Abstract
Introduction
Approximately half of oral cancers are detected in advanced stages. The current gold standard is histopathological assessment of biopsied tissue, which is subjective and dependent on expertise. Straticyte™, a novel prognostic tool at the pre-market stage, that more accurately identifies patients at high risk for oral cancer than histopathology alone. This study conducts an early cost-effectiveness analysis (CEA) of Straticyte™ and histopathology versus histopathology alone for oral cancer diagnosis in adult patients.
Methods
A decision-analytic model was constructed after narrowing the scope of Straticyte™, and defining application paths. Data was gathered using the belief elicitation method, and systematic review and meta-analysis. The early CEA was conducted from private-payer and patient perspectives, capturing both direct and indirect costs over a five-year time horizon. One-way and probabilistic sensitivity analyses were conducted to investigate uncertainty.
Results
Compared to histopathology alone, histopathology with Straticyte™ was the dominant strategy, resulting in fewer cancer cases (31 versus 36 per 100 patients) and lower total costs per cancer case avoided (3,360 versus 3,553). This remained robust when Straticyte™ was applied to moderate and mild cases, but became slightly more expensive but still more effective than histopathology alone when Straticyte™ was applied to only mild cases. The probabilistic and one-way sensitivity analyses demonstrated that incorporating Straticyte™ to the current algorithm would be cost-effective over a wide range of parameters and willingness-to-pay values.
Conclusion
This study demonstrates high probability that Straticyte™ and histopathology will be cost-effective, which encourages continued investment in the product. The analysis is informed by limited clinical data on Straticyte™, however as more data becomes available, more precise estimates will be generated.
Similar content being viewed by others
Background
Economic evaluations (EEs) are increasingly used to inform decisions of healthcare resource allocation for interventions, including drugs and medical devices [1]. EEs, primarily cost-effectiveness analyses (CEA), are done for reimbursement in the late stages (i.e. post-market) of an intervention’s development. Reimbursement facilitates wide implementation in clinical practice, which improves return on investment and patients’ access to care. Recently, there has been interest in conducting early (i.e. pre-market) CEA, which gives companies feedback from content experts and stakeholders during their development and pre-market process [2]. Early CEA better prepares the company for licensing and adoption of the product, and may increase the likelihood of reimbursement by building a stronger evidence portfolio [2, 3]. Late CEA is a one-time process, whereas early CEA is iterative [4]. There are currently no guidelines in place on conducting early CEA, however several qualitative and quantitative approaches have been proposed (Additional file 1: Table S1).
Oral cancer encompasses cancers of the lip, oral cavity, or oropharynx, and accounts for 3% of all cancers worldwide [5, 6]. Though less common in Canada, 4100 new cases were estimated in 2013. The overall incidence in Canada is an estimated 12 cases per 100,000 people per year in men, and 5 per 100,000 in women [7, 8]. Up to 50% of oral cancers are not detected until the disease is well advanced and the overall survival rate, five years after diagnosis, is about 62% [6, 8]. Mortality can be reduced if treatment is initiated at an early stage, thus early diagnosis is critical.
The current gold standard for diagnosis is histopathologic assessment of a tissue biopsy, which is subjective. Straticyte™, a biomarker, is a novel prognostic tool for oral cancer. Based on an evaluation of 107 cases of dysplasia, with up to 10 years of follow-up, Straticyte™ and histopathology demonstrated improvement in both the positive predicted value (PPV) and the negative predicted (NPV) value by 10% and 27%, respectively, compared to histopathology alone, thus more accurately identifying patients at high risk [9]. Starticyte™ is first in its class, however, there is limited data regarding its effectiveness, potential use in clinical practice, and costing estimates.
Accurate predictions of true oral cancer could save lives, reduce morbidity with less traumatic surgeries, increase the duration of productive work lives, and save healthcare costs [10, 11]. Support for its adoption rests on demonstrating value for money, as Straticyte™ will require an investment by private sectors, since public payers do not cover it. Based on the CEA, the manufacturer, healthcare system, and individual patient will be informed whether investing in this product is worthwhile. The aim of this study is to conduct an early CEA of adding Straticyte™ to the current standard of care for diagnosing malignant oral lesions in adults.
Methods
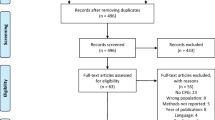
The development of the economic model to determine the cost-effectiveness of Straticyte™ is summarized in Fig. 1 and described below.
