Abstract
Background
Hypoxemia is a severe condition associated with high rates of mortality, particularly in low- and middle-income countries (LMICs) with poor access to oxygen therapy. Despite its clinical significance, there have been few studies to describe the burden of hypoxemia. Thus, the primary objective of this study is to systematically describe the prevalence of hypoxemia among pediatric and adult patients in low- and middle-income countries.
Methods/design
Standard systematic review methods will be used. Bibliographic databases (MEDLINE, EMBASE, CINAHL) will be searched from 1998 onwards. The search strategy aims to identify studies that have measured peripheral blood oxygen saturation (SpO2) in children and adults presenting to health facilities in LMICs. Studies will be included if oxygen saturation measurements by pulse oximetry were measured. No studies will be excluded based on study design though patients recruited from intensive care units and post-operative care will be excluded. The primary outcome is the prevalence of hypoxemia on presentation to the healthcare facility. We define hypoxemia on the basis of SpO2 measurements, and use a threshold of SpO2 less than 90% at sea level though allow for a lower threshold for studies conducted at higher altitude and where justified. Standardized tools will be used to extract data on number of patients with SpO2 measurements, number of patients with hypoxemia, patient population characteristics, and study characteristics. Quality of the included studies will be assessed using the “Checklist for Prevalence Studies” developed by the Joanna Briggs Institute. If there are enough studies to do so, we will conduct meta-analysis using a random effects model to estimate prevalence of hypoxemia and conduct subgroup analyses by age and disease groups.
Discussion
Hypoxemia is a critical condition and understanding the burden of hypoxemia may support decision-making in LMICs to deploy pulse oximeters and oxygen treatments more efficiently to address diseases and patient populations with the highest burden. Previous studies on hypoxemia prevalence have focused too narrowly on a few diseases or specific patient populations (e.g., pneumonia in children under five) whereas any effort to improve access to oxygen requires understanding of the potential demand for oxygen for all diseases and population groups. Governments, UN agencies, donors, and NGOs are investing strongly to improve oxygen systems in LMICs. Effective oxygen system planning requires estimation of oxygen need, informed by robust data on hypoxemia prevalence and admission patterns at all the levels of the health system. This study aims to fill that gap by providing comprehensive estimates of hypoxemia prevalence.
Systematic review registration
PROSPERO CRD42019136622.
Similar content being viewed by others
Background
Hypoxemia is a severe condition characterized as insufficient oxygen in the blood. Many diseases can cause hypoxemia, including pneumonia, malaria, neonatal sepsis, anemia, pulmonary diseases in adults, and adult heart failure, and can cause hypoxemia in different ways. For pneumonia, (one of the most common causes of hypoxemia especially in children), hypoxemia is primarily caused by obstruction of oxygen exchange in the alveoli of the lungs. A systematic review found that hypoxemia is a strong predictor of mortality for pneumonia in children, and other studies have also found hypoxemia to be associated with mortality and other poor outcomes for other diseases [1,2,3,4,5,6]. Patients in low- and middle-income countries (LMICs) are disproportionately affected as oxygen therapy, an effective treatment of hypoxemia, is not widely accessible [7, 8]. Despite the clinical significance of hypoxemia, there are few studies that have estimated the burden of hypoxemia. We found one systematic review of the prevalence of hypoxemia [9]. The systematic review included 24 studies and found hypoxemia prevalence estimates ranging between 2-23% across eight conditions in children. However, the review was limited to children younger than 12 years, and as oxygen is applicable to adolescents and adults with hypoxemia as well, an updated review including older age groups would help inform initiatives trying to improve oxygen access in LMICs. Furthermore, prevalence of diseases across LMICs is likely to differ and so providing rigorous estimates of hypoxemia prevalence across a wider range of diseases than that included in the earlier systematic review will also help improve plans for increasing oxygen access.
Methods/design
Aims and objectives
The aim of the study is to describe the prevalence of hypoxemia among pediatric and adult patients presenting to healthcare facilities in LMICs.
Selection criteria
The search strategy and selection criteria are described below.
