Abstract
Effective strategies to manage Burkholderia cepacia complex (Bcc) infections in cystic fibrosis (CF) patients are lacking. We tested combinations of clinically available antibiotics and show that moxifloxacin-ceftazidime could inhibit 16 Bcc clinical isolates at physiologically achievable concentrations. Adding low dose of colistin improved the efficacy of the combo, especially at conditions mimicking CF respiratory secretions.
Similar content being viewed by others
Introduction
Respiratory failure secondary to chronic pulmonary bacterial infection remains the primary cause of mortality and morbidity in cystic fibrosis (CF) patients [1]. We investigated the efficacy of non-standard antibiotic combinations to combat multidrug resistant Burkholderia cepacia complex (Bcc) bacteria. Bcc comprises a group of closely related species of which B. cenocepacia, B. multivorans, and B. contaminans are frequently isolated from CF patients [2, 3]. Bcc infections cause faster decline in lung function [4] and severely hinder post lung transplant survival of CF patients [5,6,7].
Effective management strategies are lacking for Bcc eradication in CF [8]. The EUCAST and the BSAC no longer provide recommendations for antimicrobial susceptibility testing against Bcc, while CLSI provides guidelines for seven agents to test for therapeutic use against Bcc [9]. These include three β-lactams (ceftazidime, meropenem, and ticarcillin-clavulanate), the fluoroquinolone levofloxacin, and trimethoprim-sulfamethoxazole combo (co-trimoxazole) in addition to the bacteriostatic drugs minocycline and chloramphenicol. New therapeutic solutions are being explored [10,11,12], but until they can be translated into clinical use, Bcc-infected patients are in dire need of effective therapeutics. We aimed to bridge this gap by finding novel combinations of clinically available antibiotics that could eradicate Bcc bacteria at physiologically relevant concentrations and could be readily used in patients. We focused on bactericidal antibiotics for which CLSI guidelines exist as candidates for combination therapy, avoiding previously tested combinations that showed no synergy against Bcc [13,14,15].
Methods
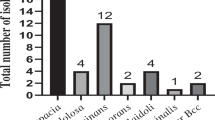
B. cenocepacia K56–2 was isolated from a CF patient in Canada and obtained from the B. cepacia Research and Referral Repository for Canadian CF Clinics (BCRRC); it is commonly used as a prototypic strain of the B. cenocepacia ET-12 epidemic clonal lineage [16]. A panel of 6 B. cenocepacia, 5 B. multivorans and 4 B. contaminans strains were isolated from CF patients. Bacteria were cultured in Luria-Bertani (LB) or Mueller-Hinton broth (MHB) media at 37 °C. LB is commonly used to grow Bcc isolates in our laboratory, while MHB is the recommended medium for standard antimicrobial susceptibility testing. MIC was initially determined by Etest strips (BioMérieux Inc., St. Laurent, Qc, Canada) as previously described [17].
Checkerboard assays were conducted with combinations of antibiotics (obtained from Sigma, St Louis, MO, USA) as previously described [10]. Initial assays against B. cenocepacia K56–2 were conducted in LB medium to select the most potent combination. Subsequent checkerboard assays of moxifloxacin-ceftazidime in the presence or absence of 4 μg/ml colistin sulphate against a panel of B. cenocepacia, B. multivorans and B. contaminans clinical isolates were conducted in MHB as recommended by CLSI for MIC testing by broth microdilution [18]. When accurate MIC values could not be determined, as for colistin methanesulfonate because Bcc bacteria grow at concentrations greater than its solubility in growth medium, the highest concentration tested was considered to be half the MIC value. Fractional inhibitory concentration indices (FICI) were calculated as FICI = A/MICA + B/MICB, where A and B are the concentrations of two antibiotics required in combination to inhibit bacterial growth and MICA and MICB are the MIC values for drugs A and B alone [19]. FICI data were interpreted as ‘synergy’ (FICI ≤ 0.5), ‘antagonism’ (FICI > 4.0), and ‘no interaction or indifference’ (FICI 1–4.0).