The three key steps followed to conduct early cost-effectiveness analysis. Step#1:Narowing the scope of the economic evaluation, building a conceptual economic model and drafting scenarios for the new prognostic tool (i.e. Straticyte™); Step #2: Inventory of available evidence from internal unpublished resources, systematic review and meta-analysis as well as by utilizing belief elicitation methods to gather scarce evidence where necessary; Step#3: Determining the cost-effectiveness of the Straticyte™ by conducting a base case analysis, scenario analyses and sensitivity analyses (at least deterministic given scarce evidence)
Step #1: Scope, conceptual economic model and scenario drafting
Scope
The potential application of Starticyte™ in the healthcare system has been assessed through a comprehensive literature search and discussions with test developers, clinicians, and experts in the field of oral cancer. Using this information and the limited available evidence on Straticyte™, we narrowed the scope of this CEA by defining the Application, Population, Comparator, Outcome, and Intervention (APCOI) (Additional file 1: Table S2) [4]. This CEA was conducted over a time horizon of five-years and from private payer’s and patient’s perspectives, to capture all relevant differences in future direct and indirect costs and outcomes associated with oral pre-cancer.
Conceptual economic model
A five-year CEA was conducted using a decision analytic tree to determine whether a prognostic algorithm for oral cancer that includes Stratictye™ compared to Histopathology alone in Canada is cost-effective. The model was build using Microsoft Excel® based on four key assumptions (Additional file 1: Table S3) and consists of two arms (Additional file 1: Figure S1). The future costs and outcomes that occur beyond one year associated with both arms were discounted at an annual rate of 5% [12].
Scenario drafting
Straticyte™ indication is not yet finalized, different application paths for Straticyte™ are possible, hence scenario drafting [13] was used to assess the dynamic aspects of this health technology. In addition to the base case analysis, the effect, cost and cost-effectiveness of two additional possible scenarios where “Straticyte™” can successfully be applied were also explored.
Step #2: Inventory of available evidence and additional data collection on histopathology and Straticyte™
The model parameters in Table 1 were gathered from published clinical and economic literature, grey literature, and expert opinion.
Probabilities
The data used in this model was derived from a retrospective study of 107 cases of dysplasia in Canada [14]. Oral dysplasia biopsy samples were assembled from archives of an oral pathology laboratory [14]. All subjects with histopathological evidence of dysplasia and follow-up information for at least five-years were included. The two primary clinical outcomes were dysplasia progression to cancer, and time in months of dysplasia progression to cancer. This cancer cases were outcomes from patients who have not undergone excision (i.e. surgery) [14]. The uncertainty in probabilities of going from one health state to another was modeled using both Dirichlet and Beta distribution for the purpose of probabilistic sensitivity analysis (PSA) [15]. Where there was a count of zero cancer cases we did not sample from the Dirichlet distribution, instead we assumed constant zero. This was done since there was no information (i.e. observation) on the probability of developing oral cancer in the retrospective study [14].
Relative risk (RR) of malignant transformation
To inform the parameter of RR of developing cancer given treatment modality (i.e. relative risk of developing cancer given patients have undergone excision vs. no excision), we conducted a comprehensive systematic literature search to identify clinical studies that investigated the malignant transformation rate (MTR) given treatment modality (Additional file 1: Table S3). The MTRs from the included studies were pooled and the RR of malignant transformation over 5 years was determined using the Cochrane Collaboration Review Manager analysis version 5.2 Statistical Software (RevMan 5.2). The methodology and detailed results of this review can be found in Additional file 1: Figure S2, S3 and Additional file 1: Table S4, S5.
Clinical practice by oral and maxillofacial (O&M) surgeons
The belief elicitation method was used to determine the potential impact of Straticyte™ on clinical practice [16]. Our objective was to determine how O&M surgeons would treat patients with oral dysplasia given the results from Straticyte™ and histopathology versus histopathology alone. Questionnaires (Additional file 1: Table S5) were administered face-to-face, requiring 15–30 min to complete, to four O&M surgeons with a minimum of five years of experience in treating patients with oral pre-cancerous lesions (Additional file 1: Table S6). A standardized script was used, explaining the process and the purpose. Questions were prepared with the help of a clinician, and clarified with participants. The outcomes of the elicitation (Additional file 1: Table S7) dictated where in the decision tree (i.e. which branch) the RR of developing oral cancer given excision and the associated costs and resources are applied.
