Abstract
Background
Although outcomes of critically ill patients with haematological malignancies (HMs) have been fully investigated in terms of organ failure and mortality, data are scarce on health-related quality of life (HRQOL) in this population. We aim to assess post-intensive care unit (ICU) burden and HRQOL of critically ill patients with HMs and to identify risk factors for quality-of-life (QOL) impairment.
Results
In total, 1011 patients with HMs who required ICU admission in 17 ICUs in France and Belgium were included in the study; 278 and 117 patients were evaluated for QOL at 3 months and 1 year, respectively, after ICU discharge. HRQOL was determined by applying the interview form of the Short Form 36 (SF-36) questionnaire. Psychological distress symptoms were evaluated using the Hospital Anxiety Depression Score (HADS) and the Impact of Event Scale (IES). In-hospital mortality rates at 3 months and 1 year were, respectively, 39.1, 50.7 and 57.2%, respectively. At 3 months, median [IQR] physical and mental component summary scores (PCS and MCS) (SF-36) were 37 [28–46] and 51 [45–58], respectively. PCS was lower in ICU patients with HMs when compared to general ICU septic patients (52 [5–13], p = 0.00001). The median combined HAD score was 8 [5–13], and the median IES score was 8 [3–16]. However, recovery during the first year after ICU discharge was not consistent in all dimensions of HRQOL. Three months after ICU discharge, the maximum daily Sequential Organ Failure Assessment score and status of the underlying malignancy at ICU admission were significantly associated with MCS impairment (− 0.54 points [95% CI − 0.99; − 0.1], p = 0.018 and − 4.83 points [95% CI − 8.44; − 1.22], p = 0.009, respectively).
Conclusion
HRQOL is strongly impaired in critically ill patients with HMs at 3 months and 1 year after ICU discharge. Organ failure and disease status are strongly associated with QOL. The kinetic evaluation of QOL at 3 months and 1 year offers the opportunity to focus on QOL aspects that may be improved by therapeutic interventions during the first year after ICU discharge.
Similar content being viewed by others
Background
Over the last few decades, the increased intensity of treatments in patients with haematological malignancies (HMs) has translated into an improved survival rate. As a consequence of more aggressive chemotherapies and their complications, the need for patients with HMs for intensive care unit (ICU) support during the course of their disease has increased. Although outcomes of these patients have been fully investigated in terms of organ failure and mortality [1], data are scarce on health-related quality of life (HRQOL) in this population [2]. Long-term outcomes for physical and psychological factors, functional status and social interactions are becoming more and more important both for physicians and nurses and for patients and their relatives. Moreover, quality-of-life (QOL) measurements should be considered when making decisions on the allocation of healthcare resources.
In the ICU, HRQOL at admission has been shown to be inversely associated with multiple organ failure during hospitalization [3] and hospital mortality [4]. Moreover, baseline HRQOL has been shown to be correlated with HRQOL following discharge [5, 6]. Finally, ICU survivors have significantly lower QOL compared with gender- and age-matched general population [7]. Data on HRQOL in critically ill patients with HMs are scarce [2]. Given the importance of the underlying disease as a strong predictor of HRQOL, the present study focused on critically ill haematological patients. We aim to assess post-ICU burden and HRQOL at 3 months and 1 year after ICU discharge and to identify risk factors for QOL impairment using the three widely used tools in this context: Short Form 36 (SF-36) [8, 9], Hospital Anxiety and Depression Scale (HADS) [10] and Impact of Event Scale (IES) [11].
Patients and methods
Description
The study was approved by the appropriate ethics committees in France and Belgium. All patients or relatives were informed and consented to participate in the study. The TRIALOH study was carried out in 17 university or university-affiliated centres in France and Belgium that belonged to a research network instituted in 2005 [1]. From 1 January 2010, to 1 May 2011, consecutive patients with HMs who were admitted to the participating ICUs for any reason were included.
Exclusion criteria were: complete cure of the malignancy for more than 5 years, ICU admission only to maximize safety of a procedure and age younger than 18 years. In each centre, we reported the ICU refusal rate (number of patients considered for ICU admission but eventually not admitted/number of patients admitted to the ICU throughout the study period).
