Abstract
Background
Cognitive impairment is one of the non-motor symptoms in Parkinson’s disease (PD). In the present study, we aim to examine the cognitive function of non-demented Parkinson’s disease patients and compare the results between male and female patients as well as control groups in search of any gender effect.
Methods
Sixty PD Patients (30 males and 30 females) from the Movement Disorders Clinic at Huashan Hospital Affiliated to Fudan University were recruited to participate in the study. One hundred age and gender matched control subjects without neurological or psychiatric disorders were voluntarily recruited. The participants were administered measures of cognition in five domains including memory, language, spatial processing abilities, attention and executive function.
Results
PD patients attained significantly lower scores in the visual spatial function, language and attention/executive function compared with the control group. Anti-parkinsonian treated patients performed worse in Rey-copy score, Clock Drawing Test (CDT) and Verbal Fluency-City than untreated ones. In regard to gender differences, though no general cognitive differences were found in Mini-mental State Examination (MMSE), men surpassed women on Boston naming test (BNT) while women were superior on Auditory Verbal Learning Test-long (AVLT) delayed cued recall test.
Conclusions
Cognitive impairments were common in PD patients even in the absence of dementia. PD patients with anti-parkinsonian medication had worse cognitive impairment than untreated patients. Genders may have different manifestations of cognitive impairment in PD patients.
Similar content being viewed by others
Background
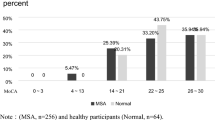
Parkinson’s disease (PD) has been considered a debilitating motor disorder, and the non-motor symptoms are gaining more and more attention. Cognitive impairment is a major non-motor symptoms, which greatly influence the quality of life [1]. It is estimated that 25% untreated ‘de novo’ patients have cognitive impairment of varying degrees. Some changes in cognition are subtle thus inconspicuous to the patients and their caregivers [2, 3]. Various studies have been conducted to measure specific cognitive functions in PD patients, such as executive abilities, working memory, visuospatial processing, language and attentional processes [4,5,6]. However, no agreement has been reached as to a definite neuropsychological profile of non-demented PD patients. Besides, it is reported that more men than women are diagnosed with PD, suggesting a gender difference in PD [7, 8]. Although a few studies addressed the gender differences in PD as well as the influence of estrogen on dopaminergic neurons and related pathways in the brain, most of them adopted general cognitive screening tools such as Mini-mental State Examination (MMSE) or Montreal Cognitive Assessment (MocA), little is known as to the specific cognitive domains influenced by gender [9,10,11,12]. Therefore, knowledge about differences in cognition between men and women with PD and about the pathophysiology underlying those differences may enhance the accuracy and effectiveness of clinical assessment and treatment of the disease.
The current study examined the five domains of cognitive function in non-demented PD patients who were not treated with anticholinergic medications and normal controls, with special emphasis on the comparison between male and female patients. Meanwhile, we performed sub-group analysis regarding medical treatment of PD patients, aiming to eliminate the possible confounding effects of medication and making the groups more comparable. As the effect of anti-parkinsonism medication on cognitive function was complicated and controversial [13,14,15].
Methods
Subjects
Patients were recruited from the Movement Disorders Clinic at Huashan Hospital Affiliated to Fudan University. All patients fulfilled the UK PD Society Brain Bank (PDSBB) diagnostic criteria for PD [16]. A total of 60 PD patients were recruited to participate in the study, including 30 males and 30 females. Every participant underwent a comprehensive neuropsychological assessment as part of a longitudinal study of cognition in PD patients. None of the patients complained of cognitive decline or visual hallucination. Dementia and depression were ruled out according to Diagnostic and Statistical Manual of Mental Disorders IV criteria [17]. Patients with the history of drug or alcohol abuse, cardiovascular disease, insulin - dependent diabetes, head trauma as well as those who underwent surgical relief of PD symptoms were excluded. One hundred age- and gender- matched control subjects with no neurological or psychiatric disorders were voluntarily recruited. The study was approved by the ethics committee of Huashan Hospital and written informed consent was obtained from each subject included in the study after the procedure was fully explained. Demographic and clinical data of all the PD patients are summarized in Table 1.