Costs and resources
The costs and resource utilizations were gathered from several sources (Table 1). All costs are reported in 2014 CAD, and, if necessary, were corrected by the Canadian consumer price inflation index using the Bank of Canada online inflation calculator [17]. The direct costs associated with the intervention and illness included in this CEA was as follows: oral biopsy (excision, following-up patients), pathology (technician, preparation of report), Straticyte™ (running the test, technician, reporting the outcome, administrative cost of O&M surgeon and pathologist), pain medication, and gingivitis treatment (Additional file 1: Table S8). The main indirect costs that were included in this CEA were the costs associated with absenteeism from work and transportation costs, included the cost of travel and parking [18, 19].
Step #3: Early cost-effectiveness data analysis
Base case and exploratory scenario analyses
CEAs were conducted in both base-case and scenario cases. This CEA investigated the costs associated with cancer cases avoided. The incremental cost is compared to the incremental health effects [20]. In the base-case scenario, this was the number of cancer cases avoided given the application of Straticyte™ to all three categories (i.e. Severe, Moderate, Mild) classified by histopathology. In addition, we explored the effect, cost, and cost-effectiveness of two alternative scenarios where “Straticyte™” can be applied. For exploratory scenario #1, we examined the number of cancer cases avoided when Straticyte™ was applied to two categories, moderate and mild cases, and for exploratory scenario #2, we examined cases avoided when Straticyte™ was applied to only mild cases.
Sensitivity analyses
To explore the uncertainty around parameters in the model to find the inputs with the largest impact on the model outcome, one-way sensitivity analyses (OWSA) and probabilistic sensitivity analyses (PSA) were conducted [15]. OWSA provides insight into alternative values for specific parameters that could make a meaningful impact on the model outcome and on the potential decision based upon it. Given this, OWSA was conducted for some of the fixed parameters such as the discount rate, number of follow-ups in a year. The upper and lower values for all included parameters were obtained from published literature. If not available, the mean ± 20% was considered a reasonable range to evaluate a model parameter in the deterministic model. Furthermore, PSA was conducted to take account the overall uncertainty from the combined variability of several factors. A Monte Carlo (MC) simulation method was used to compute the results [15]. A total of 5000 simulations were completed given the fact that early CEAs have an additional level of uncertainty due to limited evidence on Straticyte™ [15]. Additionally, the collective uncertainty of all of the parameters serves to generate uncertainty at the decision making level. Hence, the net monetary benefit (NMB) approach was used to characterize the decision uncertainty and results presented in a cost-effectiveness acceptability curve (CEAC) [15].
Results
Base-case analysis
The incorporation of Straticyte™ into the current prognostic algorithm (i.e. histopathology) was cost saving as it led to a slightly lower per patient cost and fewer cancer cases over a five-year time horizon compared to histopathology alone (3,360 versus 3,553, and 31 versus 36 per 100 patients, respectively) (Table 2). The histopathology and Straticyte™ prognostic algorithm was determined to be the dominant strategy (more effective and less costly).
Exploratory scenario analyses
Given that Straticyte™ is not in the market place yet and its indication is not finalized, its cost-effectiveness was assessed when it was only applied to moderate and mild cases (scenario #1) (Table 3). The incorporation of Straticyte™ remained the dominant strategy in scenario #1 (3,192 versus 3,551, and 28 cancer cases versus 35 cancer cases per 100 patients Straticyte™ and histopathology versus histopathology alone, respectively). However, when Straticyte™ was only used for cancer cases (i.e. scenario #2), it no longer was the dominant strategy. Over a five-year time horizon, Straticyte™ and histopathology was the more expensive approach albeit still more effective than histopathology alone for an ICER of $8610/cancer cases avoided (Table 3).
Sensitivity analyses
One-way sensitivity analysis
In almost all cases explored in the OWSA, Straticyte™ and histopathology was cost saving (more effective and cheaper) compared to histopathology alone. Changes in several parameters, such as the number of visits per year specifically, by applying only 2 visits per year (i.e. every 6 months instead of 3 to the moderate group in histopathology group), relative risk of malignant transformation and probability of developing cancer from mild dysplasia, were found to have meaningful impact on the model outcome. In all three of these cases, the incorporation of Straticyte™ was associated with slightly higher costs but still better outcomes than histopathology alone.