Data collection
In each centre, a standardized electronic case-report form was used to collect the study data. All QOL-related data were collected prospectively. Ninety days and 1 year after ICU discharge, HRQOL was assessed by asking alive patients to complete the SF-36 questionnaire (SF-36) during a telephone interview by a trained social worker.
The SF-36 includes one multi-item scale that assesses eight health concepts: (1) limitations in physical activities because of health problems; (2) limitations in social activities because of physical or emotional problems; (3) limitations in usual role activities because of physical health problems; (4) bodily pain; (5) general mental health (psychological distress and well-being); (6) limitations in usual role activities because of emotional problems; (7) vitality (energy and fatigue); and (8) general health perceptions [12]. Higher scores represent better functioning, with a range from 0 to 100. Physical and mental summary components (PCS and MCS, respectively) constitute aggregates of the eight individual dimensions and provide norm-based summary scores from physically and mentally oriented subscales. IES and HAD scale (HADS) are self-report instruments that assess the essential characteristics associated with stress and anxiety disorders among patients in a non-psychiatric hospital. The HADS is a 14-item self-report measure of psychological distress. The HADS has two subscales (anxiety and depression), each ranging from 0 to 21. Each item is rated on a scale from 0 (“not at all”) to 3 (“very much”), and higher scores indicate greater anxiety and depression. Scores from the two subscales are combined into a full-scale score that is indicative of a clinical disorder if greater than or equal to 12 points [13]. The IES is a widely used self-report measure of traumatic stress based on two subscales, evaluating intrusion and avoidance. Score of 33 points or more is described as a cut-off for a probable diagnosis of post-traumatic syndrome disorder (PTSD) [14].
Definitions
Malignancies were considered as newly diagnosed if they had been diagnosed within the past 4 weeks before ICU admission. The sepsis-related organ failure assessment (SOFA) score was computed at admission then daily throughout the patient’s stay in the ICU; this score provides an estimate of the risk of ICU death based on organ dysfunction [15]. Performance status was evaluated using the Eastern Cooperative Oncology Group scale (ECOG). Fully active, able to carry on all pre-disease performance without restriction; restricted in physically strenuous activity but ambulatory and able to carry out work of a light or sedentary nature, e.g. light house work, office work; ambulatory and capable of all self-care but unable to carry out any work activities; up and about more than 50% of waking hours; capable of only limited self-care; confined to bed or chair more than 50% of waking hours; completely disabled; cannot carry on any self-care; totally confined to bed or chair; dead. The ECOG performance status and Charlson comorbidity index were determined at ICU admission [16, 17].
Reasons for ICU admission were recorded based on the main symptoms at ICU admission. Aetiologic diagnoses of sepsis and acute respiratory failure were made by consensus by the intensivists, hematologists and consultants. In particular, aetiologies of pulmonary involvement were diagnosed based on predefined criteria [1, 18].
Statistical analysis
Continuous variables are described as medians and interquartile ranges (IQRs) and were compared between groups using the Wilcoxon’s rank-sum test. Discrete variables are described with counts and percentages and were compared using Fisher’s exact test. We report norm-based measurements of the SF-36 subscores (mean 50, SD 10), after age and sex standardization using reference values for the French population [19]. SF-36 aggregate components (i.e. PCS and MCS) were computed as recommended [8, 20] and expressed on a normalized scale centred on 50 representing the population norm (i.e. values > or < 50 reflecting values higher or lower than age–sex standardized French values). Missing data in the individual SF-36 questions were imputed using the personal mean score approach [21]. The SF-36 aggregate scores (PCS and MCS) were compared using Wilcoxon’s rank-sum test among groups defined by categorical factors in univariate analysis. Correlations between SF-36 aggregate scores and quantitative variables were estimated and tested using Spearman correlation coefficient (with its 95% confidence interval [95% CI], estimated by bootstrap with 1000 replications). Adjusted multivariate models of factors associated with PCS and MCS were selected, using linear regression models: characteristics available at ICU admission associated with p values less than 0.2 by univariate analysis were candidates, and final models were selected using backward stepwise procedures (based on a p value < 0.20).
