Abstract
Background
Titration of the continuous distending pressure during a staircase incremental–decremental pressure lung volume optimization maneuver in children on high-frequency oscillatory ventilation is traditionally driven by oxygenation and hemodynamic responses, although validity of these metrics has not been confirmed.
Methods
Respiratory inductance plethysmography values were used construct pressure–volume loops during the lung volume optimization maneuver. The maneuver outcome was evaluated by three independent investigators and labeled positive if there was an increase in respiratory inductance plethysmography values at the end of the incremental phase. Metrics for oxygenation (SpO2, FiO2), proximal pressure amplitude, tidal volume and transcutaneous measured pCO2 (ptcCO2) obtained during the incremental phase were compared between outcome maneuvers labeled positive and negative to calculate sensitivity, specificity, and the area under the receiver operating characteristic curve. Ventilation efficacy was assessed during and after the maneuver by measuring arterial pH and PaCO2. Hemodynamic responses during and after the maneuver were quantified by analyzing heart rate, mean arterial blood pressure and arterial lactate.
Results
41/54 patients (75.9%) had a positive maneuver albeit that changes in respiratory inductance plethysmography values were very heterogeneous. During the incremental phase of the maneuver, metrics for oxygenation and tidal volume showed good sensitivity (> 80%) but poor sensitivity. The sensitivity of the SpO2/FiO2 ratio increased to 92.7% one hour after the maneuver. The proximal pressure amplitude showed poor sensitivity during the maneuver, whereas tidal volume showed good sensitivity but poor specificity. PaCO2 decreased and pH increased in patients with a positive and negative maneuver outcome. No new barotrauma or hemodynamic instability (increase in age-adjusted heart rate, decrease in age-adjusted mean arterial blood pressure or lactate > 2.0 mmol/L) occurred as a result of the maneuver.
Conclusions
Absence of improvements in oxygenation during a lung volume optimization maneuver did not indicate that there were no increases in lung volume quantified using respiratory inductance plethysmography. Increases in SpO2/FiO2 one hour after the maneuver may suggest ongoing lung volume recruitment. Ventilation was not impaired and there was no new barotrauma or hemodynamic instability. The heterogeneous responses in lung volume changes underscore the need for monitoring tools during high-frequency oscillatory ventilation.
Similar content being viewed by others
Background
Preventing ventilator-induced lung injury (VILI) is one of the many challenges when ventilating critically ill children, especially since the exact underlying mechanisms and consequences in pediatrics are far from understood [1]. Little pediatric evidence supports best ventilation practices that can be applied to attenuate the detrimental effects of two key factors of VILI, being atelectrauma [the repetitive opening and closure of alveoli] and volutrauma [the delivery of large tidal volume (Vt) in relation to the amount of inflatable lung volume]. From a theoretical perspective, high-frequency oscillatory ventilation (HFOV) is an ideal mode for lung-protective ventilation given its delivery of very small stroke volumes and pressure changes at the alveolar level while preserving end-expiratory lung volume (EELV).
Pediatric critical care practitioners have embraced HFOV for the management of acute respiratory failure, despite the outcome of the only pediatric randomized clinical trial (RCT) failing to show benefit on patient outcome [2]. Also, continued use became controversial following the publication of two clinical trials in adult ARDS in 2013 [3, 4]. Whereas patient outcomes including all-cause mortality were similar in the Oscillation for ARDS (OSCAR) trial, the High Frequency Oscillation for Early ARDS (OSCILLATE) trial was stopped prematurely because of increased mortality among those randomized to HFOV [3, 4]. However, the question is whether the outcomes of these studies confirmed that HFOV was not beneficial or even harmful, or if it was a matter of how the oscillator was used that determined patient outcomes [5, 6]. For example, most adult and pediatric observational studies not reported using lung volume optimization maneuvers (LVOM). Nonetheless, experimental work underscored the importance of recruiting lung volume when transitioning to HFOV because not only oxygenation improves with more recruited lung volume, but also to prevent collapsed, atelectatic lung units from becoming exposed to larger, potentially more injurious pressure swings [7, 8]. However, the best lung volume optimization maneuver has yet to be identified both in children and adults [9].