Procedure
All the evaluations were conducted or supervised by a licensed clinical neurologist. Stage of illness was determined using the Hoehn and Yahr scale [18]. PD duration was defined as the time between disease onset (self-reported onset of the first cardinal motor manifestation of Parkinsonism, i.e., rest tremor, rigidity, or bradykinesia) and the time of neuropsychological evaluation. The severity of the motor symptoms was assessed using part III of the Unified PD Rating Scale (UPDRS) (examined in the medication “off” phase) [19].
Participants were asked to provide information on their use of medication. Thirty-one of the patients were on anti-parkinsonian treatment at the time of investigation and 29 were untreated. Treatment included MAO-B inhibitors (n = 4), L-dopa monotherapy (n = 9), dopamine agonist monotherapy (n = 7), a combination of L-dopa and dopamine agonist (n = 12), a combination of L-dopa and MAO-B inhibitors (n = 2), or a combination of dopamine agonist and MAO-B inhibitors (n = 1). No patients were asked to change their medication for this study, nor were any receiving psychoactive or anticholinergic medication. Levodopa-equivalent daily dose (LEDD) was calculated according to standard conversion formula [20].
Neuropsychological tests were conducted in the morning under the “on” status, which was 30 to 60 min after taking the anti-parkinsonism medication. Subjects were allowed to take breaks when needed, in order to maximize performances. All tests were conducted according to standard procedure as outlined in test manuals. The test battery, which required approximately 2.0 h to complete, included a screening test of MMSE for global cognitive efficiency [21]. Five cognitive domains were evaluated: memory, language, spatial processing abilities, attention and executive function. All the tests were administered and scored according to published procedures which were shown in Table 2.
Data analysis
Statistical analysis was performed using the Statistical Package for Social Science (SPSS version 18 for windows, Baltimore). For comparisons, the Student’s T test was applied as the variables met the normal distribution, whereas the Manne Whitney test was used for the variables that did not meet the norms for using parametric statistics. Multiple linear regression was used to evaluate the effects of gender on cognitive function. A value of P < 0.05 was considered statistically significant.
Results
Demographic and clinical characteristics of participants
Demographic and clinical data of all the PD patients are summarized in Table 1. There was no significant difference between male and female patients, with respect to age, education, years of illness duration, mean UPDRS-III score, proportion of treatment, levodopa equivalent dose or disease severity. In the comparison of treated and untreated PD patients, we found much longer disease duration in the treated PD group, without any other demographic difference. The controls did not differ on age, education background or the dementia screening.
Cognitive performance
The results of neuropsychological tests in PD patients and controls are reported in Table 3. PD patients and controls did not differ on age, education background or the dementia screening (MMSE, p = 0.71). It is worth mentioning that under medication-naïve condition, male patients scored significantly worse in the MMSE (male-MMSE 28.43 ± 0.65, female-MMSE 29.20 ± 1.15, p = 0.014). The comparison between these two groups on specific cognitive measures revealed some differences. Three out of five domains were involved: the visual spatial function, language and attention/executive function. Specifically, PD patients attained significantly lower scores in AVLT-sum 1 to 5 (verbal memory, p = 0.000), Clock Drawing Test (Visual spatial function, p = 0.004), Verbal Fluency-City (Language, p = 0.000), Verbal Fluency-Alternative (Language, p = 0.003), Symbol Digit Modality Test (Attention/ executive function, p = 0.000) and Trail Making Test-A (Attention/ executive function, p = 0.000). Comparing with untreated PD, those with anti-Parkinsonism medication exhibited worse performance in Rey-copy score, Clock Drawing Test and Verbal Fluency-City. In the treated PD group, decreased score in Rey-copy test was observed, while there was no significant difference in the untreated group comparing with the controls (Table 4). Except for that, both treated and untreated PD patients displayed the same distinction in cognition tests with total PD patients as described above.
Table 5 summarizes the results of analyses of each gender, respectively. When compared with control, both male and female patients showed worse performance in Auditory Verbal Learning Test-sum (AVLT) 1 to 5 (Verbal memory, p = 0.000 for both male and female patients) and Symbol Digit Modality Test (Attention/ executive function, p = 0.000 for both male and female patients). Specifically, male patients performed worse on Verbal Fluency Test-Animals (Language, p = 0.000), Verbal Fluency-Cities (Language, p = 0.000) and Verbal Fluency-Alternatives (Language, p = 0.001), while female patients attained worse scores on Clock Drawing Test (Visual spatial function, p = 0.019), Boston Naming Test (Language, p = 0.02) and Trail Making Test-A (Attention/ executive function, p = 0.003).
