Abstract
Background
Breast cancer is the cancer with the highest incidence and mortality worldwide. Its treatment is multidisciplinary with surgery, systemic therapy, and radiotherapy. In Colombia, according to Globocan 2018, there is an age-standardized incidence rate of 44 per 100,000 women. Radiotherapy improves local and regional control in patients with breast cancer, and it could even improve relapse-free survival and overall survival in patients with nodal disease. The toxicity of this treatment in most cases is mild and transient, but in a low percentage of patients, radiotherapy-induced tumors may develop.
Case presentation
Seven Colombian patients treated for breast cancer at our institution developed radiotherapy-induced tumors between 2008 and 2018. The median age was 54.4 (range 35–72) years. Six patients had locally advanced tumors at the time breast cancer was diagnosed, and all of them received neoadjuvant or adjuvant chemotherapy and radiotherapy. The radiotherapy-induced tumors were five sarcomas, one of which was a well-differentiated angiosarcomatous vascular lesion with negative c-Myc (benign lesion), and the remaining patient had basal cell carcinoma associated with radiotherapy.
Conclusions
Sarcomas are the most common radiotherapy-induced tumors after breast cancer treatment. These are rare, aggressive tumors and represent between 0.5% and 5.5% of all sarcomas. Basal cell carcinoma has also been associated with breast cancer treatment. The management is individualized and multimodal, including surgical resection and chemotherapy. Different studies have shown that radiation therapy is a risk factor for the development of soft tissue tumors.
Similar content being viewed by others
Introduction
Breast cancer is the cancer with the highest incidence and mortality for women worldwide. A total of 2,088,849 new cases were reported in 2018, corresponding to 11.6% of all cancer cases, and 626,679 died of this disease, corresponding to 6.6% of all cancer deaths [1].
Breast cancer treatment requires a multidisciplinary approach that includes the possibility of surgical resection, radiotherapy, and systemic treatments such as chemotherapy, targeted therapies, and hormone therapies [2]. Among the long-term adverse effects reported in the literature is the appearance of sarcomas, which can be associated with chronic lymphedema (Stewart-Treves syndrome) or radiation exposure; the latter are called “radiotherapy-induced sarcomas” [3].
It has been specified that radiotherapy increases the risk of skin, lung, thyroid, esophageal, and soft tissue tumors (5-year recurrence rate 2.53). Among radiotherapy-induced tumors, sarcomas are the mainly described histology [4]. In the U.S. Surveillance, Epidemiology, and End Results Program (SEER) registry, of 563,155 women diagnosed with breast cancer between 1973 and 2003, 211,027 were treated with radiotherapy; 0.07% of these women developed soft tissue sarcomas in the breast or ipsilateral arm, and the 5-year overall survival rate was 38% [5]. Similarly, literature reports the association of radiotherapy exposure with the development of benign pathologies such as vascular skin lesions, which can eventually present malignant transformation to angiosarcoma [6].
In 1948, Cahan et al. defined four criteria, subsequently modified by Arlen et al., for the diagnosis of sarcomas associated with radiotherapy: (1) sarcoma must appear within previously irradiated fields; (2) there should be no evidence that sarcoma was present before the onset of radiation; (3) it must have a different histology from that of the primary condition confirmed by biopsy; and (4) the onset of sarcoma must occur at least 6 months after ending the radiation therapy [3, 7]. Currently, the latency for the possible appearance of these tumors is not well established, hence the importance of timely follow-up. The most common histological subtypes of radiotherapy-induced sarcomas are undifferentiated pleomorphic sarcoma, angiosarcoma, osteosarcoma, and fibrosarcoma [8].
The National Cancer Institute in Bogota, Colombia (a national reference center), evaluates approximately 685 patients with breast cancer each year, of whom about 80% receive radiotherapy either because they have locally advanced tumors or after conservative surgery. Seven cases of patients who developed second tumors associated with radiotherapy from 2008 to 2018 with a previous breast cancer are presented in this report.
Case presentation
The median age of the Colombian patients was 54.4 (range 35–72) years at the time of breast cancer diagnosis. Six patients presented with locally advanced tumors at the time of their first diagnosis (three with stage IIB, two with stage IIIB, and one with stage IIIA). The remaining patient was classified as stage IIA.