SF-36 scores at 3 months versus 1 year after discharge from the ICU were compared using Wilcoxon’s signed-rank test. Factors associated with the variation of SF-36 were examined using Wilcoxon and Kruskal–Wallis tests (discrete variables), or using Spearman correlation coefficient testing (continuous variables). Last, the age–sex standardized norm-based SF-36 items and aggregate scores in the HM cohort were compared to those of a sepsis cohort of 37 patients, including adult (≥ 18 years old) patients surviving to an ICU hospitalization for a septic shock without HM. These patients were recruited from two prospective studies on sepsis [22, 23]. Secondarily, the comparison was performed after matching patients on age and sex. Factors associated with the IES and HADS scores were investigated with a similar approach, in univariate analysis.
All tests were two-sided, and p values less than .05 were considered significant. Analyses were performed using R software version 3.2.2 [24].
Results
Patients
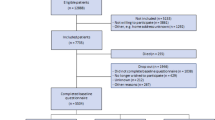
In total, 1011 patients were included in the TRIALOH study. In-hospital mortality rates at 3 months and 1 year were 39.1, 50.7 and 57.2%, respectively. At 3 months, 278, 271 and 269 patients completed the SF-36, HADS and IES forms, respectively (Fig. 1).
Table 1 shows patient characteristics of the ICU survivors. Among them, patients who did not complete the SF-36 form at 3 months were older and more likely to require renal replacement therapy than those who completed the form (p = 0.02 and p = 0.025, respectively). Conversely, bone marrow transplant recipients were more likely to complete the form at 3 months (p = 0.024) and 1 year (p = 0.062) (Table 1 and Additional file 1: Table S1). At 1 year, we did not find any other difference between responders and non-responders (Additional file 1: Table S1).
SF-36 score at 3 months and 1 year after ICU discharge
The results of SF-36 scores at 3 months and 1 year are shown in Fig. 2. At 3 months, the median [IQR] age–sex standardized norm-based physical component summary score (PCS) was 37 [28–46], which corresponds to − 1.3 SD compared to the French general population, and the median [IQR] mental component summary score (MCS) was 51 [45–58]. Median age–sex standardized MCS values were similar (0.1 SD) to those of the general population in HMs patients (Table 2).
Radar chart of the health-related quality of life (HRQOL) at 3 and 12 months after ICU discharge. M3, 3 months after ICU discharge; M12, 12 months after ICU discharge; RP, role—function physical; PF, physical functioning; MH, mental health; RE, role—emotional; SF, social functioning; VT, vitality; GH, general health; and BP, bodily pain
All subscores were not affected proportionally: while the median role function—physical (RP), median vitality (VT) and median general health (GH) scores were 32 [26–41], 41 [31–48] and 38 [30–48], respectively, median role function—emotional (RE) score, median mental health (MH), median social functioning (SF) and bodily pain (BP) scores were 54 [38–55], 53 [45–60], 51 [31–58] and 50 [38–62], respectively.
Evolution of these scores over time is shown in Fig. 2 and Table 2. MH, RE and GH scores decreased significantly between 3 months and 1 year after ICU discharge (p = 0.003, p = 0.005 and p = 0.038, respectively). MCS decreased significantly between 3 months and 1 year (p = 0.006). Conversely, RP increased significantly between 3 months and 1 year (p = 0.0004). Performance status has been shown to be strongly correlated with physical role functioning and functional capacity [25, 26]. When considering the performance status as a marker of functional capacity at baseline, we found a decrease in functional capacity from ICU admission to 3 months, with partial recovery in survivors at 1 year (Additional file 1: Figure S1).
Detailed answers to the question “Compared to 1 year ago, how would you rate your health in general now?” (item 2 of the SF-36) are shown in Fig. 3. Among survivors, 42% of patients felt better than 1 year before and 38.6% felt worse than 1 year before.
Comparison of critically ill patients with HMs with septic shock patients without HMs
We then compared QOL 3 months after discharge in critically ill patients with HMs with QOL in critically ill patients with septic shock without HMs. After matching for age and sex, we found that median PCS values were higher in septic shock patients than in HMs patients (52 [37–59] vs. 37 [29–46], p = 0.007, respectively). There was no significant difference between HMs and septic shock survivors regarding the MCS aggregate of the SF-36 questionnaire (54 [45–58] vs. 50 [45–58], p = 0.99, respectively) (Table 3). PF, RP, VT and SF subscores were significantly higher in septic shock patients than in HMs patients (p = 0.016, p = 0.007, p = 0.035 and p = 0.007, Table 3).