Between male and female participants, the comparison of cognitive performance is also reported in Table 5. In the control group, males performed better on Verbal Fluency-City (Language, p = 0.01) and Verbal Fluency-Alternative (Language, p = 0.046). In the PD patient group, although male and female patients did not differ on the dementia screening test, male patients performed worse on AVLT-long delayed cued recall test (Verbal memory, p = 0.031) and BNT test (p = 0.003).
We have conducted multiple linear regression using age, gender, educational level, UPDRS-III and BECK as independent variables, eliminating the cofounders of age, educational level, UPDRS and BECK (Table 6). Considering the purpose of our article, we only demonstrated the β value and P value of gender. After adjustment of other cofounding factors, gender difference had significant effects on the AVLT-long delayed cued recall and BNT test, consistent with the results of student T test and Manne Whitney test.
More supporting data could be accessed through emails with the corresponding authors.
Discussion
PD patients frequently encounter neuropsychological problems. The present study has confirmed the previously reported cognitive impairment in cognitive domains including attention/executive function, visuospatial function, verbal memory and language. These aspects of cognition were all affected by the disease to varying degrees.
Dysexecutive syndrome is the most prominent prototype of early cognitive impairment in PD [22]. Deficits in this domain could be sensitively detected by measures of SDMT, which showed abnormality in this study. Our result was also in accordance with previous studies documenting visuospatial impairments by evidence of poor performance of PD patients in CDT [23]. Poor performance on free recall tasks but near normal performance on recognition and cued recall tasks in our study concur with the hypothesis that verbal memory impairment in PD has been manifested as retrieval difficulty more than encoding problems [22]. Although the majority of studies showed that language remain relatively intact in PD, we found it was impaired compared to the control group in the verbal fluency test. Verbal fluency combines the ability to retrieve the correct information and suppress the incorrect response. According to O’Brien’s report, dysfunction of various domains does not occur in isolation, but presents in association with each other [24]. In fact, though impairment in substantia nigra is most pronounced in PD, areas affected by the disease are widespread, including ventral tegmental area, dorsal raphe nucleus, hypothalamus, thalamus, hippocampus, cerebral cortex, the temporal, frontal, anterior cingulate and insular cortices [25]. Thus, it is not surprising that the cognitive deficits are due to cortical pathology and subcortical circuitry dysfunction as a whole and deficits in language may be the result of deterioration of the other cognitive functions as a whole. In addition to that, PD patients with anti-parkinsonism medication had extra deficits in Rey-copy score and stroop3 test score, which may due to the longer disease duration (p = 0.000) or medical effects. These results displayed a possible vulnerability of PD patients to the effects of disease duration and medication on Rey-copy score and stroop3 test.
In regard to gender differences in PD, epidemiological survey showed that the ratio of men and women who had the disease is approximately 2:1, suggesting a biological diversity [18]. However, not many studies considered gender when examining cognition in PD patients. There were some studies investigated the gender differences with a remarkable number of participants, but the lack of control groups did not permit to determine if these differences could be specific to PD patients [26, 27]. The present study highlights the role of gender differences associated with cognitive functions. The conclusion was strengthened by the study design of age and education matched control groups. Our study showed a disparity between male and female patients in two domains of cognition. Male patients surpassed female patients on BNT, a measure less commonly used to assess frontal lobe dysfunction [28], while female patients were superior on verbal retrieval test, reflecting the impairment of hippocampus [29]. Since no significant differences were observed in these two measures between male and female controls, it is reasonable to infer that gender-based differences existed in PD patients. In a cross-sectional study of the effect of gender on BNT which recruited 1111 healthy elderly subjects, there was also a tendentiously while non-significantly higher score of males (p = 0.08) [30]. Meanwhile, it reveals that age and educational level had more powerful effect on BNT. On the other hand, other studies found no effect of gender on the BNT. Therefore, there was possibility that the gender difference in BNT was due to the natural difference between men and women, which was unrelated to PD.
