Abstract
Background
Anti-synthetase (AS) and dermato-pulmonary associated with anti-MDA-5 antibodies (aMDA-5) syndromes are near one of the other autoimmune inflammatory myopathies potentially responsible for severe acute interstitial lung disease. We undertook a 13-year retrospective multicenter study in 35 French ICUs in order to describe the clinical presentation and the outcome of patients admitted to the ICU for acute respiratory failure (ARF) revealing AS or aMDA-5 syndromes.
Results
From 2005 to 2017, 47 patients (23 males; median age 60 [1st–3rd quartiles 52–69] years, no comorbidity 85%) were admitted to the ICU for ARF revealing AS (n = 28, 60%) or aMDA-5 (n = 19, 40%) syndromes. Muscular, articular and cutaneous manifestations occurred in 11 patients (23%), 14 (30%) and 20 (43%) patients, respectively. Seventeen of them (36%) had no extra-pulmonary manifestations. C-reactive protein was increased (139 [40–208] mg/L), whereas procalcitonine was not (0.30 [0.12–0.56] ng/mL). Proportion of patients with creatine kinase ≥ 2N was 20% (n = 9/47). Forty-two patients (89%) had ARDS, which was severe in 86%, with a rate of 17% (n = 8/47) of extra-corporeal membrane oxygenation requirement. Proportion of patients who received corticosteroids, cyclophosphamide, rituximab, intravenous immunoglobulins and plasma exchange were 100%, 72%, 15%, 21% and 17%, respectively. ICU and hospital mortality rates were 45% (n = 21/47) and 51% (n = 24/47), respectively. Patients with aMDA-5 dermato-pulmonary syndrome had a higher hospital mortality than those with AS syndrome (n = 16/19, 84% vs. n = 8/28, 29%; p = 0.001).
Conclusions
Intensivists should consider inflammatory myopathies as a cause of ARF of unknown origin. Extra-pulmonary manifestations are commonly lacking. Mortality is high, especially in aMDA-5 dermato-pulmonary syndrome.
Similar content being viewed by others
Background
Identifying the cause of acute respiratory distress syndrome (ARDS) is a crucial step for initiating a targeted treatment and improving prognosis [1, 2]. However, two recent studies [3, 4] showed that 8% of patients with ARDS according to the Berlin criteria [5] lacked exposure to “common” risk factors (e.g., pneumonia, acute pancreatitis, aspiration of gastric content or extra-pulmonary sepsis) with no etiology eventually retrieved in 80% of them [4]. For such atypical ARDS, a comprehensive diagnostic work-up, including specific immunologic tests, is recommended [6] so that to identify immune causes, typically amenable to specific therapeutic interventions (e.g., corticosteroids). Yet, an ancillary analysis [4] of an international, multicenter, prospective cohort study [7] reported that such immunological examinations were performed in only 5% of ARDS without common risk factors.
Anti-synthetase (AS) and anti-melanoma differentiation-associated gene 5 (aMDA-5) syndromes are near one of the other autoimmune inflammatory myopathies [8] potentially responsible for rapidly progressive interstitial lung disease leading to acute respiratory failure and ARDS [9,10,11,12]. AS and aMDA-5 dermato-pulmonary syndromes may be clinically indistinguishable one from another, with almost three-quarter of patients with aMDA-5 dermato-pulmonary syndrome exhibiting the clinical attributes of the AS syndrome [8]. When ARF is the initial presentation of AS or aMDA-5 syndromes [9,10,11, 13,14,15,16,17] or when extra-respiratory manifestations, such as muscular, cutaneous or articular signs are lacking [9, 18,19,20,21,22], the diagnosis is challenging, especially in the intensive care unit (ICU) setting, where many other reasons of acute respiratory failure (ARF) can be discussed. To the best of knowledge, a number of case reports of ARF revealing autoimmune inflammatory myopathies have been previously reported, but an extended case series has not been published as yet.
Therefore, we undertook this retrospective study in order to: (1) describe the clinical features and the outcome of patients admitted to the ICU for ARF revealing either an AS or an aMDA-5 dermato-pulmonary syndrome, and; (2) identify predictive factors of hospital mortality.