Factors associated with QOL
Overall, 3 months after ICU discharge, the need for invasive mechanical ventilation (MV), baseline status of the underlying malignancy (partial or complete remission of the disease vs. evolutive), the need for renal replacement therapy, the need for vasopressors, sedation, SOFA score and haematopoietic stem cell transplant were associated with the MCS at a 20% level in univariate analysis (Additional file 1: Table S2); they were included as candidate factors in a multivariate adjusted model. After selection, SOFA score and baseline status of the underlying malignancy remained independently associated with MCS impairment (− 0.54 points [95% CI − 0.99; − 0.1], p = 0.018 and − 4.83 points [95% CI − 8.44; − 1.22], p = 0.009, respectively) (Fig. 4).
The only variable associated with PCS impairment at 3 months at a 20% level in univariate analysis was the Charlson index (Additional file 1: Table S3).
Of note, patients in partial or complete remission had a longer median time from the diagnosis of the underlying malignancy and ICU admission than patients classified as having an evolutive disease. Indeed, most patients in the latter case (57.3% of the patients classified as having an evolutive disease) had a newly diagnosed malignancy when admitted to the ICU (Additional file 1: Figure S2)
We did not find any association between these variables and MCS or PCS at 1 year after ICU discharge. (Univariate analyses are shown in Additional file 1: Tables S4 and S5.)
Post-traumatic stress disorder
Three months after ICU discharge, 269 patients completed the IES form. The median IES score was 8 [3, 16]. The median intrusion subscore was 3 [0; 9], and the median avoidance subscore was 3 [0; 8]. Overall, 22 (8%) patients had an IES score greater than 35 points, which is considered the threshold for PTSD.
Men had a higher IES score than women (10 [4–21] vs. 6 [1–13], respectively, p = 0.0008). The IES score was positively correlated with length of stay in the ICU (correlation coefficient 0.14 [95% CI 0.02; 0.026], p = 0.025) (Additional file 1: Figure S3). By univariate analysis, ICU length of stay was associated with IES score at 3 months (Additional file 1: Table S6).
Anxiety and depression
Three months after ICU discharge, patients had a median combined HAD score of 8 [5–13]. Considering both the subscales separately, 42 patients (15.5%) had an anxiety score > 8 and 41 patients (15%) had a depression score > 8, which are considered clinical disorders.
Discussion
This prospective study is the first multicenter study and the largest one focusing on HRQOL in critically ill patients with HMs.
To analyse all aspects of QOL, we used the SF-36 form, which offers a detailed mental and physical QOL evaluation and has been widely used and validated in ICU patients, the IES for post-traumatic stress syndrome evaluation and the HADS for evaluation of anxiety and depression.
In total, 1011 patients were included in the TRIALOH study. With a mortality rate of 50.7% (513 patients) at 3 months, 55.8% of survivors (278 patients) completed the SF-36 form at 3 months. Although response rates vary a lot between studies in ICU, ranging from 30 to 80% [27, 28], our response rate is somewhat low (56% of the survivors) and may be explained in part by the high morbidity of patients with HMs, who require multiple hospitalizations and treatments in the course of their disease. Indeed, more days spent at hospital have been associated with no response at follow-up [28]. Populations who are lost to follow-up or did not answer the questionnaire may have different demographic characteristics and different profiles of ICU-related morbidity than those who completed the QOL evaluation. Indeed, we found that age and the need for replacement therapy during ICU stay were 2 factors associated with the inability/refusal to complete the form. Different methods have been used during the study to improve response rates, such as sending hand written letters and employing reminders to the patients.
Compared with general ICU patients with septic shock, critically ill patients with HMs have profound alterations of HRQOL at 3 months. Moreover, although RP values improved at 1 year, global QOL impairment was consolidated at 1 year.
In a single-centre study, Oeyen et al. [2] investigated long-term outcomes and QOL in critically ill patients with HMs (85 patients) or solid malignancies 3 months and 1 year after ICU discharge. Similarly, they found a profound alteration of QOL at 3 months and 1 year in HM patients with median PCS and MCS values even lower than those we observed in our study. Practices may have evolved over time, taking into account the QOL as an important goal when managing these patients. This may partly explain the discrepancy between the two studies.