One approach to a lung volume optimization maneuver is the staircase incremental–decremental pressure titration [10,11,12]. Since it has been proposed that oxygenation improves linearly with increases in lung volume during HFOV, the transcutaneous measured oxygen saturation (SpO2) in relation to the delivered oxygen fraction (FiO2) drives the pressure titration. In addition, the proximal pressure amplitude is monitored during the maneuver because it may be used as a marker of respiratory system compliance. Lastly, a decrease in blood pressure may be interpreted as sign of lung overdistension [9]. The unanswered question is how reliable these variables are to identify the onset of lung volume recruitment and lung overdistension [13, 14]. Recently, we reported that changes in the cross-sectional area of the chest wall and the abdominal compartment measured with respiratory inductance plethysmography (RIP) may act as indicator for lung volume changes during a lung volume optimization maneuver [15]. The present efficacy and safety study builds on our pilot work. We sought to explore how changes in metrics for oxygenation (SpO2 and FiO2), proximal pressure amplitude and tidal volume reflected changes in lung volume during and after the lung volume optimization maneuver (efficacy). Next, we sought to study the effect of the lung volume optimization maneuver on CO2 clearance, occurrence of hemodynamic instability and development of new barotrauma (safety).
Methods
Study population
We collected data during the lung volume optimization maneuver in children after the indication for HFOV was set by the attending physician in agreement with the clinical guideline [10]. Children were enrolled after written informed consent from either parents or legal caretakers if they had acute onset of lung disease and were on neuromuscular paralysis. Children with a gestational age < 40 weeks, with congenital or acquired paralysis of the diaphragm, uncorrected congenital heart disorder, severe pulmonary hypertension or open thorax or abdomen after surgery and those with status asthmaticus were excluded. The Institutional Review Board of the hospital approved the study. PARDS was defined as previously described [16].
HFOV lung volume optimization strategy
Initial oscillator settings irrespective of age or bodyweight included frequency 10–12 Hz, continuous distending pressure 3–5 cm H2O above mean airway pressure (mPaw) on conventional mechanical ventilation (CMV), power setting targeting 70–90 cmH2O proximal pressure amplitude, inspiratory time 33% and bias flow 20–40 L/min. Immediately after transitioning to HFOV using the SensorMedics 3100A/B oscillator (SensorMedics, Yorba Linda, CA), a quasi-static lung volume optimization maneuver was performed by an individualized staircase incremental–decremental pressure titration, allowing to map the pressure–volume (PV) relationship. Briefly, the inflation limb was mapped by increasing pressure 2 cmH2O every 3–5 min with ongoing oscillations while simultaneously monitoring the SpO2 and mean arterial blood pressure, identifying the onset of lung recruitment (i.e., increase in SpO2) until no further improvement in oxygenation and/or sudden decrease in mean arterial blood pressure during two consecutive pressure increments. Subsequently, the pressure was stepwise decreased every 3–5 min by 2 cm H2O until the SpO2 decreased again indicating lung derecruitment or when other clinical situations gave rise to stop decreasing the pressure. Frequency and power remained constant, so that the proximal pressure amplitude could reflect changes in respiratory system compliance. Only in patients with severe increasing hypercapnia resulting in acidosis (pH < 7.25), frequency was lowered during the maneuver [10].
Measurements and data acquisition
Mean arterial blood pressure (Edwards Lifesciences, Irvine, CA, USA), SpO2 (Masimo Corporation, Irvine, CA, USA), transcutaneous CO2 (Radiometer, Brønshøj, Denmark) and tidal volume were continuously measured during the maneuver. Continuous distending pressure and proximal pressure amplitude were read from the oscillator. Arterial blood samples were taken to measure PaCO2, pH and lactate before and 1 h after the maneuver (Radiometer, Brønshøj, Denmark). Tidal volume was measured using an inline hot wire flow sensor (Acutronic, Hirzel, Switzerland). Respiratory inductance plethysmography signals were sampled at 200 Hz using two elastic bands (Nox Medical, Reykjavik, Iceland) connected to the Bicore II™ (Vyaire, Yorba Linda, Ca, USA) and stored for offline analysis. Uncalibrated signals were derived from the chest and abdominal respiratory inductance plethysmography signals. Data acquisition was done using a custom-built Polybench software module (Applied Biosignals, Weener, Germany).