Artificial sputum medium (ASM) mimicking CF sputum was prepared as described [20] with the exception that components of the medium were autoclaved, filter-sterilized, or obtained already sterilized (instead of adding antibiotics). 20 mg/ml mucin (instead of 10 mg/ml) was added according to Quinn et al. [21]. Overnight cultures of B. cenocepacia K56–2 in LB medium were diluted in sterile ASM with or without antibiotic(s) to reach an inoculum equivalent to OD600 of 0.004 (~106 CFU/ml) and incubated at 37 °C without shaking. Bacterial growth was assessed by CFU count on LB agar plates at different time points.
Results and discussion
The MIC of individual antibiotics was first determined by Etest against B. cenocepacia K56–2 prior to combination testing. We tested ceftazidime, a representative β-lactam antibiotic that showed success in inhaled formulations for treating P. aeruginosa lower respiratory tract infections in CF patients [22], and has activity against B. cenocepacia [14, 17, 23]. Ceftazidime showed an MIC of 128 μg/ml against K56–2 (Fig. 1a). We tested levofloxacin and other fluoroquinolones from different generations; K56–2 displayed lower resistance levels to them, with norfloxacin being the least potent (MIC = 64 μg/ml) relative to the tested newer generation agents especially moxifloxacin (MIC = 8 μg/ml) (Fig. 1a). Co-trimoxazole showed an MIC of 16 μg/ml against the prototypic B. cenocepacia isolate; whereas, K56–2 was highly resistant to colistin (MIC >256 μg/ml) (Fig. 1a). Despite its lack of activity against Bcc, colistin was included in the study owing to its reported ability to permeabilize the cell envelope of Gram-negative bacteria to other antibiotics [24, 25]. Notably, the MIC of the tested antibiotics against K56–2 are above the CLSI clinical breakpoints for susceptibility.
Antibiotic combination testing against Bcc bacteria. a MIC by Etest against K56–2 at 24 h. b Checkerboard assays in LB medium against K56–2. c Checkerboards assays in MHB per CLSI microbroth dilution method against a panel of Bcc. d and e CFU counts in ASM; mean ± SEM, n = 4 from 2 independent experiments. Antibiotic concentrations are: (d) 8 μg/ml ceftazidime (Cef), 2 μg/ml moxifloxacin (Mox) and 10 μg/ml CMS; and (e) 16 μg/ml Cef, 10 μg/ml Mox and 20 μg/ml CMS
Next, we conducted checkerboard assays for select combinations against B. cenocepacia K56–2. Colistin methanesulfonate (CMS) showed borderline synergism with moxifloxacin (Fig. 1b). CMS is a less toxic prodrug of colistin that is active in vitro and in vivo [26, 27]; 4 μg/ml of CMS is equivalent to 1.5 μg/ml of colistin base activity [28]. The trimethoprim-CMS combination was synergistic whereas trimethoprim-moxifloxacin showed indifference (Fig. 1b). Furthermore, ceftazidime combinations with either moxifloxacin or CMS were synergistic (Fig. 1b). Since the combination of moxifloxacin and CMS was also synergistic, these 3 antibiotics (ceftazidime, moxifloxacin and CMS) were chosen for further follow-up testing.
We further tested whether the synergistic effects of these three antibiotics against K56–2 are reproducible against other clinical isolates of Bcc bacteria and in MHB following the CLSI guidelines. Checkerboard assays of ceftazidime-moxifloxacin combinations showed similar synergistic patterns against a panel of 7 B. cenocepacia, 5 B. multivorans and 4 B. contaminans in MHB (Fig. 1c). Such synergism remained, or even further increased in some cases, in the presence of 4 μg/ml colistin sulphate (Fig. 1c). More importantly, these antibiotic combinations inhibited the Bcc clinical isolates at or below the clinical breakpoints set by CLSI when in combination but not individually in most cases (Fig. 1c). The CLSI breakpoints are 8 μg/ml for ceftazidime; and 2 μg/ml for levofloxacin, which is closely related to moxifloxacin, for Bcc [9]. Therefore, this shows promise that triple combination of these antibiotics would eradicate Bcc at clinically achievable concentrations.