Participants
Patients of all ages presenting to a health facility with acute illnesses for whom oxygen saturation measurements by pulse oximetry (SpO2) were measured. The following is a comprehensive, though non-exhaustive list of conditions for which studies may report hypoxemia prevalence:
Respiratory conditions:
Pneumonia/bronchiolitis/acute lower respiratory infection (ALRI)
Tuberculosis
Neonatal—prematurity/respiratory distress syndrome (RDS)
Chronic obstructed pulmonary disease (COPD)
Asthma
HIV-related infections—pneumocystis pneumonia (PJP)
Non-respiratory conditions:
Infections: sepsis, meningitis/encephalitis, malaria
Neurological: neonatal encephalopathy/asphyxia, stroke, seizures
Malignancies
Trauma/injury
Pregnancy—post-partum hemorrhage (PPH), eclampsia, and pre-eclampsia
Malnutrition (broad but will yield relevant studies): severe acute malnutrition (SAM)/moderate acute malnutrition (MAM)
The study will exclude studies of patients recruited from intensive care units (likely multi-factorial etiology of hypoxemia and mechanical ventilation) and post-operative care, or who are admitted for elective procedures. We will also exclude studies at high risk of selection bias based on quality assessments conducted by the reviewers (See the “Quality assessment” section).
Intervention
Only studies in which pulse oximetry was conducted will be included in the review. Pulse oximetry uses the differences in absorbance of two different wavelengths of light by oxygenated and deoxygenated hemoglobin to non-invasively estimate arterial oxygen saturation (recording peripheral oxygen saturation, or SpO2). It is well correlated with arterial oxygen saturation measured by blood gas analysis (PaO2), and is much cheaper and does not require the infrastructure and upkeep of blood gas machines, making the technology more applicable to LMIC settings. The World Health Organization recommends using pulse oximetry for detection of hypoxemia [10].
Setting
Studies conducted in low and lower-middle income countries as defined by the World Bank 2019 country classification list will be included in the study [11]. We will include only studies conducted in a health facility (any level) though we will exclude studies conducted within intensive care units and post-operative care.
Timing
Pulse oximetry is a relatively recent technology in LMICs. Several studies highlighting poor access to it in the perioperative setting have been published in the mid-2000s, and it was part of WHO’s Surgical Safety Checklist in 2009. To ensure a sensitive search strategy, we have included studies published a decade earlier, since January 1, 1998.
Study designs
No studies will be excluded based on the study design. There are few studies designed specifically to estimate hypoxemia prevalence as the primary outcome, but rather, hypoxemia is included as part of the clinical studies for a variety of other reasons (e.g., control variable or identification of severe illness). Thus, we will take a broad review of all studies that measured peripheral blood oxygen using pulse oximetry.
Outcomes
The primary outcome of interest is the prevalence of hypoxemia on presentation to the healthcare facility. We define hypoxemia on the basis of SpO2 measurements, and use a threshold of SpO2 less than 90% at sea level. With higher altitude, the partial pressure of oxygen reduces, and studies have demonstrated lower levels of what is considered normal SpO2 in healthy populations. Therefore, we will allow for adjustment in the definition of hypoxemia with altitude, where authors took this into account, and using an alternate definition with a lower threshold of SpO2. For studies that applied a threshold of hypoxemia likely to overestimate prevalence (such as a threshold level above SpO2 of 90% at sea level), we will exclude the study unless the authors can be contacted to provide prevalence data for the standard threshold or we are able to obtain the dataset for re-analysis to the standard threshold definition. We will include all studies which collected SpO2 measurements, even if hypoxemia was not the primary outcome.
Language
Studies published in English, French, and Spanish will be included in the review.
Information sources
We will search for published studies and datasets using the following databases: MEDLINE, PubMed (for studies published, studies in the past year that have not yet been indexed on MEDLINE), EMBASE, CINAHL, and the Index Medicus for each WHO region, and Google Scholar (the first 500 abstracts will be reviewed).
To ensure comprehensiveness of the literature search, we will also scan the reference lists of included studies or relevant reviews identified. We will also seek out unpublished data sets from key researchers in the field. We will contact researchers who are known to have done studies in low- and middle-income countries where oximetry was recorded.