Data analysis
All data analyses were done offline. First, to study how changes in metrics for oxygenation (SpO2 and FiO2), proximal pressure amplitude and tidal volume reflected changes in lung volume during the lung volume optimization maneuver, we normalized the continuous distending pressure by setting the pressure at which the maneuver started (initial and lowest pressure) at 0% and the last (highest) pressure during the incremental phase of the maneuver at 100%. We calculated mean respiratory inductance plethysmography signals (chest, abdomen and sum) from a 30-s artifact-free period just before the next increase in pressure allowing for lung volume equilibration, using a custom-built Polybench software module (Applied Biosignals, Weener, Germany). These values were then plotted against the normalized pressure to map the pressure–volume relationship according to the four-parameter logistic Venegas equation provided that enough data points were available to plot [17]. The lung volume optimization maneuver was labeled responsive if there was an increase in respiratory inductance plethysmography signal during the incremental phase as we previously have done [15]. Then, we plotted tidal volume against pressure using the four-parameter logistic Venegas equation [17]. SpO2, SpO2/FiO2, proximal pressure amplitude and the transcutaneous pCO2 were also plotted against pressure. Subsequently, three independent pediatric clinician-researchers (PdJ, RB, MK) classified these plots positive (i.e., improvement in SpO2 and/or SpO2/FiO2 ratio, tidal volume, decrease in proximal pressure amplitude) or negative by visual inspection. Intraclass correlation coefficient (ICC) Fleiss kappa was calculated to evaluate the agreement between investigators.
Next, we wanted to study the time course of the SpO2/FiO2 ratio, proximal pressure amplitude, tidal volume, PaCO2, pH and changes in mean arterial blood pressure and arterial lactate by comparing four time points: just before transitioning to high-frequency oscillatory ventilation (T0), at the end of the incremental phase when there was the highest applied pressure (T1), at the last applied pressure during the decremental phase (T2) and 1 h (T3) after the maneuver. For analytical purposes, we compared the number of patients with arterial blood lactate > 2 mmol/L and mean arterial blood pressure lower than the age-adjusted p10 or ≥ p90.
Statistical analyses
The primary endpoint was sensitivity and specificity of metrics for oxygenation, proximal pressure amplitude and tidal volume to reflect lung volume changes during the maneuver. Secondary endpoints included the time course of the SpO2/FiO2 ratio, proximal pressure amplitude and tidal volume from baseline to 1 h after the maneuver, effects of the maneuver on ventilation parameters (PaCO2 and pH), occurrence of hemodynamic instability and development of new barotrauma. Continuous data are presented as median and 25–75 interquartile range (IQR) and absolute numbers as percentage of total. Continuous paired data were tested using the Wilcoxon signed rank test and comparisons between groups with the Mann–Whitney U test. Dichotomous variables were tested with the χ2 test or the Fisher exact test if values were < 5. Sensitivity and specificity were calculated for all plots and the SpO2/FiO2 ratio at T2 and T3. P values less than 0.05 were accepted as statistically significant.
Results
Patient characteristics
Fifty-two patients completed the maneuver, with two patients having two separate HFOV runs in different ventilation periods (Table 1). Primary admission diagnosis was acute respiratory failure in 48 patients, tracheal rupture in one and sepsis in the remaining five. All but ten patients met PARDS criteria. Baseline SpO2/FiO2 ratio of the whole cohort was 190 (121–243). Median CMV settings prior to HFOV were peak inspiratory pressure (PIP) 31 cmH2O (30–34), PEEP 8 cmH2O (6–8) and FiO2 0.5 (0.4–0.76).
The median highest pressure at the end of the incremental phase of the maneuver after a median number of incremental steps of 8 (7–9) was 34 (32–36) cmH2O (Additional file 1: Table S1). The maneuver was labeled responsive in 41 patients (75.9%) by the three independent reviewers (Fleiss’ kappa 0.967). Pooled data plotted according to Venegas did not show a clear overall lower and upper inflection point (Additional file 2: Figure S1).