Probabilistic sensitivity analysis
The CEAC was constructed using MC simulation to demonstrate decision uncertainty. In this study, the CEAC explored the probability of Straticyte™ and histopathology having the greatest net benefit compared to histopathology alone over a range of potential willingness to pay (WTP) thresholds (Fig. 2). At the lowest WTP threshold, Straticyte™ and histopathology was the more cost-effective strategy (89% of the simulations) than histopathology alone (11% of the stimulations). With higher thresholds, the probability in which Straticyte™ and histopathology was the cost-effective option (i.e. the most attractive option) decreased slightly reaching a horizontal asymptote, whereby it offered the highest net benefit in 84% of the simulations (Fig. 2).
The cost-effectiveness acceptability curve (CEAC) of the early economic evaluation of the new prognostic tool, Straticyte™. Net monetary benefit is used to determine which treatment was cost-effective for each simulation at different willingness to pay thresholds (WTPs) for cancer cases avoided given the use of Staricyte™ (i.e. biomarker) in combination with the standard of care (i.e. Histopathology)
Discussion
Principal findings
In the base case analysis from the private payers and patient's perspectives, the algorithm of Straticyte™ and histopathology dominated the current standard of care (SOC), by incurring lower cost and less cancer cases developed over five-years. Uncertainty was considered in this economic model through several sensitivity analyses, for which the results remained robust. The majority of ICER values obtained from all investigated parameters kept the algorithm with Straticyte™ the dominant strategy, suggesting that it leads to better outcomes and is less expensive than current practices. The model parameters, number of visits per year, relative risk of MT, and probability of developing cancer from mild dysplasia led to less cancer cases, though was slightly more expensive. However, the cost-difference was less than $10,000/QALY, which is substantially lower than the commonly quoted Canadian threshold of $100,000/QALY for the field of oncology, thus remains cost-effective. PSA allowed us to determine the overall impact of the model inputs on the outcome of interest. The result obtained from this analysis was very close to the base-case analysis, where the algorithm with Straticyte™ was the dominant approach. The CEAC curve generated from the MC simulation demonstrated that the algorithm with Straticyte™ always had a higher probability of being cost-effective. However, the curve illustrates that there is a slight gap in the available evidence to inform decision-makers to adopt the new technology, since it had less than 100% probability of being cost-effective at very high WTP thresholds. This is not surprising given that Straticyte™ data is currently limited. As more information is gathered and estimates become more precise, they would progressively fill in this gap, allowing for continuous reassessment and strengthening of the economic output of the model.
Study in context of relevant literature
There have been no previous CEA of Straticyte™ and literature on early CEA is limited. Recently, a few studies have presented general overview of methods to conduct early CEA and briefly applied suggested methods into the process of late CEA to demonstrate their potential usefulness in conducting early CEA [3, 5, 13, 16, 21,22,23,24]. The literature highlights that integration of health economic modeling into early decision is not extensively practiced in pharmaceutical industry, and nearly absent for devices [25]. In pharmaceutical companies, CEAs are mostly conducted for marketing and reimbursement purposes versus research and development, despite the fact that economic factors are usually considered the second leading cause for research termination of an early technology [26, 27].
Limitations and strengths
This early CEA is associated with several limitations. First, there is a paucity of high level clinical evidence regarding the effectiveness of Straticyte™, which is the nature of conducting any kind of analysis at a product’s early stages of development [4]. We attempted to account for this by conducting several sensitivity analyses to test our assumptions of effectiveness and clinical use. Second, methods used in this early economic analysis are vaguely described in the literature and are commonly only pilot studies [3, 13, 16, 21,22,23,24]. Given the nature of this analysis, these methods can be conceptually challenging and rely highly on a number of assumptions [28, 29]. This makes the results very susceptible to critique by experts in the field pertaining to the technology, despite attempts to account for these assumptions through sensitivity analyses. To ensure clinical relevance, we sought expert advice throughout the evaluation process to help identify gaps and provide direction. Lastly, since some of the information such as the frequency of follow-ups was inputs by experts’ opinion based on their everyday practice, stricter follow-up (3 months vs. 6 months) could potential be more effective over long-term in identifying new pre-cancerous lesions, recurrences, which may have resulted in improved outcomes due to earlier treatment. Therefore, another major limitation of this study was not considering the potential additional benefits due to stricter follow-up by O&M surgeons. This paper has several strengths. First, we conducted an extensive review of the literature to identify methodologies of early CEA (Khoudigian-Sinani et al. manuscript in preparation). Second, we sought clinical expert opinions as well as opinions of leaders in HTA to inform our analyses. Third, we are the first to incorporate multiple methods that were suggested and piloted in the literature to complete a thorough early CEA to determine the potential value of Straticyte™.
