG, PRICKLE1, SCN1A, SCN2A, SCN8A and SCN9A. Of the 18 additional genes from Table 2 with likely pathogenic variants, a number including SZT2, SCN10A, UBA5 have been reported in whole-exome sequencing in epilepsy subjects [19, 20]. Only one homozygous mutation, a stop-gain, was observed in single individual [21], in Potassium Calcium-Activated Channel Subfamily M Alpha 1 (KCNMA), a calcium-sensitive potassium channel gene which has been shown to have a role in general and early-onset epilepsy-related phenotypes [22,23,24,25,26]. This individual, a female who was diagnosed with childhood epilepsy at 12 years old, has one family member with a diagnosis of epilepsy and was assessed to have first degree of consanguinity.
Most commonly observed likely pathogenic variants
An in-frame insertion mutation in non-imprinted in Prader–Willi/Angelman syndrome region protein 2 (NIPA2) (chr15, GRCh37 position: 23006299) was observed in seven of the study subjects (shown in Table 3 along with age of onset). A missense variant in SH2B Adaptor Protein 3 (SH2B3) (chr12, position: 111856571) and in Cholinergic Receptor Nicotinic Alpha 4 Subunit (CHRNA4) (chr20 position: 61981924) were both observed in four individuals. Missense variants in STIL Centriolar Assembly Protein (STIL) (chr1, position: 47746675), and in Tryptophanyl-TRNA Synthetase 1 (WARS2) were both observed in three individuals.
Variants of unknown significance identified in epilepsy 133 subjects
In highly curated genomic disease databases such as ClinVar, there are a large number of variants of unknown significance (VUS), where there is unknown or conflicting clinical significance to date for association of such variants with epilepsy-related phenotypes. We identified 232 variants of unknown significance across 101 different genes in 133/144 (92%) subjects as shown in Additional file 2:Supplementary Table S2. Interestingly when the genes harboring these variants of unknown significance were intersected with the 102 previously collated monogenic epilepsy genes it was observed that 43 of these monogenic gene variants were enriched in the 101 loci with VUS from these 133 Saudi epilepsy subjects (Additional file 2: Table S2). We note that two individuals were observed to have homozygous potential pathogenic variants. One individual showed homozygosity for a missense variant in Spermatogenesis Associated 5 (SPATA5), with 3 individuals showing heterozygosity for this mutation (Additional file 2: Supplementary Table S2). SPATA5 has shown clear association with severe childhood epilepsy [27,28,29,30,31,32]. This female individual was diagnoses with childhood epilepsy at the age of 10 years old and two family members having a diagnosis of epilepsy, and both parents are listed as cousins.
Another homozygous mutation was observed in one individual for a missense mutation in Calcium Voltage-Gated Channel Subunit Alpha1 H (CACNA1H) with three additional individuals also carrying one copy of this mutation. Mutations in this gene have been associated with generalized and severe epilepsies [33, 34], although it has been debated whether this is a bona fide monogenic epilepsy gene [35]. This female individual was diagnosed with epilepsy at 15 years of age and does not have any other family members with a diagnosis of epilepsy, or any consanguinity noted.
Discussion
We performed the first whole-exome sequencing study in Saudi Arabia epilepsy subjects. Using 144 individuals, we compared putative pathogenic variants as well as variants of unknown significance with population-based whole-exome sequencing and whole genome sequencing databases.
The highest number of observed mutations across the 144 subjects were observed in NIPA2, a highly selective magnesium transporter. This in-frame insertion variant (NP001171818.1 p. (Asn334Glu335insAsp)) was observed in 7 subjects from 144 overall (5%). This variant has been previously reported within a population of subjects with childhood absence epilepsy (CAE) [36,37,38].
A missense variant in CHRNA4 was observed in 4 subjects. CHRNA4 is a nicotinic acetylcholine receptor, belonging to a superfamily of ligand-gated ion channels which play an established role in signal transmission at synapses. Mutations in CHRNA4 have been reported with nocturnal frontal lobe epilepsy type 1. A missense variant in SH2B3 was observed in 4 subjects. This gene is involved in a range of signaling activities by growth factor and cytokine receptors as part of the SH2B adaptor family of proteins. Mutations in this gene have been associated with susceptibility to celiac disease type 13 and susceptibility to insulin-dependent diabetes mellitus. It has low expression in the brain however as evident in the Genotype-Tissue Expression (GTEx) database. Missense mutations in STIL were observed in 3 subjects. STIL is a cytoplasmic protein which plays a role in the regulation of the mitotic checkpoint machinery. It too has low expression levels in all GTEx brain tissues.