SpO 2 /FiO 2 ratio, proximal pressure amplitude and tidal volume as predictor for lung volume changes during the maneuver
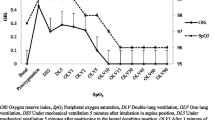
Table 2 summarizes the number of plots labeled positive or negative by visual inspection stratified by lung volume optimization maneuver outcome (i.e., responsive, or unresponsive). Metrics for oxygenation (i.e., the SpO2–pressure and/or SpO2/FiO2–pressure plot showed a high sensitivity of 87.8%, but the sensitivity was 53.8% and there was disagreement among the three independent reviewers (Fleiss’ kappa 0.431). Heterogeneity in the pooled SpO2/FiO2 ratio for a given normalized pressure during the incremental (Fig. 1a, b) and decremental phase (Fig. 1c, d) of the maneuver stratified by outcome reflected the mediocre negative predictive value of 58.3%. Proximal pressure amplitude (negative predictive value 25.6%) or tidal volume (negative predictive value 20.0%) showed even lower negative predictive values.
Pooled SpO2/FiO2 ratio for a given continuous distending pressure (CDP) normalized from 0 to 100% during the lung volume optimization maneuver incremental phase stratified by outcome, i.e., responsive (panel A and B, N = 41) or unresponsive (panel C and D, N = 13). Data are presented as median and 25–75 interquartile range
Time course of SpO 2 /FiO 2 ratio, proximal pressure amplitude and tidal volume
Except for pressure at the end of the incremental phase or at the end of the lung volume optimization maneuver, oscillator settings remained constant over time, (Additional file 1: Table S1). For the whole cohort the median SpO2/FiO2 ratio increased from 190 (121–243) before the maneuver to 240 (167–324) 1 h after the maneuver (p < 0.001). Significant improvements in SpO2/FiO2 ratio were observed in responsive and unresponsive lung volume optimization maneuvers (Table 3). Sensitivity, specificity, and positive and negative predictive value of SpO2/FiO2 were better one hour after the lung volume optimization maneuver (Table 2). Tidal volume, but not the proximal pressure amplitude did not significantly change over time, irrespective of lung volume optimization maneuver outcome (Table 3). Strong heterogeneity in tidal volume changes during the incremental and decremental phase of the lung volume optimization maneuver was observed (Additional file 3: Figure S2).
Safety of the lung volume optimization maneuver
The overall median arterial pH improved from 7.30 (7.23–7.35) before the maneuver to 7.38 (7.32–7.45, p < 0.001) 1 h after the maneuver. We also observed improvements in pCO2 from (58 (52–64) before the maneuver to 46 (36–53) mmHg, p < 0.001) 1 h after the maneuver. Significant changes were observed irrespective of lung volume optimization maneuver outcome (Additional file 4: Table S2). No new barotrauma or hemodynamic instability occurred (Additional file 5: Table S3). Fifteen (27.8%) patients received a fluid bolus during the maneuver.
Discussion
This study is one of the first studies to characterize physiologic responses to a lung volume optimization maneuver during pediatric high-frequency oscillatory ventilation. We confirmed our previous preliminary observations that clinical variables used at the bedside to identify changes in lung volume correlated poorly with lung volume changes measured using respiratory inductance plethysmography [15]. We also report that an individual staircase lung volume optimization maneuver was safe and did not negatively impact CO2 elimination.