In the present study, two main independent factors were significantly associated with QOL impairment (MCS) at 3 months: the SOFA score (i.e. organ failure) and the status of the underlying malignancy (complete or partial remission) at ICU admission. The initial SOFA score is used to quantify the degree of organ dysfunction present on admission, including the need for mechanical ventilation, vasopressors or renal replacement therapy. Many studies have demonstrated a strong correlation of initial SOFA score with mortality outcome [15, 29, 30]. In our study, we have moved a step further, presenting SOFA score as a reliable predictor of QOL after ICU discharge. Combes et al. [31] previously showed that prolonged invasive mechanical ventilation is associated with impaired HRQOL compared with that of a matched general population. Noninvasive strategies during ICU stay, such as decreasing the use of mechanical ventilation by using high flow oxygen, when appropriate, may improve QOL.
SOFA score has previously been associated with impaired QOL in critically ill patients with acute respiratory distress syndrome [32]. In clinical practice, a crucial question is “for which critically ill HMs patients should we propose a limitation or withdrawal of life-sustaining treatments”? Decisions on withholding/withdrawing therapies should take into account the expected QOL after ICU discharge; the primary goal of intensive care being to return to a quality of life the patient would have found acceptable. Considering the SOFA score at admission as a predictor of both mortality and QOL, it may be helpful to physicians to inform patients and families in a reliable way and to guide in treatment decisions.
Paradoxically, disease status (partial or complete remission) at ICU admission was also associated with MCS impairment at 3 months. Patients in partial or complete remission have previously received intensive and potentially gruelling treatments for their underlying malignancy; conversely, most of patients classified as having an “evolutive disease” have newly diagnosed malignancies when admitted to the ICU. Indeed, patients who are considered in partial or complete remission had a longer time from the diagnosis of the underlying malignancy to ICU admission and, overall, have therefore received more chemotherapy than patients with evolutive disease.
The kinetic evaluation of QOL at 3 months and 1 year offers the opportunity to focus on aspects of QOL that may be improved by therapeutic interventions during the first year after ICU discharge. If some aspects of QOL (such as RP) have improved over time, we found that BP, GH, MH, RE scores and MCS decreased between 3 months and 1 year after ICU discharge. In general ICU populations, previous studies have shown that the majority of the QOL scores recover over time [5]. Impairment of SF and RE suggests that patients with HMs may be socially isolated because of their condition. Association of a long hospital stay, including ICU stay and the presence of an underlying malignancy, has been shown to be major risk factors for social isolation [33, 34].
During hospitalization, HM patients have to deal not only with treatment-related complications and adverse events, such as physical symptoms and changes in body image, but also with isolation-related psychological distress, including loss of control and lack of contact with family members and friends. Long-term psychological follow-up, social support and recreational activities during hospitalization may improve the QOL of these patients [34, 35]. Centres that manage haematological patients may also consider extending visiting hours for relatives. Finally, bodily pain may be controlled by an approach carried out by a skilled pain care team and based on the association of causal therapies and adequate analgesics. PF, RP, VT and PCS are significantly lower in HMs patients compared with septic patients. Indeed, HMs and chemotherapies have been shown to induce a loss of weight and decrease in physical activity. Early mobilization in ICU and exercise may prevent the rapid loss of physical reserve and increase functional capacity [36].
In the princeps study published in 2013 by Azoulay et al. [1], 6 months after ICU discharge, the hematologists reported that all but seven ICU survivors were continuing their cancer treatment that ICU admission did not influence therapeutic intensity in 80% of ICU survivors, and that 80% of ICU survivors were in complete or partial remission. Unfortunately, precise data on post-ICU treatments are not available and we could not evaluate their impact on QOL.
Interestingly, only 8% of patients in our cohort were diagnosed with PTSD, according to the IES, which is lower than usually reported [37]. The use of an ICU diary in many participating centres may have participated in the low incidence of PTSD as an ICU diary has been associated with a significant reduction in PTSD symptoms in critical illness survivors [37]. A prospective multicenter comparative study of the impact of an ICU diary on PTSD in ICU is ongoing, involving many of the participating centres involved in this work.