One consideration centers on our results is the role estrogen plays in the pathogenesis of PD. Even though the menopausal condition at experiment might be heterogeneous of the female PD patients in our cohort, the lifetime cumulative level of estrogen also played an important part in the pathogenesis of Parkinson’s disease [31, 32]. According to other’s reports, it is still a mystery as to the mechanism of estrogen acting on the dopaminergic system [33, 34]. In addition, the changes in other neurotransmitter systems, such as cholinergic, noradrenergic, serotonergic, also contribute to the multiple neuropsychological impairments. The interactions of these neurotransmitter systems make the role of estrogen even more complex. Another frequently-used theory to explain the gender differences is “cognitive reserve”, which posits that premorbid condition may generate distinctions in clinical presentation [35,36,37]. Although the subjects in our study have been adjusted for education, it may not be sufficient to rule out the impact of other socioeconomic factors such as occupation, income and social status. Thus better performance in verbal memory by female patients may indicate a larger cognitive reserve in this aspect. Likewise, advantages in naming by male patients may suggest a later onset of impairment and greater reserve of prefrontal function than female counterpart. The gender differences might also be associated with neural organization [38]. Some studies shown that greater bihemispheric representation were more prominent in women taking verbal memory task and men taking visuospatial task [39, 40]. Others found right hemispheric lateralization for males and bilateralization for females [41, 42]. Though no consensus has been reached, differences in neural lateralization render certain aspects of cognition more sensitive to neuropathological changes in a gender-specific manner, which lead to dissimilar manifestation in male and female patients.
When interpreting these data, several limitations should be acknowledged. First of all, the relatively small sample size may limit the generalization of these data. As several studies pointed out, normal elderly women performed better in tests involving verbal components [37, 43].Thus, whether female PD patients’ better performance in RVLT-long delayed cued recall was due to the influence of the disease needs further study with larger sample size. Secondly, as Cronin-Golomb described, side of disease onset may also influence the cognition of the patients [44]. Should this be the case, more detailed division of participants by both gender and side of disease onset would provide stronger evidence. Finally, another limitation is the influence of medication. Though anticholinergic medications were ruled out and levodopa equivalent dose were well matched between groups, the underlying effect of dopaminergic medication may still change the natural pathological development of neurodegeneration.
In conclusion, our study indicates that cognitive impairment was common in PD patients even in the absence of dementia. PD patients who underwent anti-parkinsonian treatment had worse cognitive impairment than untreated ones. In light of the above mentioned observations, we hypothesized that genders may have a different presentation of cognitive impairment in PD patients. Sex influences on brain anatomy, chemistry and functions are poorly understood. Increased knowledge on possible gender effects in PD would provide an enhanced insight in underlying pathological mechanisms, and has potential implications for the diagnosis and treatment of PD.
References
Schrag A, Jahanshahi M, Quinn N. What contributes to quality of life in patients with Parkinson's disease? J Neurol Neurosurg Psychiatry. 2000;69(3):308–12.
Muslimovic D, et al. Cognitive profile of patients with newly diagnosed Parkinson disease. Neurology. 2005;65(8):1239–45.
Aarsland D, Bronnick K, Fladby T. Mild cognitive impairment in Parkinson's disease. Curr Neurol Neurosci Rep. 2011;11(4):371–8.
Aarsland D, et al. Risk of dementia in Parkinson's disease: a community-based, prospective study. Neurology. 2001;56(6):730–6.
Allain H, et al. Procedural memory and Parkinson's disease. Dementia. 1995;6(3):174–8.
Brown RG, Marsden CD. Cognitive function in Parkinson's disease: from description to theory. Trends Neurosci. 1990;13(1):21–9.
Dluzen DE, McDermott JL. Gender differences in neurotoxicity of the nigrostriatal dopaminergic system: implications for Parkinson’s disease. J Gend Specif Med. 2000;3(6):36–42.
Van Den Eeden SK, et al. Incidence of Parkinson's disease: variation by age, gender, and race/ethnicity. Am J Epidemiol. 2003;157(11):1015–22.
Lyons KE, et al. Gender differences in Parkinson’s disease. Clin Neuropharmacol. 1998;21(2):118–21.