There are a number of prioritized signals observed in this Saudi epilepsy study that may be novel or have very limited reports of association. Deficiency of WARS2 was observed in a patient with severe infantile-onset leukoencephalopathy, profound intellectual disability, spastic quadriplegia, epilepsy and microcephaly [39]. Rare mutations in DPYD have been implicated in children with unspecific neurological symptoms [40]. Epileptic encephalopathy caused by recessive loss-of-function (LoF) mutations have been reported in DENND5A [41]. A previous report of infantile cerebral and cerebellar atrophy showed association with a mutation in MED17 [42]. A LoF mutation in HCN4 has been reported to be associated with Familial benign myoclonic epilepsy in infancy [43]. Mutations in STRADA, SYNJ1, CACNA1A and NPRL3 have also been reported with severe epilepsy-related disease, but the association has not been reported for heterozygous variants in isolated forms of epilepsy [44,45,46,47,48,49,50,51].
A number of prioritized signals of putative pathogenicity were observed that have no reports of association with epilepsy in the literature including SEC24D, PCCA, MYO5A which may be strong candidates for further functional studies. SEC24D was reported to play a role in in vesicle trafficking and mutations in this gene are associated with Cole-Carpenter syndrome, a disorder affecting bone formation [52]. PCCA codes for the alpha subunit of the mitochondrial enzyme Propionyl-CoA carboxylase, and mutations in this gene leads to enzyme deficiency and are associated with propionic acidemia [53]. MYO5A encodes myosin 5A, and mutations in this gene are associated with Griscelli syndrome, which is characterized by hypopigmentation and a primary neurological abnormality [54]. These aforementioned genes may be good candidates for further functional studies.
This study is limited in that incomplete pedigrees and depth of sub-phenotyping are available, although putative pathogenic variants many known epilepsy-related loci are evident, and a number of potential new loci may be prioritized for further investigation. The Saudi population offers a lot of promise for elucidation of the genetic etiology of common diseases such as epilepsy due to consanguinity, with extended homozygosity stretches often observed over several megabases, affording the opportunity to enrich for recessive forms of epilepsy. While this study looked at 144 subjects, we are aiming to expand the cohort to encompass genetic analyses of extended pedigrees with additional phenotyping.
Conclusions
We identified for the first time 32 potentially causative pathogenic variants in Saudi individuals with epilepsy. In addition, several potential new loci have been identified that have no reports of association with epilepsy in other populations. These potentially causative pathogenic variants in these new loci may be prioritized for further functional studies.
Availability of data and materials
The datasets generated during the current study are available in the European Nucleotide Archive (ENA)repository, https://eur02.safelinks.protection.outlook.com/?url=https%3A%2F%2Fwww.ebi.ac.uk%2Fena%2Fbrowser%2Fview%2FPRJEB57370&data=05%7C01%7Caalali%40iau.edu.sa%7Cf185a40ee56a4cfbd98808dacb2affab%7C2c86bbfc8d0441ffa83a942f075e0f60%7C0%7C0%7C638045682787922255%7CUnknown%7CTWFpbGZsb3d8eyJWIjoiMC4wLjAwMDAiLCJQIjoiV2luMzIiLCJBTiI6Ik1haWwiLCJXVCI6Mn0%3D%7C2000%7C%7C%7C&sdata=49Th7XeOmQ6HTM69EHDOdReNEmdK7NEb2QrS%2FXWE%2B4w%3D&reserved=0,, under the title" Whole‐Exome Sequencing of a Saudi Epilepsy Cohort Reveals Association Signals in Known and Potentially Novel Loci" with accession number PRJEB57558. All requests for data can be sent to the corresponding author (AKA), and verified academic investigators will be granted full access.
References
England MJ, Liverman CT, Schultz AM, Strawbridge LM. Epilepsy across the spectrum: promoting health and understanding. A summary of the Institute of Medicine report. Epilepsy Behav. 2012;25(2):266–76.
Shorvon SD, Farmer PJ. Epilepsy in developing countries: a review of epidemiological, sociocultural, and treatment aspects. Epilepsia. 1988;29(Suppl 1):S36-54.
Brundtland GH. Welcome: The WHO view and launch of the second phase of the Global Campaign Against Epilepsy. Epilepsia. 2002;43(Suppl 6):5–6.
Hildebrand MS, Dahl HH, Damiano JA, Smith RJ, Scheffer IE, Berkovic SF. Recent advances in the molecular genetics of epilepsy. J Med Genet. 2013;50(5):271–9.