The present study has several limitations. First, we were unable to provide QOL measures at ICU admission. Emergent admission and critical illness prevent patients from providing self-reported baseline QOL at the time of ICU admission. Reliable retrospective QOL data are difficult to obtain due to memory biases following ICU discharge. Answers to the question “Compared to 1 year ago, how would you rate your health in general now?” suggest that almost half of the patients felt better than 1 year before. Factors such as severity of current symptoms may bias patients’ recall of baseline status, especially in more severe patients, such as ICU patients [38]. Indeed, Granja et al. [39] have shown that almost 50% of ICU survivors did not remember the time in the hospital before ICU admission. Moreover, proxy assessment of patients’ baseline quality of life often differs from the patient’s assessment [40]. Despite these limitations, HRQOL impairment at ICU admission has been correlated with multiple organ failure during ICU stay, increased hospital mortality and worsened HRQOL following discharge [4, 6].
Second, as mentioned above, the response rate (55.8% of the survivors) is low, which is explained by the high morbidity of our population.
Third, our data are now 7 years old. Improvements in outcomes of cancer patients, as well as the improvements in process of care may have modified the impact of ICU complications on HRQOL. In HM patients, several cohort studies and trials evaluating a noninvasive diagnostic and therapeutic management of acute respiratory failure have shown the feasibility and safety of the noninvasive strategy [41]. High flow oxygen has also demonstrated survival benefits as compared to noninvasive ventilation [42]. The increased use of noninvasive strategies may then have improved HRQOL of these patients after ICU discharge.
Finally, a longer follow-up would have been interesting to analyse, as a gradual improvement of most aspects of QOL might have occurred after 1 year.
Conclusion
This study shows that HRQOL is strongly impaired in critically ill patients with HMs at 3 months and 1 year after ICU discharge. SOFA score and disease status are strongly correlated with QOL. Recovery after the ICU is not consistent in all dimensions of HRQOL. Future studies should focus on specific physical and psychosocial rehabilitation programs that may start in the ICU. They may then continue after ICU discharge and could lead to improved management of patients with HMs after their stay in the ICU.
Abbreviations
- ICU:
-
intensive care unit
- HM:
-
haematological malignancy
- HRQOL:
-
health-related quality of life
- QOL:
-
quality of life
- SF-36:
-
Short Form 36 questionnaire
- HADS:
-
Hospitality and Depression Scale
- IES:
-
Impact of Event Scale
- PTSD:
-
post-traumatic stress disorder
- SOFA:
-
the sepsis-related organ failure assessment
- MDS:
-
myelodysplastic syndrome
- AML:
-
acute myeloid leukaemia
- CLL:
-
chronic lymphocytic leukaemia
- CML:
-
chronic myeloid leukaemia
- BMT:
-
bone marrow transplantation
- HSCT:
-
haematopoietic stem cell transplant
- LOS:
-
length of stay
- ALL:
-
acute lymphoid leukaemia
- MCS:
-
mental component summary score
- PCS:
-
physical component summary score
- RP:
-
role function—physical
- VT:
-
vitality
- MH:
-
mental health
- GH:
-
general health
- RE:
-
role—emotional
- BP:
-
bodily pain
- SF:
-
social functioning
- PF:
-
physical functioning
References
Azoulay E, Mokart D, Pene F, Lambert J, Kouatchet A, Mayaux J, et al. Outcomes of critically Ill patients with hematologic malignancies: prospective multicenter data from France and Belgium: A Groupe de Recherche Respiratoire en reanimation onco-hematologique study. J Clin Oncol. 2013;31(22):2810–8.
Oeyen SG, Benoit DD, Annemans L, Depuydt PO, Van Belle SJ, Troisi RI, et al. Long-term outcomes and quality of life in critically ill patients with hematological or solid malignancies: a single center study. Intensive Care Med. 2013;39(5):889–98.
Gerth AMJ, Hatch RA, Young JD, Watkinson PJ. Changes in health-related quality of life after discharge from an intensive care unit: a systematic review. Anaesthesia. 2019;74(1):100–8.
Hofhuis JGM, Spronk PE, van Stel HF, Schrijvers AJP, Bakker J. Quality of life before intensive care unit admission is a predictor of survival. Crit Care Lond Engl. 2007;11(4):R78.