To test the efficacy of these combinations in CF sputum-like conditions, we used an artificial CF sputum medium (ASM) and determined the CFUs of K56–2 at different time points following treatment with the antibiotic combinations. Low antibiotic concentrations, equivalent to the CLSI breakpoints where available (8 μg/ml ceftazidime, 2 μg/ml moxifloxacin and 10 μg/ml CMS), resulted in killing of only ~1-log at the 4 h time-point compared to the initial inoculum (up to 2-log less than the untreated control at the same time-point) in ASM (Fig. 1d). Reduced antibiotic efficiencies in ASM compared to LB and MHB is not unexpected given the reported lack of correlation between in vitro susceptibility testing results performed in standard laboratory media as MHB and the clinical outcome in CF patients [29]. Therefore, higher antibiotic concentrations were tested in ASM (Fig. 1e). Moxifloxacin (at 10 μg/ml) had a bacteriostatic effect with no appreciable change in survival over 24 h compared to the initial inoculum (2-log reduction in CFU compared to control at 24 h). Ceftazidime at 16 μg/ml resulted in significant initial killing of 2-log CFU from the starting inoculum (up to 3-log CFU reduction relative to the control at 6 h). However, overgrowth of resistant cells occurred at 24 h leading to only 1-log reduction compared to control values at the same time-point and an increase of almost 2-log CFU relative to the initial inoculum. Combining moxifloxacin with ceftazidime prevented overgrowth of resistant cells and sustained the killing effect of ceftazidime until 24 h (5-log reduction compared to the untreated control at 24 h). CMS at 20 μg/ml further reduced the CFU by 1-log (3-log CFU killing relative to the initial inoculum or 6-log total CFU reduction compared to untreated control at 24 h) when combined with moxifloxacin and ceftazidime (Fig. 1e). These concentrations, although slightly above the CLSI breakpoints, are physiologically achievable in respiratory fluids and tissues (see FDA documents available for moxifloxacin [30] and for ceftazidime [31]).
In summary, we report novel double and triple antibiotic combinations that inhibit Bcc bacteria at physiologically achievable concentrations and hence could be ready for immediate use in patients. In addition, nanotechnology-based novel respiratory delivery systems may deliver even higher doses of these antibiotics at the local site of infection. For example, a pilot trial of long-term administration of tobramycin inhalation powder delivered using a Podhaler has shown some promise for CF patients chronically infected with Bcc [32], despite the low efficiency of tobramycin against Bcc in vitro [33]. We then propose these combinations as ideal targets for experimental screening of novel antibiotic adjuvants for enhanced efficacy against Bcc bacteria.
Abbreviations
- EUCAST:
-
European Committee on Antimicrobial Susceptibility Testing
- BSAC:
-
British Society of Antimicrobial Chemotherapy
- CLSI:
-
Clinical and Laboratory Standards Institute
References
Waters V. New treatments for emerging cystic fibrosis pathogens other than pseudomonas. Curr Pharm Des. 2012;18:696–725.
Reik R, Spilker T, Lipuma JJ. Distribution of Burkholderia cepacia complex species among isolates recovered from persons with or without cystic fibrosis. J Clin Microbiol. 2005;43:2926–8.
Medina-Pascual MJ, Valdezate S, Carrasco G, Villalon P, Garrido N, Saez-Nieto JA. Increase in isolation of Burkholderia contaminans from Spanish patients with cystic fibrosis. Clin Microbiol Infect. 2015;21:150–6.
Speert DP, Henry D, Vandamme P, Corey M, Mahenthiralingam E. Epidemiology of Burkholderia cepacia complex in patients with cystic fibrosis, Canada. Emerg Infect Dis. 2002;8:181–7.
De Soyza A, Meachery G, Hester KL, Nicholson A, Parry G, Tocewicz K, Pillay T, Clark S, Lordan JL, Schueler S, et al. Lung transplantation for patients with cystic fibrosis and Burkholderia cepacia complex infection: a single-center experience. J Heart Lung Transplant. 2010;29:1395–404.
Morrell MR, Pilewski JM. Lung transplantation for cystic fibrosis. Clin Chest Med. 2016;37:127–38.