Optimization of lung volume after switching to HFOV is necessary to minimize lung injury and to allow for a better dampening of the pressure swings as well as oscillation on the deflation limb of the pressure–volume loop where there is less continuous alveolar recruitment and derecruitment [7, 18,19,20]. Despite this physiologic rationale, there is very little data regarding the optimal lung volume optimization maneuver except for one neonatal lamb model study comparing a staircase CDP titration with (repeated) sustained inflations (SI) [11]. A stepwise CDP increase produced the greatest increase in lung volume and resolution of atelectasis compared with a 20-s SI (either once or repeated 6 times) or a standard approach (i.e., randomly setting the CDP) [11]. SIs have been studied in relevant animal models, but no comparisons were made with other lung volume optimization maneuvers [21, 22]. By using a staircase incremental CDP titration, we observed a highly variable response to titration among the studied patients. Many studied patients showed a lung volume increase and individual lower (LIP) and upper inflection points (UIP) identified, but there was no clear overall LIP or UIP point during the inflation phase of the lung volume optimization maneuver (Fig. 1). Even though our study was not designed to identify the best lung volume optimization maneuver, the heterogeneity that we observed may put the lung volume optimization maneuver used in the OSCILLATE trial in a different perspective. In that trial, a SI of 40 cmH2O for 40 s was used, but it can be argued that such a standardized, non-individualized lung volume optimization maneuver may have led to either lung overdistension or poorly recruited alveoli contributing to poor patient outcome [3, 5, 6]. We also observed heterogeneity during the deflation phase (Additional file 2: Figure S1), questioning if routinely reducing the CDP to a certain level to find the sweet spot of ventilation as was done in the OSCILLATE trial is justified. Our data underscore the need for further studies into the most optimal lung volume optimization maneuver.
The uncertainty about lung volume optimization maneuver is further fueled by the fact that it is unclear how to bedside monitor changes in lung volume. Traditionally, clinical parameters such as SpO2, OI and PaO2/FiO2 are used to monitor changes in lung volume [13, 14]. Preliminary experimental and clinical work in neonates supported the possibility of monitoring lung volume changes during HFOV with respiratory inductance plethysmography [12, 23,24,25]. Respiratory inductance plethysmography is a validated, noninvasive respiratory monitoring technique used as proxy for changes in lung volume by quantifying changes in the cross-sectional area of the chest wall and the abdominal compartment [26, 27]. Previously, we also reported that RIP may be of additional value during pediatric HFOV [15]. In our present study, we found that oxygenation improved not only in responsive, but also unresponsive lung volume optimization maneuvers, challenging if oxygenation is a good bedside marker for lung volume changes as also has been observed during CMV [28, 29]. It has also been proposed that a decrease in blood pressure might be perceived as sign of lung overdistension and may thus be used as a parameter guiding the lung volume optimization maneuver. In line with our previously reported pilot data, we very infrequently observed this phenomenon [15]. It can also be argued that we did not fully recruit the lung, hence explaining our failure to observe a decrease in blood pressure and even suggesting potential for delivering a higher CDP during the lung volume optimization maneuver. However, it has never been studied if a heterogeneous diseased lung should be recruited up to the point of a decrease in blood pressure, as the inherent risk is that some areas may be already overdistended at even low airway pressures [30, 31].
Traditionally, HFOV decouples oxygenation and ventilation. However, we observed an improvement in pCO2 and pH one hour post lung volume optimization maneuver, irrespective of the response status or changes in F. Also, changes in tidal volume were seen in both responsive and unresponsive lung volume optimization maneuvers. Our findings may be interpreted as that HFOV may exert also positive effects not only on oxygenation, but also ventilation.
Our study may have two clinical implications. First, we observed that oxygenation improved further after the lung volume optimization maneuver, yielding a better sensitivity and specificity compared with oxygenation immediately post lung volume optimization maneuver. The significant decrease in proximal pressure amplitude without changes in oscillatory power in responsive lung volume optimization maneuvers suggests an ongoing improvement in lung compliance post maneuver. Hence, we postulate that the clinical assessment of whether the lung volume optimization maneuver was successful should be done in the hours following the maneuver. Second, the staircase lung volume optimization maneuver was safe in both responsive and unresponsive lung volume optimization maneuvers as there was no significant hypercapnia despite using a high frequency nor did it lead to hemodynamic impairment or new barotrauma.