Patients and methods
Patients
We conducted a 13-year multicenter retrospective non-interventional study in 35 ICUs in France from January 1, 2005, to December 31, 2017. All patients older than 18 years were included if they met the following criteria: (1) admitted to the ICU for ARF not related to cardiogenic pulmonary edema; (2) no common ARDS risk factor, among pneumonia, acute pancreatitis, aspiration of gastric content, extra-pulmonary sepsis, multiple transfusions, major trauma, pulmonary vasculitis, drowning, severe burns, identified according to the Berlin definition [5]; (3) immunologic test performed during ICU stay, which was positive for anti-synthetase (Jo-1, PL7, PL12, OJ, EJ, KS, Zo, YRS/Tyr/Ha) or anti-MDA-5 autoantibodies; and (4) no alternative diagnosis for ARF. It is worth notifying that in the present study the diagnosis of AS or aMDA-5 dermato-pulmonary syndromes had to be made during the ICU stay. Therefore, those who had a diagnosis of AS or aMDA-5 made before ICU admission were not included.
The investigator of each participating center was responsible for the identification of the patients, either from the hospital medical reports, using the function “research the files in which the key words MDA-5 or anti-synthetase or myositis occurs” of Microsoft Windows®, or through a search using the International Classification of Diseases (10th Revision) following codes: M608 (autoimmune myositis), M609 (myositis), M332 (polymyositis) and M331 (dermatomyositis). The clinical charts of all identified patients were anonymized before sending to the main investigators (DC and CV). Clinical charts were reviewed in order to check the inclusion criteria.
Data collection
The following data were collected on a standardized anonymized case record form: demographic characteristics (age, gender), severity scores upon ICU admission (Sequential Organ Failure Assessment [23] and Simplified Acute Physiology Score II [24]), main comorbidities, delay between first respiratory sign and ICU admission, clinical examination (respiratory and extra-respiratory manifestations) and laboratory findings at the time of ICU admission (blood leukocytes and platelets counts, serum procalcitonine, C-reactive protein, creatine kinase and creatinine levels, PaO2/FiO2 with FiO2 calculated according to the following formula [25, 26]: FiO2 = oxygen flow in liter per minute × 0.04 + 0.21 when standard oxygen was used), radiological findings on chest X-ray and CT scan, cytological and bacteriological analyses of broncho-alveolar lavage (BAL) fluid, type of positive autoantibodies (Jo-1, PL7, PL12, OJ, EJ, KS, Zo, YRS/Tyr/Ha or aMDA-5), immunosuppressive treatments received (corticosteroids, cyclophosphamide, rituximab, basiliximab, tacrolimus, cyclosporine, methotrexate, intravenous immunoglobulins or plasma exchange), organ supports in the ICU (invasive mechanical ventilation, extra-corporeal membrane oxygenation (ECMO), renal replacement therapy, vasopressors), ICU and hospital length of stay, ICU and hospital mortality.
Written reports of chest CT scan performed at the time of ICU admission were sent to the main investigators (DC and CV) in order to individualize elementary lesions (ground-glass attenuation, alveolar consolidation, septal thickening, pleural effusion, pneumothorax, pneumomediastinum and mediastinal lymphadenopathy) and their location (lower or upper lobe predominance). Signs of lung fibrosis (honeycombing, traction bronchiectasis and reticulations) were also collected. Cytological analyses of BAL fluid collected at the time of ICU admission were reported, as well as results of open lung, skin or muscle biopsies, if performed.
Statistical analysis
Continuous variables are reported as median [1st–3rd quartiles] and compared by the Mann–Whitney U test. Categorical variables are reported as counts and percentage points in groups and compared by using the Fisher’s exact test. Survival curves of patients with aMDA-5 and AS syndromes were drawn using the Kaplan–Meier method and compared using the log-rank test. All tests were two-sided, with p < 0.05 indicating statistical significance. The statistical analysis was performed by using the RStudio software version 0.99.441 (www.rStudio.com).
Results
Study population and clinical manifestations
From January 1, 2005, to December 31, 2017, 47 patients fulfilled the inclusion criteria, including 28 (60%) with AS syndrome (Jo-1 n = 13/28 (47%); PL7 n = 9/28 (32%); PL12 n = 4/28 (14%); EJ n = 2/28 (7%)) and 19 (40%) with aMDA-5 dermato-pulmonary syndrome. All the patients with aMDA-5 dermato-pulmonary syndrome were admitted after January 1, 2010. Demographical characteristics, main comorbidities and clinical manifestations are given in Table 1. Most of the patients had no comorbidity (n = 40/47, 85%). Median SAPSII and SOFA scores at the time of ICU admission were 35 [27–53] and 5 [3–8], respectively. The median delay between first respiratory sign and ICU admission was 21 [10–41] days. Most of the patients had central temperature > 38 °C (n = 27/47, 57%). Myalgia, arthralgia/arthritis and cutaneous manifestations occurred in 23% (n = 11/47), 30% (n = 14/47) and 43% (n = 20/47) of patients, respectively. About one-third of patients (n = 17/47, 36%) had no extra-pulmonary manifestation, in a similar proportion in aMDA-5 and AS groups.