Annegers JF, Hauser WA, Anderson VE, Kurland LT. The risks of seizure disorders among relatives of patients with childhood onset epilepsy. Neurology. 1982;32(2):174–9.
International League Against Epilepsy Consortium on Complex Epilepsies. Electronic address e-auea. Genetic determinants of common epilepsies: a meta-analysis of genome-wide association studies. Lancet Neurol 2014;13:893–903.
International League Against Epilepsy Consortium on Complex E. Genome-wide mega-analysis identifies 16 loci and highlights diverse biological mechanisms in the common epilepsies. Nat Commun 2018;9:5269.
Muthaffar OY. The utility of whole exome sequencing in diagnosing pediatric neurological disorders. Balkan J Med Genet. 2020;23(2):17–24.
Sun H, Shen XR, Fang ZB, Jiang ZZ, Wei XJ, Wang ZY, et al. Next-generation sequencing technologies and neurogenetic diseases. Life (Basel). 2021;11(4):361.
Consortium EK, Project EPG. Ultra-rare genetic variation in common epilepsies: a case-control sequencing study. Lancet Neurol. 2017;16(2):135–43.
Pottoo FH, Alshayban DM, Joseph R, Al-Musa F, Al-Jabran O, Aljaafari D. Impact of adherence to antiepileptic medications on quality of life of epileptic patients in the Eastern Province of Saudi Arabia: a cross-sectional study. Imam J Appl Sci. 2020;2020(5):1.
Reynolds EH. The ILAE/IBE/WHO epilepsy global campaign history. International League Against Epilepsy. International Bureau for Epilepsy. Epilepsia. 2002;43(Suppl 6):9–11.
Manichaikul A, Mychaleckyj JC, Rich SS, Daly K, Sale M, Chen WM. Robust relationship inference in genome-wide association studies. Bioinformatics. 2010;26(22):2867–73.
Arthur R, Schulz-Trieglaff O, Cox AJ, O’Connell J. AKT: ancestry and kinship toolkit. Bioinformatics. 2017;33:142–4.
Cingolani P, Platts A, Wang LL, Coon M, Nguyen T, Wang L, et al. A program for annotating and predicting the effects of single nucleotide polymorphisms, SnpEff: SNPs in the genome of Drosophila melanogaster strain w1118; iso-2; iso-3. Fly. 2012;6(2):80–92.
Karczewski KJ, Francioli LC, Tiao G, Cummings BB, Alföldi J, Wang Q, et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature. 2020;581(7809):434–43.
Landrum MJ, Lee JM, Benson M, Brown G, Chao C, Chitipiralla S, et al. ClinVar: public archive of interpretations of clinically relevant variants. Nucleic Acids Res. 2016;44(D1):D862–8.
Stenson PD, Ball EV, Mort M, Phillips AD, Shiel JA, Thomas NS, et al. Human Gene Mutation Database (HGMD): 2003 update. Hum Mutat. 2003;21(6):577–81.
Kambouris M, Thevenon J, Soldatos A, Cox A, Stephen J, Ben-Omran T, et al. Biallelic. Ann Clin Transl Neurol. 2017;4(1):26–35.
Hong SY, Yang JJ, Li SY, Lee IC. A wide spectrum of genetic disorders causing severe childhood epilepsy in Taiwan: a case series of ultrarare genetic cause and novel mutation analysis in a pilot study. J Pers Med. 2020;10(4):281.
Al-Saady ML, Kaiser CS, Wakasuqui F, Korenke GC, Waisfisz Q, Polstra A, et al. Homozygous UBA5 variant leads to hypomyelination with thalamic involvement and axonal neuropathy. Neuropediatrics. 2021;52:489–94.
Lee CG, Lee J, Lee M. Multi-gene panel testing in Korean patients with common genetic generalized epilepsy syndromes. PLoS ONE. 2018;13(6): e0199321.
Yeşil G, Aralaşmak A, Akyüz E, İçağasıoğlu D, Uygur Şahin T, Bayram Y. Expanding the phenotype of homozygous. Balkan Med J. 2018;35(4):336–9.
Liang L, Li X, Moutton S, Schrier Vergano SA, Cogné B, Saint-Martin A, et al. De novo loss-of-function KCNMA1 variants are associated with a new multiple malformation syndrome and a broad spectrum of developmental and neurological phenotypes. Hum Mol Genet. 2019;28(17):2937–51.
Moldenhauer HJ, Matychak KK, Meredith AL. Comparative gain-of-function effects of the. J Neurophysiol. 2020;123(2):560–70.