The strength of this study is that it is the first clinical pediatric study characterizing the lung volume optimization maneuver during HFOV coming from a high-volume HFOV unit, reporting limited applicability of traditionally used clinical variables and safety and feasibility of a staircase, personalized lung volume optimization maneuver. However, there are also several limitations that need to be discussed. First, as our study was a single-center study, this may limit the generalizability of our findings. The study cohort was an inhomogeneous population with different causes and stages of the lung disease and different degrees of PARDS. However, we are confident that this does not reduce the validity of the data. Second, we measured changes in respiratory inductance plethysmography as proxy of lung volume changes. Validation against any other lung imaging technique such as CT or electrical impedance tomography (EIT) may be necessary because the respiratory inductance plethysmography signal does not distinguish between global changes in lung and thoracic blood volume [23, 27]. Nonetheless, respiratory inductance plethysmography has been shown to estimate mean lung volume changes during HFOV and the lack of cardiovascular instability observed in our study suggests that most (if not all) of the respiratory inductance plethysmography changes were due to changes in thoracic gas volume [23, 32, 33]. Lastly, we did not a priori define how much the respiratory inductance plethysmography signal needed to improve to be labeled as responsive lung volume optimization maneuver when mapping these against pressure. Again, this requires comparison with other measures of lung volume change such as EIT or CT.
Conclusions
Clinically used bedside variables commonly used during a lung volume optimization maneuver with pediatric HFOV correlate poorly with lung volumes changes measured using respiratory inductance plethysmography. A personalized staircase lung volume optimization maneuver does not cause hemodynamic impairment or negatively impacts CO2 elimination. Further studies are necessary to compare the maneuver with other maneuvers and study the effect of a respiratory inductance plethysmography-guided maneuver on patient outcome.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- CDP:
-
Continuous distending pressure
- CDPhyperinflation :
-
CDP point representing the onset of hyperinflation
- CDPrecruitment :
-
CDP point representing the onset of lung recruitment
- CMV:
-
Conventional mechanical ventilation
- EELV:
-
End-expiratory lung volume
- EIT:
-
Electrical impedance tomography
- F:
-
Frequency
- FiO2:
-
Delivered oxygen fraction
- HFOV:
-
High-frequency oscillatory ventilation
- ICC:
-
Intraclass correlation coefficient
- IQR:
-
Interquartile range
- LIP:
-
Lower inflection point
- LVOM:
-
Lung volume optimization maneuver
- mABP:
-
Mean arterial blood pressure
- mPaw:
-
Mean airway pressure
- MV:
-
Mechanical ventilation
- OI:
-
Oxygenation index
- PARDS:
-
Pediatric acute respiratory distress syndrome
- PEEP:
-
Positive end-expiratory pressure
- PIP:
-
Peak inspiratory pressure
- ΔPproximal :
-
Proximal pressure amplitude
- PRISM:
-
Pediatric risk of mortality
- ptcCO2 :
-
Transcutaneous measured pCO2
- P–V:
-
Pressure–volume (PV)
- RCT:
-
Randomized clinical trial
- RIP:
-
Respiratory inductance plethysmography
- SI:
-
Sustained inflations
- SpO2 :
-
Transcutaneous measured oxygen saturation
- T0:
-
Time point just before transitioning to HFOV
- T1:
-
Time point at the highest applied CDP at the end of the incremental phase
- T2:
-
Time point at the last applied CDP during the decremental phase
- T3:
-
Time point 1 h after the LVOM
- UIP:
-
Upper inflection point
- VILI:
-
Ventilator-induced lung injury
- V t :
-
Tidal volume
References
Kneyber MC, Zhang H, Slutsky AS. Ventilator-induced lung injury: similarity and differences between children and adults. Am J Respir Crit Care Med. 2014;190(3):258–65.
Arnold JH, Hanson JH, Toro-Figuero LO, Gutierrez J, Berens RJ, Anglin DL. Prospective, randomized comparison of high-frequency oscillatory ventilation and conventional mechanical ventilation in pediatric respiratory failure. Crit Care Med. 1994;22(10):1530–9.
Ferguson ND, Cook DJ, Guyatt GH, Mehta S, Hand L, Austin P, Zhou Q, Matte A, Walter SD, Lamontagne F, et al. High-frequency oscillation in early acute respiratory distress syndrome. N Engl J Med. 2013;368(9):795–805.
Young D, Lamb SE, Shah S, MacKenzie I, Tunnicliffe W, Lall R, Rowan K, Cuthbertson BH, Group OS. High-frequency oscillation for acute respiratory distress syndrome. N Engl J Med. 2013;368(9):806–13.