Laboratory and radiological findings
Biological data at the time of ICU admission and radiological findings are reported in Table 2. C-reactive protein levels (N < 5 mg/L) were increased (139 [40–208] mg/L), while procalcitonine levels (N < 0.5 ng/mL) were not (0.30 [0.12–0.56] ng/mL). The rate of patients having creatine kinase plasma levels greater than 2 times the upper limit of normal laboratory range was 20% (n = 9/47) in the whole population, and only 31% (n = 8/28) in the AS group. The median PaO2/FiO2 ratio at ICU admission was 123 [83–147] mmHg.
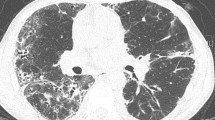
Most patients (n = 45/47, 96%) had bilateral condensations on chest X-ray, with a predominantly lower location (n = 46/47, 98%) (Table 2). All patients underwent a lung CT scan, which showed ground-glass attenuation in 78% (n = 37/47) and alveolar condensation in 75% (n = 35/47). Signs of lung fibrosis were observed in 36% (n = 17/47), while 38% (n = 18/47) had mediastinal lymphadenopathies.
Broncho-alveolar fluid analysis and histological data
BAL fluid analyses were available in 89% (n = 42/47) of patients and are summarized in Table 2. The cell count was 250 [140–330] × 103/mL, and percentages of lymphocytes, neutrophils and macrophages were 11% [4–30], 38% [13–65] and 40% [20–60], respectively. BAL was performed before antibiotic therapy in only 12/42 (29%) patients and was negative for lung infection in every patient. There was no correlation between BAL findings and elementary lesions observed on chest CT scan. In particular, the proportion of patients with > 40% BAL neutrophils did not differ between patients with or without elementary lesions of lung fibrosis on chest CT scan (n = 8/19, 42% vs. n = 11/19, 58%, p = 0.72). An open lung biopsy was performed in 4 (9%) patients and depicted findings consistent with organizing pneumonia (n = 2), usual interstitial pneumonitis (n = 1) and diffuse alveolar damage (n = 1) (Table 2). A total of 13 patients (28%) had a muscle (n = 7) or a skin (n = 6) biopsy performed during the ICU stay. All muscle biopsies revealed findings consistent with an inflammatory myositis, while skin biopsies were either normal (n = 1) or revealed findings consistent with lichenoid dermatitis (n = 3) or with dermatomyositis (n = 2) (Table 2).
ICU management and outcome
Most patients (n = 41/47, 89%) received an antimicrobial therapy upon ICU admission (Table 3). All patients received steroids, after a median delay of 6 [3–12] days following the ICU admission. Other immunosuppressive treatments administered are reported in Table 3.
Almost all patients (n = 42/47, 89%) had ARDS, categorized as severe (PaO2/FiO2 ≤ 100 mmHg with PEEP ≥ 5 mmH2O) in 86% (n = 36/47), with 17% (n = 8/47) of them requiring ECMO. ICU and hospital mortality rates were 45% (n = 21/47) and 51% (n = 24/47), respectively. Patients with aMDA-5 dermato-pulmonary syndrome had a higher ICU mortality than those with AS syndrome (n = 16/19, 84% vs. n = 5/28, 18%; p < 0.001). Among the 26 ICU survivors, 5 (19%) were diagnosed with a cancer (colorectal n = 3, pharyngeal n = 1, melanoma n = 1) during the 279 [158–500] days post-ICU stay follow-up.
Comparison between hospital survivors and non-survivors
Compared to patients who survived at the hospital discharge, those who died were more likely to have an aMDA-5 autoantibody (n = 16/24, 67% vs. n = 3/23, 13%; p = 0.001), had a higher rate of ground-glass attenuation (n = 22/24, 92% vs. 15/23, 65%; p = 0.04) and a lower rate of alveolar condensation (n = 14/24, 58% vs. 21/23, 91%; p = 0.02) on chest CT scan, and were given 3 [2, 3] versus 2 [1, 2] different immunosuppressive regimens during the ICU stay (p = 0.002) (Table 4). After adjustment on syndrome (anti-synthetase or aMDA-5 dermato-pulmonary syndrome), the presence of ground-glass attenuations on chest CT scan was no longer associated with in-hospital mortality (p = 0.24). The Kaplan–Meier graph showed a lower probability of survival 90 days after ICU admission in patients with aMDA-5 antibody than in patients with AS antibody (Fig. 1; p < 0.0001 log-rank test).