Hofhuis JGM, Spronk PE, van Stel HF, Schrijvers GJP, Rommes JH, Bakker J. The impact of critical illness on perceived health-related quality of life during ICU treatment, hospital stay, and after hospital discharge: a long-term follow-up study. Chest. 2008;133(2):377–85.
Oeyen S, Vermeulen K, Benoit D, Annemans L, Decruyenaere J. Development of a prediction model for long-term quality of life in critically ill patients. J Crit Care. 2018;43:133–8.
Myhren H, Ekeberg Ø, Stokland O. Health-related quality of life and return to work after critical illness in general intensive care unit patients: a 1-year follow-up study. Crit Care Med. 2010;38(7):1554–61.
Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83.
Angus DC, Carlet J. 2002 Brussels roundtable participants. Surviving intensive care: a report from the 2002 Brussels roundtable. Intensive Care Med. 2003;29(3):368–77.
Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–70.
Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41(3):209–18.
McHorney CA, Ware JE, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32(1):40–66.
Scragg P, Jones A, Fauvel N. Psychological problems following ICU treatment. Anaesthesia. 2001;56(1):9–14.
Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale: revised. Behav Res Ther. 2003;41(12):1489–96.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The sepsis-related organ failure assessment (SOFA) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10.
Soares M, Salluh JIF, Carvalho MS, Darmon M, Rocco JR, Spector N. Prognosis of critically ill patients with cancer and acute renal dysfunction. J Clin Oncol Off J Am Soc Clin Oncol. 2006;24(24):4003–10.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Schellongowski P, Staudinger T, Kundi M, Laczika K, Locker GJ, Bojic A, et al. Prognostic factors for intensive care unit admission, intensive care outcome, and post-intensive care survival in patients with de novo acute myeloid leukemia: a single center experience. Haematologica. 2011;96(2):231–7.
Leplège A, Ecosse E, Verdier A, Perneger TV. The French SF-36 Health Survey: translation, cultural adaptation and preliminary psychometric evaluation. J Clin Epidemiol. 1998;51(11):1013–23.
Ware JE, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care. 1995;33(4 Suppl):AS264–79.
Peyre H, Leplège A, Coste J. Missing data methods for dealing with missing items in quality of life questionnaires. A comparison by simulation of personal mean score, full information maximum likelihood, multiple imputation, and hot deck techniques applied to the SF-36 in the French 2003 decennial health survey. Qual Life Res. 2011;20(2):287–300.
Boissier F, Razazi K, Seemann A, Bedet A, Thille AW, de Prost N, et al. Left ventricular systolic dysfunction during septic shock: the role of loading conditions. Intensive Care Med. 2017;43(5):633–42.
Contou D, Roux D, Jochmans S, Coudroy R, Guérot E, Grimaldi D, et al. Septic shock with no diagnosis at 24 hours: a pragmatic multicenter prospective cohort study. Crit Care Lond Engl. 2016;20(1):360.
Arogundade FA, Zayed B, Daba M, Barsoum RS. Correlation between Karnofsky Performance Status Scale and Short-Form Health Survey in patients on maintenance hemodialysis. J Natl Med Assoc. 2004;96(12):1661–7.
Atkinson TM, Andreotti CF, Roberts KE, Saracino RM, Hernandez M, Basch E. The level of association between functional performance status measures and patient-reported outcomes in cancer patients: a systematic review. Support Care Cancer Off J Multinatl Assoc Support Care Cancer. 2015;23(12):3645–52.
Eddleston JM, White P, Guthrie E. Survival, morbidity, and quality of life after discharge from intensive care. Crit Care Med. 2000;28(7):2293–9.
Andersen FH, Flaatten H, Klepstad P, Romild U, Kvåle R. Long-term survival and quality of life after intensive care for patients 80 years of age or older. Ann Intensive Care [Internet]. 2015 Dec [cited 2018 Nov 15]; 5(1). http://www.annalsofintensivecare.com/content/5/1/13.
Ferreira FL. Serial evaluation of the SOFA Score to predict outcome in critically ill patients. JAMA. 2001;286(14):1754.
Moreno R, Vincent JL, Matos R, Mendonça A, Cantraine F, Thijs L, et al. The use of maximum SOFA score to quantify organ dysfunction/failure in intensive care. Results of a prospective, multicentre study. Working Group on Sepsis related Problems of the ESICM. Intensive Care Med. 1999;25(7):686–96.