Miller JP, Moldenhauer HJ, Keros S, Meredith AL. An emerging spectrum of variants and clinical features in. Channels. 2021;15(1):447–64.
Oesch G, Bozarth XL. Rufinamide efficacy and association with phenotype and genotype in children with intractable epilepsy: a retrospective single center study. Epilepsy Res. 2020;168: 106211.
Zanus C, Costa P, Faletra F, Musante L, Russo A, Grazian L, et al. Description of a peculiar alternating ictal electroclinical pattern in a young boy with a novel SPATA5 mutation. Epileptic Disord. 2020;22(5):659–63.
Braun F, Hentschel A, Sickmann A, Marteau T, Hertel S, Förster F, et al. Muscular and molecular pathology associated with SPATA5 deficiency in a child with EHLMRS. Int J Mol Sci. 2021;22(15):7835.
Papuc SM, Abela L, Steindl K, Begemann A, Simmons TL, Schmitt B, et al. The role of recessive inheritance in early-onset epileptic encephalopathies: a combined whole-exome sequencing and copy number study. Eur J Hum Genet. 2019;27(3):408–21.
Puusepp S, Kovacs-Nagy R, Alhaddad B, Braunisch M, Hoffmann GF, Kotzaeridou U, et al. Compound heterozygous SPATA5 variants in four families and functional studies of SPATA5 deficiency. Eur J Hum Genet. 2018;26(3):407–19.
Kurata H, Terashima H, Nakashima M, Okazaki T, Matsumura W, Ohno K, et al. Characterization of SPATA5-related encephalopathy in early childhood. Clin Genet. 2016;90(5):437–44.
Stringer RN, Jurkovicova-Tarabova B, Souza IA, Ibrahim J, Vacik T, Fathalla WM, et al. De novo SCN8A and inherited rare CACNA1H variants associated with severe developmental and epileptic encephalopathy. Mol Brain. 2021;14(1):126.34.
Wei Z, Liu C, Wu Z, Cao M, Qiao X, Han T, et al. The prognosis of epilepsy patients with CACNA1H missense variants: a longitudinal cohort study. Seizure. 2021;91:52–9.
Calhoun JD, Huffman AM, Bellinski I, Kinsley L, Bachman E, Gerard E, et al. CACNA1H variants are not a cause of monogenic epilepsy. Hum Mutat. 2020;41(6):1138–44.
Jiang Y, Zhang Y, Zhang P, Sang T, Zhang F, Ji T, et al. NIPA2 located in 15q11.2 is mutated in patients with childhood absence epilepsy. Hum Genet. 2012;131(7):1217–24.
Xie H, Zhang Y, Zhang P, Wang J, Wu Y, Wu X, et al. Functional study of NIPA2 mutations identified from the patients with childhood absence epilepsy. PLoS ONE. 2014;9(10): e109749.
Jiang Y, Zhang Y, Zhang P, Zhang F, Xie H, Chan P, et al. NIPA2 mutations are correlative with childhood absence epilepsy in the Han Chinese population. Hum Genet. 2014;133(5):675–6.
Theisen BE, Rumyantseva A, Cohen JS, Alcaraz WA, Shinde DN, Tang S, et al. Deficiency of WARS2, encoding mitochondrial tryptophanyl tRNA synthetase, causes severe infantile onset leukoencephalopathy. Am J Med Genet A. 2017;173(9):2505–10.
Schmidt C, Hofmann U, Kohlmüller D, Mürdter T, Zanger UM, Schwab M, et al. Comprehensive analysis of pyrimidine metabolism in 450 children with unspecific neurological symptoms using high-pressure liquid chromatography-electrospray ionization tandem mass spectrometry. J Inherit Metab Dis. 2005;28(6):1109–22.
Han C, Alkhater R, Froukh T, Minassian AG, Galati M, Liu RH, et al. Epileptic encephalopathy caused by mutations in the guanine nucleotide exchange factor DENND5A. Am J Hum Genet. 2016;99(6):1359–67.
Kaufmann R, Straussberg R, Mandel H, Fattal-Valevski A, Ben-Zeev B, Naamati A, et al. Infantile cerebral and cerebellar atrophy is associated with a mutation in the MED17 subunit of the transcription preinitiation mediator complex. Am J Hum Genet. 2010;87(5):667–70.
Campostrini G, DiFrancesco JC, Castellotti B, Milanesi R, Gnecchi-Ruscone T, Bonzanni M, et al. A loss-of-function. HCN4 mutation associated with familial benign myoclonic epilepsy in infancy causes increased neuronal excitability. Front Mol Neurosci. 2018;11:269.