Histopathologically, five patients had luminal A tumors, one had a BRCA1 mutation, one had a luminal tumor that could not be stablished as A or B because Ki67 was not available, and one had triple-negative disease (Table 1). All patients received chemotherapy regimens that consisted of anthracyclines and taxanes, either neoadjuvant or adjuvant. In relation to surgical treatment, conservative surgery of the breast was performed in four cases and modified radical mastectomy in three cases; adjuvant hormone therapy was given to patients positive for hormone receptors, and adjuvant radiotherapy was completed in all patients, performed with a three-dimensional conformational technique, 2-Gy fractioning, and a complete dose from 50 to 60 Gy. The detailed characteristics of patients in relation to their primary breast tumor, treatment received, and diagnosis of the lesion associated with the corresponding radiotherapy are summarized in Table 1.
In our series, the time elapsed between diagnosis of the primary tumor and diagnosis of the tumor associated with radiotherapy varied between 5 years and 10 years, with a mean of 6.7 years. Histopathology following biopsies revealed five cases as sarcomas, one angiosarcoma (very well differentiated, c-Myc negative (benign lesion), and one basal cell carcinoma associated with radiotherapy, which appeared as two lesions with different onset periods, one at 6 years and another at 14 years from the first diagnosis.
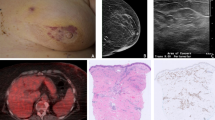
Regarding histology of the sarcomas, two corresponded to pleomorphic sarcomas with osteoid component, two to high-grade angiosarcomas, and the remainder was a high-grade carcinosarcoma. All secondary tumors were located in the previous radiotherapy field (Fig. 1), appearing more frequently in the breast (42.8%), followed by the chest wall (28.6%) or sternum and infraclavicular in 14.3%, respectively (Table 2). Many of these tumors were large, averaging 10 cm in diameter, conditioning an exophytic component tending to skin ulceration (Fig. 2).
Once the tumor diagnoses were confirmed, all patients were presented to multidisciplinary tumor boards, in which the services of breast and soft tissue surgery, clinical oncology, radiation oncology, oncology pathology, oncological radiology, and oncological dermatology participated. The therapeutic decisions to be followed with each patient were defined in these meetings. The five patients diagnosed with sarcomas were taken to wide local resection with margins of 3 cm (Fig. 2). The patient who developed the well-differentiated vascular lesion was handled with clinical follow-up, and the patient with basal cell carcinomas was treated with cryosurgery.
Two patients were offered adjuvant chemotherapy with mesna, anthracycline, and ifosfamide. One of them rejected chemotherapy at first but received anthracycline and platinum when the disease progressed.
Two patients received adjuvant radiotherapy with three-dimensional conformal technique, 1.8-Gy fractions, and a total dose of 30 and 45 Gy. These doses were based on the fields to be irradiated, the organs at risk, and accumulated toxicity of the previous radiotherapy.
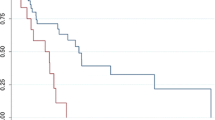
Progressive disease was seen in four of five cases in lung, pleura, chest wall, and regional nodes, and the patients died between 12 and 38 months after diagnosis. Only one of the five patients diagnosed with sarcoma is alive without disease, as are the two patients diagnosed with benign vascular lesion and basal cell carcinoma (Table 3).
Discussion
Breast cancer is the cancer entity most frequently diagnosed in women. The overall survival rate in patients with early breast cancer has increased over the years, largely as a result of adjuvant systemic treatment (chemotherapy, hormone therapy, and targeted therapies) [1]. In breast cancer, radiation therapy is indicated in patients with locally advanced disease and in patients who undergo conservative breast surgery. This treatment modality has been able to demonstrate benefits in relapse-free survival and overall survival [2]. However, its use has been described as an established risk factor for the development of other malignant tumors. Some sites show a significantly higher relative risk of developing tumors associated with radiotherapy, such as the thyroid, esophagus, lung, and soft tissues. This risk depends on the technologies used, the area treated, the equivalent biological dose, the dose per fraction, fractionation, the duration of treatment, bone marrow exposure, and personal sensitivity [9].
Within the genomics of tumors, implication of the rearrangement of the RET proto-oncogene in thyroid cancer and amplification of MYC in cutaneous angiosarcoma after irradiation of the chest wall for breast cancer are known [9]. Atypical vascular lesions associated with radiation are in a state of continuous transformation, which can progress to more aggressive malignant angiosarcoma [10].