Kneyber MC, Markhorst DG. Do we really know how to use high-frequency oscillatory ventilation in critically Ill children? Am J Respir Crit Care Med. 2016a;193(9):1067–8.
Kneyber MC, Markhorst DG. Any trial can (almost) kill a good technique. Intensive Care Med. 2016b;42(6):1092–3.
Pillow JJ. High-frequency oscillatory ventilation: mechanisms of gas exchange and lung mechanics. Crit Care Med. 2005;33(3 Suppl):S135–41.
Suzuki H, Papazoglou K, Bryan AC. Relationship between PaO2 and lung volume during high frequency oscillatory ventilation. Acta Paediatr Jpn. 1992;34(5):494–500.
Kneyber MC, van Heerde M, Markhorst DG. Reflections on pediatric high-frequency oscillatory ventilation from a physiologic perspective. Respir Care. 2012;57(9):1496–504.
de Jager P, Kamp T, Dijkstra SK, Burgerhof JGM, Markhorst DG, Curley MAQ, Cheifetz IM, Kneyber MCJ. Feasibility of an alternative, physiologic, individualized open-lung approach to high-frequency oscillatory ventilation in children. Ann Intensive Care. 2019;9(1):9.
Pellicano A, Tingay DG, Mills JF, Fasulakis S, Morley CJ, Dargaville PA. Comparison of four methods of lung volume recruitment during high frequency oscillatory ventilation. Intensive Care Med. 2009;35(11):1990–8.
Miedema M, de Jongh FH, Frerichs I, van Veenendaal MB, van Kaam AH. Changes in lung volume and ventilation during lung recruitment in high-frequency ventilated preterm infants with respiratory distress syndrome. J Pediatr. 2011;159(2):199-205.e192.
Goffi A, Ferguson ND. High-frequency oscillatory ventilation for early acute respiratory distress syndrome in adults. Curr Opin Crit Care. 2014;20(1):77–85.
Ng J, Ferguson ND. High-frequency oscillatory ventilation: still a role? Curr Opin Crit Care. 2017. https://doi.org/10.1097/MCC.0000000000000387.
de Jager P, Burgerhof JGM, Koopman AA, Markhorst DG, Kneyber MCJ. Lung volume optimization maneuver responses in pediatric high frequency oscillatory ventilation. Am J Respir Crit Care Med. 2019. https://doi.org/10.1164/rccm.201809-1769L.
Khemani RG, Smith LS, Zimmerman JJ, Erickson S. Pediatric Acute Lung Injury Consensus Conference G: Pediatric acute respiratory distress syndrome: definition, incidence, and epidemiology: proceedings from the pediatric acute lung injury consensus conference. Pediatr Crit Care Med. 2015;16(5 Suppl 1):S23-40.
Venegas JG, Harris RS, Simon BA. A comprehensive equation for the pulmonary pressure-volume curve. J Appl Physiol. 1998;84(1):389–95.
Froese AB, Kinsella JP. High-frequency oscillatory ventilation: lessons from the neonatal/pediatric experience. Crit Care Med. 2005;33(3 Suppl):S115-121.
McCulloch PR, Forkert PG, Froese AB. Lung volume maintenance prevents lung injury during high frequency oscillatory ventilation in surfactant-deficient rabbits. Am Rev Respir Dis. 1988;137(5):1185–92.
Bond DM, Froese AB. Volume recruitment maneuvers are less deleterious than persistent low lung volumes in the atelectasis-prone rabbit lung during high-frequency oscillation. Crit Care Med. 1993;21(3):402–12.
Muellenbach RM, Kredel M, Zollhoefer B, Wunder C, Roewer N, Brederlau J. Sustained inflation and incremental mean airway pressure trial during conventional and high-frequency oscillatory ventilation in a large porcine model of acute respiratory distress syndrome. BMC Anesthesiol. 2006;6:8.
Byford LJ, Finkler JH, Froese AB. Lung volume recruitment during high-frequency oscillation in atelectasis-prone rabbits. J Appl Physiol (1985). 1988;64(4):1607–14.