Aerden M, Vallaeys L, Holvoet M, De Waele L, Van Den Bogaert K, Devriendt K. Homozygous missense STRADA mutation in a patient with polyhydramnios, megalencephaly and symptomatic epilepsy syndrome. Clin Dysmorphol. 2021;30(3):121–4.
Alsaif HS, Khashab HYEL, Alkuraya FS. Two further cases of polyhydramnios, megalencephaly, and symptomatic epilepsy syndrome, caused by a truncating variant in STRADA. Am J Med Genet A. 2021;185(2):604–7.
Samanta D, Arya K. Electroclinical findings of SYNJ1 epileptic encephalopathy. J Pediatr Neurosci. 2020;15(1):29–33.
Ben Romdhan S, Sakka S, Farhat N, Triki S, Dammak M, Mhiri C. A Novel SYNJ1 mutation in a Tunisian family with Juvenile Parkinson’s disease associated with epilepsy. J Mol Neurosci. 2018;66(2):273–8.
Hardies K, Cai Y, Jardel C, Jansen AC, Cao M, May P, et al. Loss of SYNJ1 dual phosphatase activity leads to early onset refractory seizures and progressive neurological decline. Brain. 2016;139(Pt 9):2420–30.
Dyment DA, Smith AC, Humphreys P, Schwartzentruber J, Beaulieu CL, Bulman DE, et al. Homozygous nonsense mutation in SYNJ1 associated with intractable epilepsy and tau pathology. Neurobiol Aging. 2015;36(2):1222.e1-5.
Dyment DA, Tétreault M, Beaulieu CL, Hartley T, Ferreira P, Chardon JW, et al. Whole-exome sequencing broadens the phenotypic spectrum of rare pediatric epilepsy: a retrospective study. Clin Genet. 2015;88(1):34–40.
Lyon SM, Waggoner D, Halbach S, Thorland EC, Khorasani L, Reid RR. Syndromic craniosynostosis associated with microdeletion of chromosome 19p13.12–19p13.2. Genes Dis. 2015;2(4):347–52.
Garbes L, Kim K, Rieß A, Hoyer-Kuhn H, Beleggia F, Bevot A, et al. Mutations in SEC24D, encoding a component of the COPII machinery, cause a syndromic form of osteogenesis imperfecta. Am J Hum Genet. 2015;96(3):432–9.
Wang Y, Sun Y, Jiang T. A novel PCCA mutation in a patient with late-onset propionic acidemia identified by genetic diagnosis panel. Front Pediatr. 2018;6:233.
Pastural E, Barrat FJ, Dufourcq-Lagelouse R, Certain S, Sanal O, Jabado N, et al. Griscelli disease maps to chromosome 15q21 and is associated with mutations in the myosin-Va gene. Nat Genet. 1997;16(3):289–92.
Acknowledgements
The authors would like to acknowledge the financial supported extended by King Abdulaziz City for Science and Technology, Riyadh, Saudi Arabia (Grant Number 14-MED81-46). We are also grateful to the nurses and technical staff for their work and dedication.
Funding
This work is supported by King Abdulaziz City for Science and Technology, Riyad, Saudi Arabia, Grant Number 14-MED81-46. This is a government agency. They have no role in the design, collection, analysis and interpretation of the data and writing of the manuscript.
Author information
Authors and Affiliations
Contributions
AHA, ASA, MA, DA, IK, AKA, AAA, FA, RA and SB were involved in the design of the work, critically revising the protocol, patient recruitment, analysis, interpretation of data and drafting of the manuscript. CC, DG, HL, BJK and AKA were involved in the design of the work, laboratory work, analysis, interpretation of data, critically revising the protocol and drafting the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received ethical approval from the Imam Abdulrahman bin Faisal University Ethical Committee (Reference: IRB-2015-01-063). The study was conducted according to the ethical principles of the Declaration of Helsinki and Good Clinical Practice guidelines. A signed informed consent form was obtained from each participating patient and control by the treating physicians prior to inclusion in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary Table S1: outlines additional minor allele frequencies in additional databases and further annotation of these putative pathogenic variants.
Additional file 2.
Supplementary Table S2: identified 232 variants of unknown significance across 101 different genes in 133/144 (92%) subjects.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Al Anazi, A.H., Ammar, A.S., Al-Hajj, M. et al. Whole‐exome sequencing of a Saudi epilepsy cohort reveals association signals in known and potentially novel loci. Hum Genomics 16, 71 (2022). https://doi.org/10.1186/s40246-022-00444-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40246-022-00444-6