Sarcoma associated with radiotherapy is a rare and aggressive neoplasm that represents between 0.5% and 5.5% of all sarcomas. The prevalence of basal cell carcinoma induced by ionizing radiation is estimated at 4% [11]. Several studies have shown that radiotherapy is a significant risk factor for the development of soft tissue tumors and, in particular, angiosarcomas, after breast cancer treatment [12, 13]. Blanchard et al. reported the appearance of sarcomas associated with radiotherapy in 34 patients who received treatment for breast cancer between 1975 and 2001, and 65% of these patients died [14]. Taghian et al. reported an accumulated risk of developing soft tissue or bone sarcomas of 0.2% at 10 years within their breast cancer post-treatment cohort of women [15] (see Table 4).
In a study carried out in the radiation therapy oncology department at the Curie Institute in Paris, France, in 2004, where the records of 16,705 patients with breast carcinoma were reviewed, 27 sarcomas associated with radiotherapy were found. The time interval between irradiation and the presence of a second tumor in the irradiated area ranged from 3 to 20.3 years, and the mortality was 55.5% [16]. At the Helsinki Comprehensive Cancer Center, the Finnish Cancer Registry reported a total of 96 patients diagnosed with sarcoma after treatment for breast cancer between 1953 and 2014, with an average latency period of 11.0 (range 0.6–29.9) years [17].
In our institution, 6850 patients treated for breast cancer were found from 2008 to 2018. The time elapsed between diagnosis of the primary tumor and diagnosis of the sarcoma associated with radiotherapy varied between 5 years and 10 years. In the study carried out in Tunisia in 2013, the mean latency for basal cell carcinomas between irradiation and carcinoma was 35.7 years [11]; a longer latency period was found in our case. Atypical radiologically induced vascular lesions occur approximately 3 years after initial treatment [10]. The initial approach begins with physical examination and imaging, but the gold standard is confirmation of the lesion through a biopsy that will corroborate a histological type of tumor different from the primary cancer, as described by Cahan and Arlen [18].
Among different treatments for breast cancer is hypofractionated radiotherapy, which gives a total radiation dose of 40 to 42.56 Gy, but this is not the standard for advanced disease and was not given to any of the seven patients in this series. When comparing hypofractionated radiotherapy with the standard fractioning, they are biologically equivalent, and there is no evidence that different radiotherapy fractioning could increase the risk of second tumors.
The optimal treatment is a wide surgical resection with negative margins, which may result in 5-year survival rates of 40% [19]. However, recurrence and metastases are common, so chemotherapy has become a main component of treatment for sarcomas associated with radiotherapy [20]. Sometimes the benefit of radiotherapy must be established within this therapeutic approach (depending on the histological grade and size of the lesion). The five cases with diagnosis of radiotherapy-induced sarcomas underwent extensive local resection; the patient with well-differentiated vascular lesion was followed in the outpatient clinic; and the patient who had basal cell carcinomas was treated with cryosurgery, as recommended by current literature [21].
Patients with radiation-associated sarcomas have a worse prognosis than patients with primary soft tissue sarcomas; hence, their treatment must be aggressive, including chest wall resections if necessary. Due to the low prevalence of tumors associated with breast cancer radiotherapy, it is difficult to establish a specific monitoring schedule. However, this review aims to provide context for health professionals with regard to the risk of its long-term development and its aggressive behavior and to emphasize the need for timely treatment by a professional who is expert in soft tissue tumors and preferably at a cancer reference center.
Another important aspect to highlight is that, although this entity has a poor prognosis, its low incidence should not affect the decision to administer radiotherapy to patients with breast cancer who have the indication to receive it, because the benefit of radiation therapy is higher than the risk of radiotherapy-induced tumors.
New scientific studies are expected to better define the factors associated with adjuvant radiotherapy that increase the risk of developing other tumors, and to determine whether changes in these factors (for example, smaller radiation fields) would have an impact on the future incidence of the disease.
Conclusions
Tumors associated with radiotherapy are a low-incidence entity but with high aggressiveness from the local and systemic points of view, which results in high mortality rates. It is noteworthy that radiotherapy is an indispensable therapeutic tool in the treatment of breast cancer, and the presented risk does not outweigh its benefit.
These tumors must be differentiated from local breast cancer relapses, so a biopsy for histological confirmation and a multidisciplinary approach at a reference cancer center are always required. It is expected that new scientific studies will help determine the risk factors for developing this disease and the impact that new technologies will have on the appearance of tumors associated with radiotherapy.