Stephenson AL, Sykes J, Berthiaume Y, Singer LG, Aaron SD, Whitmore GA, Stanojevic S. Clinical and demographic factors associated with post-lung transplantation survival in individuals with cystic fibrosis. J Heart Lung Transplant. 2015;34:1139–45.
Regan KH, Bhatt J. Eradication therapy for Burkholderia cepacia complex in people with cystic fibrosis. Cochrane Database Syst Rev. 2016;11:CD009876.
CLSI. Performance Standards for Antimicrobial Susceptibility Testing. CLSI supplement M100. In: Wayne PA, editor. Clinical and Laboratory Standards Institute. 27th ed; 2017.
Loutet SA, El-Halfawy OM, Jassem AN, Lopez JM, Medarde AF, Speert DP, Davies JE, Valvano MA. Identification of synergists that potentiate the action of polymyxin B against Burkholderia cenocepacia. Int J Antimicrob Agents. 2015;46:376–80.
Selin C, Stietz MS, Blanchard JE, Gehrke SS, Bernard S, Hall DG, Brown ED, Cardona STA. Pipeline for screening small molecules with growth inhibitory activity against Burkholderia cenocepacia. PLoS One. 2015;10:e0128587.
McClean S, Healy ME, Collins C, Carberry S, O'Shaughnessy L, Dennehy R, Adams A, Kennelly H, Corbett JM, Carty F, et al. Linocin and OmpW are involved in attachment of the cystic fibrosis-associated pathogen Burkholderia cepacia complex to lung epithelial cells and protect mice against infection. Infect Immun. 2016;84:1424–37.
Zhou J, Chen Y, Tabibi S, Alba L, Garber E, Saiman L. Antimicrobial susceptibility and synergy studies of Burkholderia cepacia complex isolated from patients with cystic fibrosis. Antimicrob Agents Chemother. 2007;51:1085–8.
Aaron SD, Ferris W, Henry DA, Speert DP, Macdonald NE. Multiple combination bactericidal antibiotic testing for patients with cystic fibrosis infected with Burkholderia cepacia. Am J Respir Crit Care Med. 2000;161:1206–12.
Van den Driessche F, Vanhoutte B, Brackman G, Crabbe A, Rigole P, Vercruysse J, Verstraete G, Cappoen D, Vervaet C, Cos P, et al. Evaluation of combination therapy for Burkholderia cenocepacia lung infection in different in vitro and in vivo models. PLoS One. 2017;12:e0172723.
Mahenthiralingam E, Coenye T, Chung JW, Speert DP, Govan JR, Taylor P, Vandamme P. Diagnostically and experimentally useful panel of strains from the Burkholderia cepacia complex. J Clin Microbiol. 2000;38:910–3.
El-Halfawy OM, Valvano MA. Chemical communication of antibiotic resistance by a highly resistant subpopulation of bacterial cells. PLoS One. 2013;8:e68874.
CLSI. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard—ninth edition. CLSI document M07-A9. In: Wayne PA, editor. Clinical and Laboratory Standards Institute; 2012.
Vaara M, Porro M. Group of peptides that act synergistically with hydrophobic antibiotics against gram-negative enteric bacteria. Antimicrob Agents Chemother. 1996;40:1801–5.
Fung C, Naughton S, Turnbull L, Tingpej P, Rose B, Arthur J, Hu H, Harmer C, Harbour C, Hassett DJ, et al. Gene expression of Pseudomonas aeruginosa in a mucin-containing synthetic growth medium mimicking cystic fibrosis lung sputum. J Med Microbiol. 2010;59:1089–100.
Quinn RA, Whiteson K, Lim YW, Salamon P, Bailey B, Mienardi S, Sanchez SE, Blake D, Conrad D, Rohwer FA. Winogradsky-based culture system shows an association between microbial fermentation and cystic fibrosis exacerbation. ISME J. 2015;9:1024–38.
Falagas ME, Trigkidis KK, Vardakas KZ. Inhaled antibiotics beyond aminoglycosides, polymyxins and aztreonam: a systematic review. Int J Antimicrob Agents. 2015;45:221–33.