Implications for clinicians and policymakers
The considerable burden of disease and expense of oral cancer in Canada highlights the importance of accurately predicting the risk of developing oral cancer to both patients and the health care system [5]. Straticyte™, is at its early pre-market stage of its lifecycle, hence this was an attempt to compare the costs and outcomes of incorporating it to the current prognostic algorithm using limited data related to its clinical use and effectiveness. Decision analytical modeling techniques as well as qualitative methods, such as belief elicitation method and scenario drafting, were applied, and parameters for which the model outcome is most sensitive was explored. This provides a thorough early CEA that is important for clinicians and policymakers to consider. Furthermore, whilst presenting a successful attempt in early modeling and the difficulties associated with it, this paper creates a potential foundation to work on and build a guiding framework in creating more robust early models, with useful insight into the potential value of the product at that moment as well as meet the requirements of fully developed models at late stages of the product’s life cycle.
Unanswered questions and future research considerations
Canadian policy makers have to make informed decisions on how to allocate resources for the population in the most efficient manner, given increasing health expenditures and scarce resources [1]. These decisions generally are based on both clinical and cost-effectiveness evidence of new health technologies compared with standard care or alternative technologies [1]. Even though cost-effectiveness analysis within health technology assessment has long been recognized as a compelling way to ascertain value for buyers, its role in the allocation of research and development by companies is not well described. There is no set guideline that helps guide on how to conduct CEAs during the early stages of a technology’s development life cycle and how to deal with challenges associated with the lack of both clinical and economic evidence. Despite the development in health economic methods to support reimbursement after the product is in the market place, the use of CEA at the early stages of product’s development is less explored and needs further research.
Conclusion
This early CEA demonstrates a high probability of success that Straticyte™ will be cost-effective. This supports continued investment by the manufacturer, and that investment by the healthcare system and individual patients may be worthwhile. Data is currently limited, and as the product cycle progresses, additional information will inform the model and provide more accurate estimates of the technology’s cost effectiveness.
Abbreviations
- APCOI:
-
Application, population, comparator, outcome, intervention
- CAD:
-
Canadian
- CEA:
-
Cost-effectiveness analysis
- CEAC:
-
Cost-effectiveness acceptability curve
- EE:
-
Economic evaluation
- ICER:
-
Incremental cost-effectiveness ratio
- MC:
-
Monte Carlo
- MT:
-
Malignant transformation
- MTR:
-
Malignant transformation rate
- NMB:
-
Net monetary benefit
- NPV:
-
Negative predictive value
- O&M:
-
Oral and maxillofacial
- OWSA:
-
One-way sensitivity analysis
- PPV:
-
Positive predictive value
- PSA:
-
Probabilistic sensitivity analysis
- QALY:
-
Quality adjusted life years
- RR:
-
Relative risk
- WTP:
-
Willingness to pay threshold
References
Eddama O, Coast J. A systematic Review of the use of economic evaluation in local decision-making. Health Policy. 2008;86(2):129–41.
Vallejo-Torres L, Steuten L, Parkinson B, Girling AJ, Buxton MJ. Integrating Health Economics Into the Product Development Cycle A Case Study of Absorbable Pins for Treating Hallux Valgus. Med Decis Mak. 2011;31(4):596–610.
Haakma W, Steuten LM, Bojke L, IJzerman MJ. Belief Elicitation to Populate Health Economic Models of Medical Diagnostic Devices in Development. Appl Health Econ Health Policy. 2014;12(3):327–34.
Buisman LR, Rutten-van Mölken MP, Postmus D, Luime JJ, Uyl-de Groot CA, Redekop WK. The early bird catches the worm: early cost-effectiveness analysis of new medical tests. Int J Technol Assess. 2016;32(1-2):46-53.
Lingen MW, Kalmar JR, Karrison T, Speight PM. Critical evaluation of diagnostic aids for the detection of oral cancer. Oral Oncol. 2008;44(1):10–22.