Search strategy
The search strategy aims to identify studies that have collected SpO2 measurements using pulse oximetry on patients meeting the criteria described above. The specific search strategies will be developed in consultation with a health sciences research librarian with expertise in systematic reviews. A draft MEDLINE search strategy is included in Additional file 1: Appendix 1 and has been informed by prior experience in conducting a systematic review on hypoxemia prevalence in children less than 12 years [9]. After the MEDLINE search strategy is finalized, it will be adapted to the syntax and subject headings of other databases.
Study records
Data management
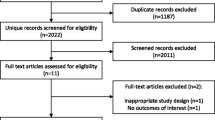
Search results will be documented in an electronic database such as Excel or Google Sheets. A template for documenting search results is included in Additional file 1: Appendix 2. A standardized form (Additional file 1: Appendix 3) will be used to screen and select studies. Each publication will be assigned a “Report ID,” and where there are multiple publications coming from the same study, each study will also be assigned a single “Study ID.” During the screening process, we will identify duplication of studies reported across multiple publications and multiple databases and remove duplicates from our study database. For studies meeting the screening criteria, the form will also be used to extract relevant study variables for analysis and quality assessment. We will pilot the study forms using the first 20 studies found using the search strategy and amend the form as necessary before implementing it on the entire search results. The full text articles of studies selected for inclusion will be uploaded to Endnote.
Selection process
Two independent reviewers will screen the full text of all studies resulting from the search strategy and use the data extraction and assessment form to screen studies for inclusion. Disagreements between the two reviewers will be screened by a third independent reviewer. For studies where any of the eligibility criteria are unclear, the reviewers will attempt to contact the study’s corresponding author for clarification. Three attempts will be made to contact the study’s corresponding author. If all three attempts fail, the study will be excluded from the review.
Data collection process
For all studies meeting the inclusion criteria, one reviewer will extract data from the reports. The data extraction and assessment form will be used, and the data will be entered into an electronic database. For studies not reporting summary statistics on SpO2, the reviewer will reach out to the study’s corresponding author to request for the study’s dataset. We will use the draft letter in Additional file 1: Appendix 4. Three attempts will be made to contact the study’s corresponding author. If all three attempts fail, the study will be excluded from the review.
Data items
The data items we aim to extract include the following:
Numbers of patients with hypoxemia at presentation or first recording thereafter and total number of patients screened
Patient population information, including number of patients included in the study, age range of study population, inclusion and exclusion criteria, and diagnostic case definitions (e.g., WHO defined severe pneumonia)
Study characteristics, including the study’s aim, the study design, the healthcare setting where the study was conducted, elevation above sea level where study was conducted, and time period where the study was conducted
Outcomes and prioritization
The primary outcome of interest is the proportion of patients with hypoxemia (SpO2 < 90%) on presentation to the facility. If the primary outcome is not reported, a secondary outcome using another SpO2 cutoff may be used if adequate justification was used for the alternate cutoff. We will contact authors for the dataset and re-analyze the data to standardize the definition of hypoxemia if possible.
Quality assessment
We will use the “Checklist for Prevalence Studies” developed by the Joanna Briggs Institute for assessing study quality at the study level [12]. The ‘Checklist for Prevalence Studies’ assesses study quality along nine components: appropriate sampling frame, appropriate sampling design, adequate sample size, detailed description of study subjects and setting, sufficient coverage of sample, valid methods for identifying the condition, standard and reliable measurement of the condition, appropriate statistical analysis, and adequate response rate. Study quality will be assessed by two reviewers, and with agreement of the two reviewers, we will exclude studies where there was high potential for selection bias, such as where there was selective recruitment of sub-populations of patients with more severe illness, or where oximetry was not measured and recorded in a systematic way within the study. Where there are disagreements between the two reviewers, a third independent reviewer will assess the study quality for a final determination.
We will also assess for publication bias of selective populations by seeking out unpublished data from researchers. Published studies may represent populations with high prevalence of hypoxemia, such as cohorts in large tertiary hospitals wherein severity of illness is usually higher.