Lupo A, Isis E, Tinguely R, Endimiani A. Clonality and antimicrobial susceptibility of Burkholderia cepacia complex isolates collected from cystic fibrosis patients during 1998-2013 in Bern, Switzerland. New Microbiol. 2015;38:281–8.
Gordon NC, Png K, Wareham DW. Potent synergy and sustained bactericidal activity of a vancomycin-colistin combination versus multidrug-resistant strains of Acinetobacter baumannii. Antimicrob Agents Chemother. 2010;54:5316–22.
Aoki N, Tateda K, Kikuchi Y, Kimura S, Miyazaki C, Ishii Y, Tanabe Y, Gejyo F, Yamaguchi K. Efficacy of colistin combination therapy in a mouse model of pneumonia caused by multidrug-resistant Pseudomonas aeruginosa. J Antimicrob Chemother. 2009;63:534–42.
Yapa SWS, Li J, Patel K, Wilson JW, Dooley MJ, George J, Clark D, Poole S, Williams E, Porter CJ, et al. Pulmonary and systemic pharmacokinetics of inhaled and intravenous colistin methanesulfonate in cystic fibrosis patients: targeting advantage of inhalational administration. Antimicrob Agents Chemother. 2014;58:2570–9.
Li J, Turnidge J, Milne R, Nation RL, Coulthard K. vitro pharmacodynamic properties of colistin and colistin methanesulfonate against Pseudomonas aeruginosa isolates from patients with cystic fibrosis. Antimicrob Agents Chemother. 2001;45:781–5.
Li J, Nation RL, Turnidge JD, Milne RW, Coulthard K, Rayner CR, Paterson DL. Colistin: the re-emerging antibiotic for multidrug-resistant gram-negative bacterial infections. Lancet Infect Dis. 2006;6:589–601.
Hurley MN, Ariff AH, Bertenshaw C, Bhatt J, Smyth AR. Results of antibiotic susceptibility testing do not influence clinical outcome in children with cystic fibrosis. Journal of cystic fibrosis: official journal of the European cystic fibrosis. Society. 2012;11:288–92.
FDA Record on Avelox. 1999. [https://www.accessdata.fda.gov/drugsatfda_docs/nda/99/21-085_Avelox_biopharmr.pdf].
FDA Record on Fortaz. 2007. [https://www.accessdata.fda.gov/drugsatfda_docs/label/2007/050578s053,050634s020lbl.pdf].
Waters V, Yau Y, Beaudoin T, Wettlaufer J, Tom SK, McDonald N, Rizvi L, Klingel M, Ratjen F, Tullis E. Pilot trial of tobramycin inhalation powder in cystic fibrosis patients with chronic Burkholderia cepacia complex infection. Journal of cystic fibrosis: official journal of the European cystic fibrosis. Society. 2017;16:492–5.
Ratjen A, Yau Y, Wettlaufer J, Matukas L, Zlosnik JE, Speert DP, LiPuma JJ, Tullis E, Waters V. In vitro efficacy of high-dose tobramycin against Burkholderia cepacia complex and Stenotrophomonas maltophilia isolates from cystic fibrosis patients. Antimicrob Agents Chemother. 2015;59:711–3.
Acknowledgements
M.A.V. acknowledges participation in COST action BM1003 “Microbial cell surface determinants of virulence as targets for new therapeutics in cystic fibrosis”.
Funding
Research by the authors was funded by grants from Cystic Fibrosis Canada, The Cystic Fibrosis Trust and The Infection and Immunity Translational Research Group, Northern Ireland HSC. The funding bodies did not have any roles in the design of the study and collection, analysis, and interpretation of data or in writing the manuscript.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Author information
Authors and Affiliations
Contributions
OME planned and conducted most of the experiments; MMN performed and critically analysed MICs; OME, MMN wrote and edited the manuscript. MAV directed the research, analyzed the results, and provided feedback on experimental strategies. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
El-Halfawy, O.M., Naguib, M.M. & Valvano, M.A. Novel antibiotic combinations proposed for treatment of Burkholderia cepacia complex infections. Antimicrob Resist Infect Control 6, 120 (2017). https://doi.org/10.1186/s13756-017-0279-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13756-017-0279-8