Ford PJ, Farah CS. Early detection and diagnosis of oral cancer: Strategies for improvement. J Cancer Policy. 2013;1(1):e2–7.
Canadian Cancer Society. Canadian Cancer Statistics: Oral cavity cancer statistics: Toronto. http://www.cancer.ca/en/cancer-information/cancer-type/oral/statistics/?region=on. Published 2017. Accessed Dec 2015.
Laronde DM, Hislop TG, Elwood JM, Rosin MP. Oral cancer: just the facts. J Can Dent Assoc. 2008;74(3):269–72.
Alyass A. A quantitative risk assessment model for progression of oral dysplasia to cancer. Toronto: Mitacs-Accelerate; 2013.
Kao SY, Ya-Wei C, Kuo-Wei C, Tsung-Yun L. Detection and screening of oral cancer and pre-cancerous lesions. J Chin Med Assoc. 2009;72(5):227–33.
Warnakulasuriya S, Jesper R, Bouquot J, Dabelsteen E. Oral epithelial dysplasia classification systems: predictive value, utility, weaknesses and scope for improvement. J Oral Pathol Med. 2008;37(3):127–33.
Canadian Agency for Drugs and Technology in Health. Guidelines for economic evaluation of health technologies: Canada, 3rd Ed. Ottawa: Canadian Agency for Drugs and Technology in Health (CADTH); 2006.
Chapman AM, Taylor CA, Girling AJ. Early HTA to inform medical device development decisions-the headroom method. In XIII Mediterr Conf Med Biol Eng Comput. 2014:1151–4.
Proteocyte Diagnostic Inc. Straticyte™ oral cancer test- technology and application: Improved accuracy for confidence in clinical decisions and better outcome. Toronto. 2013.
Briggs A, Claxton K, Sculpher M. Decision Modeling for Health Economic Evaluation. Chapter #4: Making Decision Models Probabilistic. New York, NY: Oxford University Press; 2006.
Retèl VP, Joore MA, Linn SC, Rutgers EJ, Van Harten WH. Scenario drafting to anticipate future developments in technology assessment. BMC Res Notes. 2012;5(1):1.
Inflation Calculator. Consumer Price Index for Canada. http://www.bankofcanada.ca/rates/related/inflation-calculator/. Published 2012. Accessed Dec 2015.
Statistics Canada. CANSIM: socioeconomic database. http://www5.statcan.gc.ca/cansim/a01?lang=eng. Published 2015. Accessed Dec 2015.
Canadian Revenue Agency. Automobile and motor vehicle allowances. https://www.canada.ca/en/revenue-agency/services/tax/businesses/topics/payroll/benefits-allowances/automobile/automobile-motor-vehicle-allowances/automobile-allowance-rates.html Published 2015. Accessed Dec 2015.
Drummond MF, O’Brien BJ, Stoddart GL, Sulpher MJ, Torrance GW. Methods for the Economic Evaluation of Health Care Programmes, 3rd Ed. Chapter # 5: Cost-effectiveness Analysis. New York, NY: Oxford University Press; 2005.
Hummel MJ, Steuten LM, Groothuis-Oudshoorn KG, IJzerman MJ. How the Analytic Hierarchy Process may fill missing gaps in early decision modeling. ISPOR Connections. 2011;17(3):9–10.
Hilgerink MP, Hummel JM, Manohar S, Vaartjes SR, IJzerman MJ. Assessment of the added value of the Twente Photoacoustic Mammoscope in breast cancer diagnosis. Med Devices Evid Res. 2011;4:107–15.
Vallejo-Torres L, Steuten LM, Buxton MJ, Girling AJ, Lilford RJ, Young T. Integrating health economics modeling in the product development cycle of medical devices: a Bayesian approach. Int J Technol Assess. 2008;24(04):459–64.
Carlson JJ, Thariani R, Roth J, Gralow J, Henry NL, Esmail L, Deverka P, Ramsey SD, Baker L, Veenstra DL. Value-of-information analysis within a stakeholder-driven research prioritization process in a US setting: an application in cancer genomics. Med Dec Making. 2013;33(4):463–71.
Craven MP, Morgan SP, Crowe B, Lu B. First experiences from deploying a spreadsheet tool for early economic value assessment of medical device innovations with healthcare decision makers. J Manage Mark Healthc. 2009; 2(3).