Discussion
We are herein reporting the first large cohort of patients admitted to ICU for ARF revealing either AS or aMDA-5 dermato-pulmonary syndrome. The main findings are: (1) clinical manifestations may be nonspecific with the absence of extra-pulmonary manifestations of inflammatory myositis in one-third of patients; (2) hypoxemia is severe with a high rate of severe ARDS and rescue maneuvers; and (3) hospital mortality is high, especially in dermato-pulmonary syndrome associated with aMDA-5 autoantibodies.
AS and aMDA-5-associated dermato-pulmonary syndromes are two near each of the other inflammatory myopathies that may be responsible for severe acute interstitial lung diseases [9,10,11]. The diagnosis is easy to consider when extra-pulmonary manifestations are present. In AS syndrome, the main extra-pulmonary manifestations include myositis with elevated creatine kinase levels, non-erosive arthritis, Raynaud’s phenomenon and thick cracked skin over the tips and sides of the fingers called “mechanic’s hands” [27,28,29,30,31,32]. However, there is a wide heterogeneity in clinical manifestations depending on the causative AS autoantibody [33, 34]. In aMDA-5-associated dermato-pulmonary syndrome, the cutaneous manifestations (skin ulcerations or necrosis, facial erythema, mechanic’s hands, periungual telangiectasia, Gottron’s papules, Raynaud’s phenomenon) are in the forefront [10, 11, 35] and usually contrast with the absence of clinical signs of myositis (clinically “amyopathic myositis”). Demographical and clinical findings in our patients were in line with those recently reported in non-ICU patients with AS [22, 32, 34] or with aMDA-5 dermato-pulmonary syndromes [10].
Both in AS and aMDA-5 dermato-pulmonary syndromes, extra-pulmonary manifestations may be lacking [9, 10] rendering the diagnosis difficult to make. In our series, more than one-third of patients had no extra-pulmonary manifestations with a similar proportion in AS and aMDA-5 patients. This rate contrasts with the 10% rate recently reported [10] in patients with aMDA-5 dermato-pulmonary syndrome, reflecting the lack of training of intensivists for the clinical assessment of these patients and highlighting the need for a multidisciplinary approach. Considering the high proportion of patients lacking extra-pulmonary manifestations, the clinical presentation may mimic that of a “bilateral pneumonia without microbiological documentation.” Hence, 89% of our patients received antibiotic therapy at ICU admission. The presence of an intense inflammatory syndrome with increased C-reactive protein levels contrasting with the lack of elevation of serum procalcitonine could help intensivists appreciating the probability of an infectious process, this dissociation being highly suggestive of a non-infectious inflammatory process.
In our series, BAL was performed in 89% of patients. Unlike a recent work [3] showing that a lymphocytic BAL fluid was associated with better ICU survival in ARDS patients with no common risk factor, our study failed to identify any predictive role of BAL cytology on hospital survival. BAL fluid analysis does not seem a useful diagnostic tool for AS or aMDA-5 dermato-pulmonary syndromes, but should nevertheless be performed to rule out an alternative diagnosis, such as diffuse alveolar hemorrhage or active infection.
All included patients underwent chest CT scan. Interestingly, CT chest findings predominate in the lower lobes, which is consistent with a previous report [36]. CT scan signs of lung fibrosis have been recently shown to be associated with a poor outcome in patients with ARF related to interstitial lung diseases [37]. In our study, CT scan signs of lung fibrosis were not associated with hospital mortality, probably because of a lack of adequate power. While ground-glass opacities are usually considered as potentially reversible lung lesions during idiopathic pulmonary fibrosis [38, 39], these lesions were associated with in-hospital mortality in our study, probably because they were more frequently observed during aMDA-5 dermato-pulmonary syndromes. Indeed, this association was no longer observed after adjustment on the type of positive antibody (anti-synthetase or aMDA-5).
Our series underlines the severity of AS and aMDA-5 dermato-pulmonary syndrome, since 89% of patients fulfilled the Berlin criteria for ARDS [5], categorized as severe (PaO2/FiO2 ≤ 100 mmHg with PEEP ≥ 5 mmH2O) in 86% of cases. Anti-MDA-5 dermato-pulmonary syndromes exhibited a significantly higher mortality than AS syndromes, with almost all these patients dying in the ICU of refractory ARDS despite a high rate of ECMO (32%). Moreover, aMDA-5 patients had a much higher mortality than those with severe ARDS included in the lung safe study [7], highlighting the irreversibility of lung lesions despite immunosuppressive treatments. These results are in line with previous series, showing that refractory ARDS is the leading cause of mortality in aMDA-5 patients [10].