Braak H, et al. Cognitive status correlates with neuropathologic stage in Parkinson disease. Neurology. 2005;64(8):1404–10.
Nazem S, et al. Montreal cognitive assessment performance in patients with Parkinson’s disease with “normal” global cognition according to mini-mental state examination score. J Am Geriatr Soc. 2009;57(2):304–8.
Riedel O, et al. Cognitive impairment in 873 patients with idiopathic Parkinson’s disease. Results from the German study on epidemiology of Parkinson’s disease with dementia (GEPAD). J Neurol. 2008;255(2):255–64.
MacDonald AA, et al. Differential effects of Parkinson's disease and dopamine replacement on memory encoding and retrieval. PLoS One. 2013;8(9):e74044.
Edelstyn NM, et al. Effect of disease severity and dopaminergic medication on recollection and familiarity in patients with idiopathic nondementing Parkinson’s. Neuropsychologia. 2010;48(5):1367–75.
Hanna-Pladdy B, Pahwa R, Lyons KE. Paradoxical effect of dopamine medication on cognition in Parkinson’s disease: relationship to side of motor onset. J Int Neuropsychol Soc. 2015;21(4):259–70.
Daniel SE, Lees AJ. Parkinson’s disease society brain Bank, London: overview and research. J Neural Transm Suppl. 1993;39:165–72.
Runeson BS, Rich CL. Diagnostic and statistical manual of mental disorders, 3rd ed. (DSM-III), adaptive functioning in young Swedish suicides. Ann Clin Psychiatry. 1994;6(3):181–3.
Hoehn MM, Yahr MD. Parkinsonism: onset, progression and mortality. Neurology. 1967;17(5):427–42.
Goetz CG, et al. Movement Disorder Society-sponsored revision of the unified Parkinson’s disease rating scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord. 2008;23(15):2129–70.
Tomlinson CL, et al. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord. 2010;25(15):2649–53.
Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Higginson CI, et al. The relationship between executive function and verbal memory in Parkinson’s disease. Brain Cogn. 2003;52(3):343–52.
Cormack F, et al. Pentagon drawing and neuropsychological performance in dementia with Lewy bodies, Alzheimer’s disease, Parkinson’s disease and Parkinson’s disease with dementia. Int J Geriatr Psychiatry. 2004;19(4):371–7.
O'Brien TJ, et al. The contribution of executive control on verbal-learning impairment in patients with Parkinson’s disease with dementia and Alzheimer’s disease. Arch Clin Neuropsychol. 2009;24(3):237–44.
Tomer R, Levin BE, Weiner WJ. Side of onset of motor symptoms influences cognition in Parkinson’s disease. Ann Neurol. 1993;34(4):579–84.
Locascio JJ, Corkin S, Growdon JH. Relation between clinical characteristics of Parkinson's disease and cognitive decline. J Clin Exp Neuropsychol. 2003;25(1):94–109.
Solla P, et al. Gender differences in motor and non-motor symptoms among Sardinian patients with Parkinson’s disease. J Neurol Sci. 2012;323(1–2):33–9.
Green J, et al. Cognitive impairments in advanced PD without dementia. Neurology. 2002;59(9):1320–4.
Balthazar ML, et al. Learning, retrieval, and recognition are compromised in aMCI and mild AD: are distinct episodic memory processes mediated by the same anatomical structures? J Int Neuropsychol Soc. 2010;16(1):205–9.
Zec RF, et al. A cross-sectional study of the effects of age, education, and gender on the Boston naming test. Clin Neuropsychol. 2007;21(4):587–616.
Simon KC, et al. Reproductive factors, exogenous estrogen use, and risk of Parkinson’s disease. Mov Disord. 2009;24(9):1359–65.
Gatto NM, et al. Lifetime exposure to estrogens and Parkinson’s disease in California teachers. Parkinsonism Relat Disord. 2014;20(11):1149–56.
Liu B, Dluzen DE. Oestrogen and nigrostriatal dopaminergic neurodegeneration: animal models and clinical reports of Parkinson’s disease. Clin Exp Pharmacol Physiol. 2007;34(7):555–65.
Janowsky JS. The role of androgens in cognition and brain aging in men. Neuroscience. 2006;138(3):1015–20.
Stern Y. What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc. 2002;8(3):448–60.