Some studies may also have selective definitions of hypoxemia that may result in over- or under-reporting of hypoxemia. Where possible, we will request the data from the authors for re-analysis to standardize the definition of hypoxemia to SpO2 < 90%. As mentioned above, we will allow for lower thresholds of hypoxemia due to altitude where authors have provided such information.
We will also assess for the possible presence of small sample bias in the publication literature using funnel plots and test for asymmetry using Egger’s test [13].
Data synthesis
Statistical analysis will be done using the Stata 16 statistical software (Statacorp, College Station, Texas, USA). We will report hypoxemia prevalence for the following subgroups: age, diagnosis (and severity), level of health facility (primary, secondary, tertiary), and altitude. For age, we will stratify results into three age categories: neonates (< 28 days of age), infant/young child (1-59 months), older child (5-17 years), and adults (> 18 years). We will stratify disease based on clinical diagnosis and severity using standardized case definitions where these exist. The clinical criteria for defining diseases are likely to vary across studies. For example, pneumonia in some studies may be defined by chest radiography while in other studies pneumonia may be defined by tachypnea alone. We will compare reported case definitions to standardized global guidelines (e.g., WHO guidelines) and combine data from studies using comparable case definitions as much as possible. We will classify altitude as high (≥ 1500 m above sea level) and low altitude (< 1500 m above sea level).
We will use a random-effects meta-analysis to obtain a point prevalence of hypoxemia (95% confidence interval), pooling together all studies, by age, clinical diagnosis and severity, health facility type, and high/low altitude. The calculated point prevalence of hypoxemia will represent an average of distributions rather an estimate of a one true prevalence. We expect a moderate-high degree of heterogeneity between studies. Depending on the number of available studies, we will attempt to reconcile some of these differences by calculating point prevalence for more targeted subgroups—e.g., prevalence of hypoxemia in 1-59 month old children for severe pneumonia in secondary or tertiary facilities. We will determine the I2 value (index of the proportion of total variation across studies that is due to heterogeneity rather than to chance) for each estimate of prevalence as an indication of the between-study heterogeneity. If the point-prevalence by the described analysis is likely to be misleading due to irreconcilable heterogeneity between included studies, we will present these results as the medians and inter-quartile ranges of the proportion of hypoxemic children in the studies within each subgroup.
Discussion
Hypoxemia is a critical condition and understanding the burden of hypoxemia may support decision-making in LMICs to deploy pulse oximeters and oxygen treatments more efficiently to address diseases and patient populations with the highest burden. Previous studies on hypoxemia prevalence have focused too narrowly on a few diseases or specific patient populations (e.g., pneumonia in children under five) whereas any effort to improve access to oxygen requires understanding of the potential demand for oxygen for all diseases and population groups. This study aims to fill that gap by providing comprehensive estimates of hypoxemia prevalence. Furthermore, governments, UN agencies, donors, and NGOs are investing strongly to improve oxygen systems in LMICs. Effective oxygen system planning requires estimation of oxygen need, informed by robust data on hypoxemia prevalence and admission patterns at all the levels of the health system. Currently, the lack of quality data on hypoxemia prevalence is compromising efforts to predict oxygen needs and efficiently plan scale up of pulse oximetry and oxygen systems.
Limitations of this study are that pulse oximetry is not widely used in low-resource settings and while it is used in clinical research, pulse oximetry results are often not reported as a primary outcome of the study. We aim to mitigate this limitation by contacting study authors to obtain data for re-analysis. A key logistical factor in the study’s success will be the cooperation of those authors.
Availability of data and materials
Not applicable
Abbreviations
- ALRI:
-
Acute lower respiratory infection
- COPD:
-
Chronic obstructive pulmonary disorder
- HIV:
-
Human immunodeficiency virus
- LMIC:
-
Low- and middle-income countries
- MAM:
-
Moderate acute malnutrition
- PaO2 :
-
Partial pressure of arterial oxygen
- PJP:
-
Pneumocystis pneumonia
- PPH:
-
Post-partum hemorrhage
- RDS:
-
Respiratory distress syndrome
- SAM:
-
Severe acute malnutrition
- SpO2 :
-
Peripheral oxygen saturation
- WHO:
-
World Health Organization
References
Lazzerini M, Sonego M, Pellegrin MC. Hypoxaemia as a mortality risk factor in acute lower respiratory infections in children in low and middle-income countries: systematic review and meta-analysis. PLoS One. 2015;10(9):e0136166.