Combes A, Costa M-A, Trouillet J-L, Baudot J, Mokhtari M, Gibert C, et al. Morbidity, mortality, and quality-of-life outcomes of patients requiring > or = 14 days of mechanical ventilation. Crit Care Med. 2003;31(5):1373–81.
Pfoh ER, Wozniak AW, Colantuoni E, Dinglas VD, Mendez-Tellez PA, Shanholtz C, et al. Physical declines occurring after hospital discharge in ARDS survivors: a 5-year longitudinal study. Intensive Care Med. 2016;42(10):1557–66.
Chambers SK, Baade P, Youl P, Aitken J, Occhipinti S, Vinod S, et al. Psychological distress and quality of life in lung cancer: the role of health-related stigma, illness appraisals and social constraints. Psychooncology. 2015;24(11):1569–77.
Annibali O, Pensieri C, Tomarchio V, Biagioli V, Pennacchini M, Tendas A, et al. Protective isolation for patients with haematological malignancies: a pilot study investigating patients’ distress and use of time. Int J Hematol Oncol Stem Cell Res. 2017;11(4):313–8.
Allart P, Soubeyran P, Cousson-Gélie F. Are psychosocial factors associated with quality of life in patients with haematological cancer? A critical review of the literature: psychosocial factors and quality of life in haematological patients. Psychooncology. 2013;22(2):241–9.
Cormie P, Zopf EM, Zhang X, Schmitz KH. The impact of exercise on cancer mortality, recurrence, and treatment-related adverse effects. Epidemiol Rev. 2017;39(1):71–92.
Parker AM, Sricharoenchai T, Raparla S, Schneck KW, Bienvenu OJ, Needham DM. Posttraumatic stress disorder in critical illness survivors: a metaanalysis*. Crit Care Med. 2015;43(5):1121–9.
Schmier JK, Halpern MT. Patient recall and recall bias of health state and health status. Expert Rev Pharmacoecon Outcomes Res. 2004;4(2):159–63.
Granja C, Gomes E, Amaro A, Ribeiro O, Jones C, Carneiro A, et al. Understanding posttraumatic stress disorder-related symptoms after critical care: the early illness amnesia hypothesis*. Crit Care Med. 2008;36(10):2801–9.
Gifford JM, Husain N, Dinglas VD, Colantuoni E, Needham DM. Baseline quality of life before intensive care: a comparison of patient versus proxy responses. Crit Care Med. 2010;38(3):855–60.
Azoulay E, Mokart D, Lambert J, Lemiale V, Rabbat A, Kouatchet A, et al. Diagnostic strategy for hematology and oncology patients with acute respiratory failure: randomized controlled trial. Am J Respir Crit Care Med. 2010;182(8):1038–46.
Frat J-P, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372(23):2185–96.
Authors’ contributions
FE, LZ and EA contributed to conception and design. FE, LZ, EA, VL, DM, FP, AK, JM, FV, MN, FB, AR, CL, PP, APM, DB, RH, MD, DC and NDP were involved in provision of study materials or patients, collection and assembly of data. LB, FE, LZ and EA were involved in data analysis and interpretation. FE, LZ and LB contributed to manuscript writing. All authors read and approved the final manuscript.
Acknowledgements
The authors thank Etienne Audureau for his valuable participation in the methodology and statistical analysis of the study.
Competing interests
The authors indicate no potential competing interests related to the study.
Availability of data and materials
The datasets generated and analysed during the current study are not publicly available due to the potential risk of leakage of personally identifiable information.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the appropriate ethics committees in France and Belgium (PHRC AOM 08235).
Funding
The study was supported by grant PHRC AOM 08235 from the French Ministry of Health.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional information
Dr. Antoine Rabbat, co-author of the manuscript is deceased
Additional file
Additional file 1.
Tables and figures.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ehooman, F., Biard, L., Lemiale, V. et al. Long-term health-related quality of life of critically ill patients with haematological malignancies: a prospective observational multicenter study. Ann. Intensive Care 9, 2 (2019). https://doi.org/10.1186/s13613-018-0478-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-018-0478-3