Whether our patients had a true ARDS (i.e., presence of diffuse alveolar damage (DAD), the histological hallmark of ARDS) or simply fulfilled the Berlin criteria while having a non-DAD histology is unknown. In fact, the Berlin definition of ARDS is not fully reliable for diagnosing DAD, and several non-DAD histological entities (such as lung fibrosis, organizing pneumonia, diffuse alveolar hemorrhage or lung tumoral infiltration) have been reported in patients fulfilling the clinical and radiological criteria for ARDS [1, 40,41,42]. Regarding the onset of lung injury, the Berlin definition of ARDS stipulates that “respiratory signs should occur (or worsen) within 7 days after an exposure to a common ARDS risk factor” (e.g., pneumonia, acute pancreatitis, aspiration of gastric content or extra-pulmonary sepsis). In our patients, the absence of a common risk factor for ARDS according to the Berlin definition together with delay between first respiratory sign and ICU admission exceeding 7 days (21 days) advocate more for an ARDS mimicker rather than for a real ARDS. However, a recent histological study revealed that 50% of patients with an acute decompensation of AS syndrome due to JO-1 autoantibody exhibited histological lesions of DAD [43].
In non-ICU patients, the prognosis of inflammatory myopathies depends on the severity of lung involvement [10, 22, 32, 44]. Treatment of interstitial lung disease associated with AS and aMDA-5 dermato-pulmonary syndromes is not standardized and based on case reports. Numerous immunosuppressive therapies are available (e.g., cyclophosphamide, methotrexate, azathioprine, mycophenolate mofetil, cyclosporine, tacrolimus, rituximab, basiliximab, intravenous immunoglobulins or plasma exchange) [9, 11, 14, 21, 45, 46], but high-dose corticosteroids remain the first-line therapy. Our study underlines the wide variations in the choice of immunosuppressive treatment even if the association corticosteroids–cyclophosphamide was administered in almost 3 over 4 patients. Patients with aMDA-5 received significantly more immunosuppressive drugs highlighting a higher severity.
Of note, 19% of ICU survivors developed cancer, in line with previous series of AS patients [47].
Limitations
Our study suffers from several limitations. First, we included a limited number of patients, inherent to the rarity of the disease. However, this is the first series on ARF revealing AS or aMDA-5 syndromes in an ICU context and our findings are consistent with previous reports. This limited number of patients precluded performing multivariable analyses and thus did not allow for adjusting the observed association between some variables and mortality with potential confounders. Second, the relationship between positive AS or aMDA-5 autoantibody and ARF is not proven. We therefore cannot exclude that some patients had a fortuitously positive autoantibody and that inflammatory myopathy was not the cause of ARF. However, this hypothesis appears unlikely since an alternative diagnosis for ARF had to be excluded, and all patients were treated with immunosuppressive therapies underlining the high degree of clinician’s suspicion. Third, because the patients were recruited over a 13-year period in 35 centers, ICU procedures were inevitably heterogeneous. Fourth, the prevalence of aMDA-5 dermato-pulmonary syndromes may have been underestimated during the study period since detection of aMDA-5 autoantibody was first described in 2005 [48] and was therefore routinely available only from 2010 in most of participating centers. Last, several classical predictors of mortality related to ventilation (tidal volume or driving pressure [49]) were not available as a result of a long-term retrospective design.
Clinical implications
Considering the high proportion of patients lacking extra-pulmonary manifestations and the nonspecific presentation mimicking that of a bilateral community-acquired pneumonia, we believe that ARF related to autoimmune inflammatory myopathies may be underdiagnosed. Hence, de Prost et al. recently showed that the diagnostic work-up performed in ARDS patients with no common risk factor was not comprehensive, with only 5% of patients having immunological tests [4]. The lack of screening for AS or aMDA-5 autoantibodies is probably one of the reasons why these diseases are underestimated. Therefore, when the etiology of ARF appears unclear, we recommend a more aggressive diagnostic work-up [6], including immunological tests in order to identify patients amenable to specific therapies.
A careful assessment of extra-pulmonary manifestations, such as cutaneous or articular signs, is crucial. While the presence of extra-pulmonary manifestations is highly suggestive, the 3-week delay between first respiratory signs and ICU admission, the absence of an obvious etiology for ARF, the presence of bi-basal consolidations on chest X-ray with an intense inflammatory process, contrasting with a low procalcitonin level together with the lack of microbiological documentation are the main clues to consider the diagnosis of AS or aMDA-5 syndromes in a patient without extra-pulmonary manifestation. To better assess the relevance of these signs, further prospective studies aiming at systematically screen for autoantibodies in ARDS without risk factors are needed. Once the diagnosis is made, the management is difficult and requires a multidisciplinary approach involving intensivists, pulmonologists, internists and rheumatologists in order to decide the best-individualized therapeutic strategy.