Barnes LL, et al. Gender, cognitive decline, and risk of AD in older persons. Neurology. 2003;60(11):1777–81.
Beinhoff U, et al. Gender-specificities in Alzheimer’s disease and mild cognitive impairment. J Neurol. 2008;255(1):117–22.
Ripich DN, et al. Gender differences in language of AD patients: a longitudinal study. Neurology. 1995;45(2):299–302.
Volf NV, Razumnikova OM. Sex differences in EEG coherence during a verbal memory task in normal adults. Int J Psychophysiol. 1999;34(2):113–22.
Clements AM, et al. Sex differences in cerebral laterality of language and visuospatial processing. Brain Lang. 2006;98(2):150–8.
Antonova E, et al. The relationship between brain structure and neurocognition in schizophrenia: a selective review. Schizophr Res. 2004;70(2–3):117–45.
Gur RC, et al. An fMRI study of sex differences in regional activation to a verbal and a spatial task. Brain Lang. 2000;74(2):157–70.
Proust-Lima C, et al. Gender and education impact on brain aging: a general cognitive factor approach. Psychol Aging. 2008;23(3):608–20.
Cronin-Golomb A. Parkinson’s disease as a disconnection syndrome. Neuropsychol Rev. 2010;20(2):191–208.
Guo Q, et al. A comparison study of mild cognitive impairment with 3 memory tests among Chinese individuals. Alzheimer Dis Assoc Disord. 2009;23(3):253–9.
Caffarra P, et al. Rey-Osterrieth complex figure: normative values in an Italian population sample. Neurol Sci. 2002;22(6):443–7.
Guo Q, Fu J, Yuan J, et al. A study of validity of a new scoring system of clock drawing test. Chin J Neurol. 2008;41(4):234–7.
Lucas JA, et al. Mayo’s older African Americans normative studies: norms for Boston naming test, controlled oral word association, category fluency, animal naming, token test, WRAT-3 reading, trail making test, Stroop test, and judgment of line orientation. Clin Neuropsychol. 2005;19(2):243–69.
Zhao Q, et al. The Shape Trail test: application of a new variant of the trail making test. PLoS One. 2013;8(2):e57333.
Steinberg BA, et al. Mayo’s older Americans normative studies: age- and IQ-adjusted norms for the trail-making test, the Stroop test, and MAE controlled oral word association test. Clin Neuropsychol. 2005;19(3–4):329–77.
Acknowledgements
This work was supported by grants 81571232 and 81371413 from the National Natural Science Foundation of China (to Jian Wang), grant 81301136 from the National Natural Science Foundation of China (to Huan Yu). Project 2016YFC1306500 from Ministry of Science and technology of China (to Jian Wang), project XBR20134042 from Shanghai Municipal Health Bureau (to Huan Yu), project 15ZR1435800 from the Science and Technology Commission of Shanghai Municipality (to Jian-jun Wu).
Fundings
This work was supported by grants 81571232 and 81371413 from the National Natural Science Foundation of China (to Jian Wang), grant 81301136 from the National Natural Science Foundation of China (to Huan Yu). Project 2016YFC1306500 from Ministry of Science and technology of China (to Jian Wang), project XBR20134042 from Shanghai Municipal Health Bureau (to Huan Yu), Grant form Jingan District JA2015-Z002 (to Jian-jun Wu).
Availability of data and materials
Data could be accessed through emails with the corresponding authors.
Author information
Authors and Affiliations
Contributions
KY and BS were involved in the manuscript preparation, writing of the first draft, and statistical analysis with design and execution. DL, YW, JZ, JZ, W-BY, ZL, YT were involved in the initiation of the project, data collection, and review of the manuscript. HY, FL and JW were involved in organization and execution of the project, review and revision of the manuscript. JW and QG were involved in the conception, planning and supervising the execution of the research project, and critical revision final review of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the ethics committee of Huashan Hospital and written informed consent was obtained from each subject included in the study after the procedure was fully explained.
Competing interests
The authors declare that they have no competing interests.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yang, K., Shen, B., Li, Dk. et al. Cognitive characteristics in Chinese non-demented PD patients based on gender difference. Transl Neurodegener 7, 16 (2018). https://doi.org/10.1186/s40035-018-0120-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40035-018-0120-1