Orimadegun A, Ogunbosi B, Orimadegun B. Hypoxemia predicts death from severe falciparum malaria among children under 5 years of age in Nigeria: the need for pulse oximetry in case management. Afr Health Sci. 2014;14(2):397–407.
Garde A, Zhou G, Raihana S, Dunsmuir D, Karlen W, Dekhordi P, et al. Respiratory rate and pulse oximetry derived information as predictors of hospital admission in young children in Bangladesh: a prospective observational study. BMJ Open. 2016;6(8):e011094.
Wells JM, Estepar RS, McDonald MN, Bhatt SP, Diaz AA, Bailey WC, et al. Clinical, physiologic, and radiographic factors contributing to development of hypoxemia in moderate to severe COPD: a cohort study. BMC Pulm Med. 2016;16(1):169.
Oldenburg O, Wellmann B, Buchholz A, Bitter T, Fox H, Thiem U, et al. Nocturnal hypoxaemia is associated with increased mortality in stable heart failure patients. Eur Heart J. 2016;37(21):1695–703.
Vold ML, Aasebo U, Wilsgaard T, Melbye H. Low oxygen saturation and mortality in an adult cohort: the Tromso study. BMC Pulm Med. 2015;15:9.
Belle J, Cohen H, Shindo N, Lim M, Velazquez-Berumen A, Ndihokubwayo JB, et al. Influenza preparedness in low-resource settings: a look at oxygen delivery in 12 African countries. J Infect Dev Ctries. 2010;4(7):419–24.
Ginsburg AS, Van Cleve WC, Thompson MI, English M. Oxygen and pulse oximetry in childhood pneumonia: a survey of healthcare providers in resource-limited settings. J Trop Pediatr. 2012;58(5):389–93.
Subhi R, Adamson M, Campbell H, Weber M, Smith K, Duke T, et al. The prevalence of hypoxaemia among ill children in developing countries: a systematic review. Lancet Infect Dis. 2009;9(4):219–27.
World Health Organization. Oxygen therapy for children: a manual for health workers. 2016.
The World Bank. World Bank list of economies Washington, DC: The World Bank; 2018 [updated June 2018. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/378834-how-does-the-world-bank-classify-countries.
Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13(3):147–53.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Acknowledgements
The authors would like to acknowledge Poh Chua, Royal Children’s Hospital Research Librarian, with assistance in designing and conducting electronic database search for this review.
Funding
The authors have received funding from the Bill and Melinda Gates Foundation and IKEA Foundation to support the authors’ time to conduct the study. The funders are not involved in any other aspect of the project, such as the design of the project’s protocol and analysis plan, the collection and analyses. The funders will have no input on the interpretation or publication of the study results.
Author information
Authors and Affiliations
Contributions
HG is the guarantor. FL drafted the manuscript. All authors contributed to the development of the selection criteria, the risk of bias assessment strategy, and data extraction criteria. RS and HG developed the search strategy. All authors read, provided feedback, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received non-human subject research determination by Advarra IRB in the USA (Pro000034171) and was determined to be exempt from ethical approval by the Royal Children’s Hospital Human Research Ethics Committee (HREC), Melbourne, Australia (29 May 2019).
Consent for publication
Not applicable
Competing interests
FL, JH, KS, and AB are receiving funding from the Bill and Melinda Gates Foundation and IKEA Foundation for projects related to improving access to pulse oximetry and oxygen for hypoxemia. HG is receiving funding from the Bill and Melinda Gates Foundation for projects related to pulse oximetry and oxygen therapy.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lam, F., Subhi, R., Houdek, J. et al. The prevalence of hypoxemia among pediatric and adult patients presenting to healthcare facilities in low- and middle-income countries: protocol for a systematic review and meta-analysis. Syst Rev 9, 67 (2020). https://doi.org/10.1186/s13643-020-01326-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-020-01326-5