Conclusions
Intensivists should consider inflammatory myopathies, such as anti-synthetase syndrome and dermato-pulmonary syndrome associated with anti-MDA-5 antibodies, as a cause of acute respiratory failure when the etiology appears unclear. Extra-pulmonary manifestations are commonly lacking and an isolated lung involvement may reveal the disease. Hospital mortality is high, especially in aMDA-5 dermato-pulmonary syndrome.
Abbreviations
- ARDS:
-
acute respiratory distress syndrome
- ARF:
-
acute respiratory failure
- AS:
-
anti-synthetase
- aMDA-5:
-
anti-MDA-5 autoantibody
- BAL:
-
broncho-alveolar lavage
- DAD:
-
diffuse alveolar damage
- ECMO:
-
extra-corporeal membrane oxygenation
- ICU:
-
intensive care unit
References
Papazian L, Doddoli C, Chetaille B, Gernez Y, Thirion X, Roch A, et al. A contributive result of open-lung biopsy improves survival in acute respiratory distress syndrome patients. Crit Care Med. 2007;35:755–62.
Vincent JL, Santacruz C. Do we need ARDS? Intensive Care Med. 2012;42:282–3.
Gibelin A, Parrot A, Maitre B, Brun-Buisson C, Mekontso Dessap A, Fartoukh M, et al. Acute respiratory distress syndrome mimickers lacking common risk factors of the Berlin definition. Intensive Care Med. 2015;42:164–72.
de Prost N, Pham T, Carteaux G, Mekontso Dessap A, Brun-Buisson C, Fan E, et al. Etiologies, diagnostic work-up and outcomes of acute respiratory distress syndrome with no common risk factor: a prospective multicenter study. Ann Intensive Care. 2017;7:69.
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, et al. Acute respiratory distress syndrome: the Berlin definition. JAMA. 2012;307:2526–33.
Papazian L, Calfee CS, Chiumello D, Luyt CE, Meyer NJ, Sekiguchi H, et al. Diagnostic workup for ARDS patients. Intensive Care Med. 2016;42:674–85.
Bellani G, Laffey JG, Pham T, Fan E, Brochard L, Esteban A, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800.
Hall JC, Casciola-Rosen L, Samedy LA, Werner J, Owoyemi K, Danoff SK, et al. Anti-melanoma differentiation-associated protein 5-associated dermatomyositis: expanding the clinical spectrum. Arthritis Care Res (Hoboken). 2013;65:1307–15.
Tillie-Leblond I, Wislez M, Valeyre D, Crestani B, Rabbat A, Israel-Biet D, et al. Interstitial lung disease and anti-Jo-1 antibodies: difference between acute and gradual onset. Thorax. 2008;63:53–9.
Uzunhan Y, Nunes H, Leroux G, Miyara M, Benveniste O, Allenbach Y. Dermato-pulmonary syndrome associated with MDA-5 antibodies. Eur Respir J. 2016;48(suppl 60):2138.
Chaisson NF, Paik J, Orbai AM, Casciola-Rosen L, Fiorentino D, Danoff S, et al. A novel dermato-pulmonary syndrome associated with MDA-5 antibodies: report of 2 cases and review of the literature. Medicine (Baltimore). 2012;91:220–8.
Grasselli G, Vergnano B, Pozzi MR, Sala V, D’Andrea G, Scaravilli V, et al. Interstitial pneumonia with autoimmune features: an additional risk factor for ARDS? Ann Intensive Care. 2017;7:98.
Bizien N, Renault A, Boles JM, Delluc A. Acute interstitial lung disease revealing antisynthetase syndrome. Rev Pneumol Clin. 2011;67:367–70.
Guglielmi S, Merz TM, Gugger M, Suter C, Nicod LP. Acute respiratory distress syndrome secondary to antisynthetase syndrome is reversible with tacrolimus. Eur Respir J. 2008;31:213–7.
Kim SH, Park IN. Acute respiratory distress syndrome as the initial clinical manifestation of an antisynthetase syndrome. Tuberc Respir Dis (Seoul). 2016;79:188–92.
Clawson K, Oddis CV. Adult respiratory distress syndrome in polymyositis patients with the anti-Jo-1 antibody. Arthritis Rheum. 1995;38:1519–23.
Piroddi IM, Ferraioli G, Barlascini C, Castagneto C, Nicolini A. Severe respiratory failure as a presenting feature of an interstitial lung disease associated with anti-synthetase syndrome (ASS). Respir Investig. 2016;54:284–8.
Friedman AW, Targoff IN, Arnett FC. Interstitial lung disease with autoantibodies against aminoacyl-tRNA synthetases in the absence of clinically apparent myositis. Semin Arthritis Rheum. 1996;26:459–67.