DiMasi JA, Caglarcan E, Wood-Armany M. Emerging role of pharma2coeconomics in the research and development decision-making process. PharmacoEconomics. 2001;19(7):753–66.
Grabowski H. The effect of pharmacoeconomics on company research and development decisions. PharmacoEconomics. 1997;11(5):389–97.
Mayhew S. Practical approaches to early stage life sciences technology valuations [Kinapse White Paper]. 2009.
Bartelmes M, Neumann U, Lühmann D, Schönermark M, Hagen A. Methods for assessment of innovative medical technologies during early stages of development. GMS Health Technol Assess. 2009;5:15.
Saito T, Sugiura C, Hirai A, Notani KI, Totsuka Y, Shindoh M, Fukuda H. Development of squamous cell carcinoma from pre-existent oral leukoplakia: with respect to treatment modality. Int J Oral Maxillofac Surg. 2001;30(1):49–53.
Bánóczy J, Csiba Á. Occurrence of epithelial dysplasia in oral leukoplakia: analysis and follow-up study of 12 cases. Oral Surg Oral Med Oral Pathol. 1976;42(6):766–74.
Arduino PG, Surace A, Carbone M, Elia A, Massolini G, Gandolfo S, Broccoletti R. Outcome of oral dysplasia: a retrospective hospital-based study of 207 patients with a long follow-up. J Oral Pathol Med. 2009;38(6):540–4.
Arnaoutakis D, Bishop J, Westra W, Califano JA. Recurrence patterns and management of oral cavity premalignant lesions. Oral Oncol. 2013;49(8):814–7.
Holmstrup P, Vedtofte P, Reibel J, Stoltze K. Long-term treatment outcome of oral premalignant lesions. Oral Oncol. 2006;42(5):461–74.
Review Manager (RevMan5) Software. Cochrane Informatics and Knowledge Management Department. http://community.cochrane.org/tools/review-production-tools/revman-5. Published 2015. Accessed Dec 2015.
Ontario Dental Association. Published 2014. Accessed Dec 2015.
Acknowledgments
This research was supported by the MITACS Accelerate Program, jointly funded by Federal Government and Proteocyte Diagnostic Inc. We would like to thank Dr. David Mock, Dr. Joseph Friedlich and Dr. Alonso Carrasco-Labra for their valuable clinical insights, expert opinion, and guidance. We would also like to thank the Oral and Maxillofacial surgeons for taking time and completing the questionnaires of this study.
Funding
The MITACS Accelerate Program (funding by the Federal Government and Proteocyte Diagnostic Inc) supported this research. The funders head no role in any aspect of this study. They did not have any role in the study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
SKS, GB, and DO designed the study, analyzed and interpreted the data. SKS and GB conducted the statistical and economic analysis. SKS critically interpreted the results and drafted the manuscript. SKS, GB, ML, LT and DO reviewed and provided critical revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1: Figure S1.
The Decision Analytic Model for Oral Pre-cancerous Lesions. Patients who have already undergone biopsy are diagnosed either by histopathology, where the dysplasia is graded as severe, moderate or mild based on the extent of the architectural and cytological changes, or with histopathology and Stratictye™, where patients in each dysplasia grading are further classified as high, medium, or low risk of developing oral cancer based on the result of the Stratictye™ test. These categorizations are mapped in mutually exclusive pathways. Table S1. Qualitative and Quantitative Approaches to Conduct Early CEA. Table S2. Defining the Scope of Early Cost-effectiveness (CEA) Model. Table S3. Four Key Model Assumptions. Table S4. The Literature Search Strategy. Figure S2. The PRISMA flow chart. Table S5. The characteristics of the included studies [30,31,32,33,34]. Figure S3. The forest plot by RevMan [35]. Table S6. Questionnaire for Oral and Maxillofacial Surgeons. Table S7. The outcome of the Questionnaires. Table S8. Costing Details [36]. Table S9. Definitions of the model input parameters. Figure S4. The scattered plot of 5000 Monte Carlo simulations. (DOCX 2425 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Khoudigian-Sinani, S., Blackhouse, G., Levine, M. et al. The premarket assessment of the cost-effectiveness of a predictive technology “Straticyte™” for the early detection of oral cancer: a decision analytic model. Health Econ Rev 7, 35 (2017). https://doi.org/10.1186/s13561-017-0170-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13561-017-0170-6