Brazelton TB 3rd, Watson KF, Murphy M, Al-Khadra E, Thompson JE, Arnold JH. Identification of optimal lung volume during high-frequency oscillatory ventilation using respiratory inductive plethysmography. Crit Care Med. 2001;29(12):2349–59.
Tingay DG, Mills JF, Morley CJ, Pellicano A, Dargaville PA. Indicators of optimal lung volume during high-frequency oscillatory ventilation in infants. Crit Care Med. 2013;41(1):237–44.
van der Burg PS, Miedema M, de Jongh FH, Frerichs I, van Kaam AH. Cross-sectional changes in lung volume measured by electrical impedance tomography are representative for the whole lung in ventilated preterm infants. Crit Care Med. 2014;42(6):1524–30.
Valta P, Takala J, Foster R, Weissman C, Kinney JM. Evaluation of respiratory inductive plethysmography in the measurement of breathing pattern and PEEP-induced changes in lung volume. Chest. 1992;102(1):234–8.
Markhorst DG, Van Gestel JP, Van Genderingen HR, Haitsma JJ, Lachmann B, Van Vught AJ. Respiratory inductive plethysmography accuracy at varying PEEP levels and degrees of acute lung injury. J Med Eng Technol. 2006;30(3):166–75.
Caironi P, Gattinoni L. How to monitor lung recruitment in patients with acute lung injury. Curr Opin Crit Care. 2007;13(3):338–43.
Laviola M, Rafl J, Rozanek M, Kudrna P, Roubik K. Models of PaO2 response to the continuous distending pressure maneuver during high frequency oscillatory ventilation in healthy and ARDS lung model pigs. Exp Lung Res. 2016;42(2):87–94.
Grune J, Tabuchi A, Kuebler WM. Alveolar dynamics during mechanical ventilation in the healthy and injured lung. Intensive Care Med Exp. 2019;7(Suppl 1):34–34.
Del Sorbo L, Tonetti T, Ranieri VM. Alveolar recruitment in acute respiratory distress syndrome: should we open the lung (no matter what) or may accept (part of) the lung closed? Intensive Care Med. 2019;45(10):1436–9.
Gothberg S, Parker TA, Griebel J, Abman SH, Kinsella JP. Lung volume recruitment in lambs during high-frequency oscillatory ventilation using respiratory inductive plethysmography. Pediatr Res. 2001;49(1):38–44.
Brazelton TB, Watson KF, Thompson JE, Arnold JH. Bench validation of respiratory inductive plethysmography in determining the end-expiratory lung volume during high frequency ventilation. Pediatr Res. 1999;45(4):37a–37a.
Acknowledgements
The authors would like to thank Sandra K. Dijkstra, RN, for her help in collecting the clinical data.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
PdJ collected the data, performed the analyses and wrote the first draft of the manuscript. JGMB and DM provided intellectual content to the manuscript. AK contributed to the data analyses. MK conceived and supervised the study and is accountable for accuracy and integrity of the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Children were enrolled after written informed consent from either parents or legal caretakers in line with the Helsinki declaration. The Institutional Review Board of the University Medical Center Groningen approved the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1:
Table S1. Oscillator settings at start of the lung volume optimization maneuver, at the end of the incremental phase, at the end of the decremental phase and one hour after completion of the maneuver.
Additional file 2:
Figure S1. Pooled changes in respiratory inductance plethysmography (RIP) measured during the lung volume optimization maneuver for a given continuous distending pressure (CDP) (normalized from 0 to 100%).
Additional file 3:
Figure S2. Pooled changes in tidal volume (Vt) measured during the lung volume optimization maneuver for a given continuous distending pressure (CDP) (normalized from 0 to 100%) fitted according to Venegas for the incremental phase and decremental phase.
Additional file 4:
Table S2. Summary of changes in PaCO2 and pH.
Additional file 5:
Table S3. Comparison between the number of patients with hemodynamic instability and new barotrauma before and after the lung volume optimization maneuver.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Jager, P., Burgerhof, J.G.M., Koopman, A.A. et al. Physiologic responses to a staircase lung volume optimization maneuver in pediatric high-frequency oscillatory ventilation. Ann. Intensive Care 10, 153 (2020). https://doi.org/10.1186/s13613-020-00771-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-020-00771-8