Shi J, Li S, Yang H, Zhang Y, Peng Q, Lu X, et al. Clinical profiles and prognosis of patients with distinct antisynthetase autoantibodies. J Rheumatol. 2017;44:1051–7.
Kinebuchi S, Mizuno K, Moriyama H, Ooi H, Hasegawa T, Yoshizawa H, et al. Two cases of interstitial pneumonia with anti-Jo-1 antibodies in the absence of myositis. Nihon Kokyuki Gakkai Zasshi. 2003;41:739–45.
Sauty A, Rochat T, Schoch OD, Hamacher J, Kurt AM, Dayer JM, et al. Pulmonary fibrosis with predominant CD8 lymphocytic alveolitis and anti-Jo-1 antibodies. Eur Respir J. 1997;10:2907–12.
Hervier B, Wallaert B, Hachulla E, Adoue D, Lauque D, Audrain M, et al. Clinical manifestations of anti-synthetase syndrome positive for anti-alanyl-tRNA synthetase (anti-PL12) antibodies: a retrospective study of 17 cases. Rheumatology (Oxford). 2010;49:972–6.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–10.
Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute physiology score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–63.
Wettstein RB, Shelledy DC, Peters JI. Delivered oxygen concentrations using low-flow and high-flow nasal cannulas. Respir Care. 2005;50:604–9.
Coudroy R, Frat JP, Boissier F, Contou D, Robert R, Thille AW. Early identification of acute respiratory distress disorder in the absence of positive pressure ventilation: implications for revision of the berlin criteria for acute respiratory distress syndrome. Crit Care Med. 2017;46:540–6.
Connors GR, Christopher-Stine L, Oddis CV, Danoff SK. Interstitial lung disease associated with the idiopathic inflammatory myopathies: what progress has been made in the past 35 years? Chest. 2010;138:1464–74.
Imbert-Masseau A, Hamidou M, Agard C, Grolleau JY, Cherin P. Antisynthetase syndrome. Joint Bone Spine. 2003;70:161–8.
Schmidt WA, Wetzel W, Friedlander R, Lange R, Sorensen HF, Lichey HJ, et al. Clinical and serological aspects of patients with anti-Jo-1 antibodies—an evolving spectrum of disease manifestations. Clin Rheumatol. 2000;19:371–7.
Hengstman GJ, van Engelen BG, van Venrooij WJ. Myositis specific autoantibodies: changing insights in pathophysiology and clinical associations. Curr Opin Rheumatol. 2004;16:692–9.
Marguerie C, Bunn CC, Beynon HL, Bernstein RM, Hughes JM, So AK, et al. Polymyositis, pulmonary fibrosis and autoantibodies to aminoacyl-tRNA synthetase enzymes. Q J Med. 1990;77:1019–38.
Marie I, Josse S, Decaux O, Diot E, Landron C, Roblot P, et al. Clinical manifestations and outcome of anti-PL7 positive patients with antisynthetase syndrome. Eur J Intern Med. 2013;24:474–9.
Vazquez-Abad D, Rothfield NF. Sensitivity and specificity of anti-Jo-1 antibodies in autoimmune diseases with myositis. Arthritis Rheum. 1996;39:292–6.
Marie I, Josse S, Decaux O, Dominique S, Diot E, Landron C, et al. Comparison of long-term outcome between anti-Jo1- and anti-PL7/PL12 positive patients with antisynthetase syndrome. Autoimmun Rev. 2012;11:739–45.
Fiorentino D, Chung L, Zwerner J, Rosen A, Casciola-Rosen L. The mucocutaneous and systemic phenotype of dermatomyositis patients with antibodies to MDA5 (CADM-140): a retrospective study. J Am Acad Dermatol. 2010;65:25–34.
Zamora AC, Hoskote SS, Abascal-Bolado B, White D, Cox CW, Ryu JH, et al. Clinical features and outcomes of interstitial lung disease in anti-Jo-1 positive antisynthetase syndrome. Respir Med. 2016;118:39–45.
Zafrani L, Lemiale V, Lapidus N, Lorillon G, Schlemmer B, Azoulay E. Acute respiratory failure in critically ill patients with interstitial lung disease. PLoS ONE. 2014;9:e104897.
Gay SE, Kazerooni EA, Toews GB, Lynch JP 3rd, Gross BH, Cascade PN, et al. Idiopathic pulmonary fibrosis: predicting response to therapy and survival. Am J Respir Crit Care Med. 1998;157:1063–72.
Wells AU, Desai SR, Rubens MB, Goh NS, Cramer D, Nicholson AG, et al. Idiopathic pulmonary fibrosis: a composite physiologic index derived from disease extent observed by computed tomography. Am J Respir Crit Care Med. 2003;167:962–9.
Thille AW, Esteban A, Fernandez-Segoviano P, Rodriguez JM, Aramburu JA, Penuelas O, et al. Comparison of the Berlin definition for acute respiratory distress syndrome with autopsy. Am J Respir Crit Care Med. 2013;187:761–7.
Patel SR, Karmpaliotis D, Ayas NT, Mark EJ, Wain J, Thompson BT, et al. The role of open-lung biopsy in ARDS. Chest. 2004;125:197–202.
Gerard L, Bidoul T, Castanares-Zapatero D, Wittebole X, Lacroix V, Froidure A, et al. Open lung biopsy in nonresolving acute respiratory distress syndrome commonly identifies corticosteroid-sensitive pathologies, associated with better outcome. Crit Care Med. 2018;46:907–14.
Yousem SA, Gibson K, Kaminski N, Oddis CV, Ascherman DP. The pulmonary histopathologic manifestations of the anti-Jo-1 tRNA synthetase syndrome. Mod Pathol. 2010;23:874–80.
Marie I, Hachulla E, Cherin P, Dominique S, Hatron PY, Hellot MF, et al. Interstitial lung disease in polymyositis and dermatomyositis. Arthritis Rheum. 2002;47:614–22.
Witt LJ, Curran JJ, Strek ME. The diagnosis and treatment of antisynthetase syndrome. Clin Pulm Med. 2016;23:218–26.
Zou J, Li T, Huang X, Chen S, Guo Q, Bao C. Basiliximab may improve the survival rate of rapidly progressive interstitial pneumonia in patients with clinically amyopathic dermatomyositis with anti-MDA5 antibody. Ann Rheum Dis. 2014;73:1591–3.
Castaneda-Pomeda M, Prieto-Gonzalez S, Grau JM. Antisynthetase syndrome and malignancy: our experience. J Clin Rheumatol. 2011;17:458.
Sato S, Hirakata M, Kuwana M, Suwa A, Inada S, Mimori T, et al. Autoantibodies to a 140-kd polypeptide, CADM-140, in Japanese patients with clinically amyopathic dermatomyositis. Arthritis Rheum. 2005;52:1571–6.
Amato MB, Meade MO, Slutsky AS, Brochard L, Costa EL, Schoenfeld DA, et al. Driving pressure and survival in the acute respiratory distress syndrome. N Engl J Med. 2015;372:747–55.
Authors’ contributions
DC had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. DC made substantial contribution to the study design, data collection and analysis and manuscript writing. CV contributed to data collection and interpretation, and drafting of the manuscript. MPC, NdP, AD, J-PQ, SP, GL, MN, GV, MF, RC, GD, EM, NT, YT-L, FS, MG, EG, RL, SR, RLM, GC, CG, LZ and EM contributed to patients identification in each center, data collection and manuscript writing. MD contributed to the data analysis, statistical analysis and manuscript revision. NdP, CG, OP, HM and GP contributed to the manuscript writing and revision, and provided important intellectual content. All authors read and approved the final manuscript.
Acknowledgements
We thank Jonathan Messika (Réanimation, Hôpital Louis Mourier, Colombes), Frédéric Pène (Réanimation médicale, Hôpital Cochin, Paris), Morgan Benaïs (Réanimation médico-chirurgicale, Saint Denis), Jérémy Rosman (Réanimation polyvalente, Charleville), David Schnell (Réanimation médico-chirurgicale, Angoulême), Sébastien Jochmans (Réanimation Polyvalente, Melun), Sami Hraiech and Jérémy Bourenne (Réanimations, Marseille), Guillaume Schnell (Réanimation médico-chirurgicale, Le Havre), Damien Du Cheyron (Réanimation médicale, Caen), Aude Gibelin (Réanimation médico-chirurgicale, Hôpital Tenon, Paris), Cédric Bruel (Réanimation Polyvalente, Hôpital Saint-Joseph, Paris), Kamel Toufik (Réanimation médico-chirurgicale, Orléans) and Jérémie Lemarié (Réanimation, Nancy) for having searched for eligible patients.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The study was approved by Institutional Review Board of the French Society for Respiratory Medicine in September 2017 (CEPRO 2017-32), which waived informed consent.
Funding
This study did not receive funding from external or internal sources.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Vuillard, C., Pineton de Chambrun, M., de Prost, N. et al. Clinical features and outcome of patients with acute respiratory failure revealing anti-synthetase or anti-MDA-5 dermato-pulmonary syndrome: a French multicenter retrospective study. Ann. Intensive Care 8, 87 (2018). https://doi.org/10.1186/s13613-018-0433-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-018-0433-3