Availability of data and materials
Data are available in the digital medical records at the National Cancer Institute, Bogota, Colombia. These records are not public, owing to the confidentiality of the type of documents, but they are available from the corresponding author on reasonable request.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global Cancer 348 Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 349 Cancers in 185 Countries. CA Cancer J Clin. 2018;68(6):394–424.
National Comprehensive Cancer Network (NCCN). NCCN guidelines for breast cancer. Version 3.2019. www.nccn.org/professionals/physician_gls/pdf/cervical.pdf. Accessed September 15, 2019.
Murray EM, Werner D, Greeff EA, Taylor DA. Postradiation sarcomas: 20 cases and a literature review. Int J Radiat Oncol Biol Phys. 1999;45(4):951–61.
Berrington de Gonzalez A, Curtis RE, Gilbert E, Berg CD, Smith SA, Stovall M, et al. Second solid cancers after radiotherapy for breast cancer in SEER cancer registries. Br J Cancer. 2010;102(1):220–6.
Mery CM, George S, Bertagnolli MM, Raut CP. Secondary sarcomas after radiotherapy for breast cancer: sustained risk and poor survival. Cancer. 2009;115(18):4055–63.
Uchin JM, Billings SD. Radiotherapy-associated atypical vascular lesions of the breast. J Cutan Pathol. 2009;36(1):87–8.
Sheth GR, Cranmer LD, Smith BD, Grasso-LeBeau L, Lang JE. Radiation-induced sarcoma of the breast: a systematic review. Oncologist. 2012;17(3):405–18.
Sheppard DG, Libshitz HI. Post-radiation sarcomas: a review of the clinical and imaging features in 63 cases. Clin Radiol. 2001;56(1):22–9.
Sholl LM, Barletta JA, Hornick JL. Radiation-associated neoplasia: clinical, pathological and genomic correlates. Histopathology. 2017;70(1):70–80.
Anzalone CL, Cohen PR, Tschen JA, MacFarlane DF. Radiation-associated atypical vascular lesions: vascular lesions with endothelial cell atypia presenting in the radiation port of breast cancer patients. Skinmed. 2014;12(6):344–8.
Zaraa I, Ben Taazayet S, Zribi H, Chelly I, El Euch D, Trojjet S, et al. Cutaneous carcinoma induced by radiotherapy: a report of 31 cases. Tunis Med. 2013;91(3):191–5.
Russell WO, Cohen J, Enzinger F, Hajdu SI, Heise H, Martin RG, et al. A clinical and pathological staging system for soft tissue sarcomas. Cancer. 1977;40(4):1562–70.
Laskin WB, Silverman TA, Enzinger FM. Postradiation soft tissue sarcomas: an analysis of 53 cases. Cancer. 1988;62(11):2330–40.
Blanchard DK, Reynolds C, Grant CS, Farley DR, Donohue JH. Radiation-induced breast sarcoma. Am J Surg. 2002;184(4):356–8.
Taghian A, De Vathaire F, Terrier P, Le M, Auquier A, Mouriesse H, et al. Long-term risk of sarcoma following radiation treatment for breast cancer. Int J Radiat Oncol Biol Phys. 1991;21(2):361–7.
Kirova YM, Vilcoq JR, Asselain B, Sastre-Garau X, Fourquet A. Radiation-induced sarcomas after radiotherapy for breast carcinoma: a large-scale single-institution review. Cancer. 2005;104(4):856–63.
Salminen SH, Sampo MM, Böhling TO, Tuomikoski L, Tarkkanen M, Blomqvist CP. Radiation-associated sarcoma after breast cancer in a nationwide population: Increasing risk of angiosarcoma. Cancer Med. 2018;7(9):4825–35.
Arlen M, Higinbotham NL, Huvos AG, Marcove RC, Miller T, Shah IC. Radiation-induced sarcoma of bone. Cancer. 1971;28(5):1087–99.
Cha C, Antonescu CR, Quan ML, Maru S, Brennan MF, Aust JB, et al. Long-term results with resection of radiation-induced soft tissue sarcomas. Ann Surg. 2004;239(6):903–9.
Dickson MA. Systemic treatment options for radiation-associated sarcomas. Curr Treat Options in Oncol. 2014;15(3):476–81.
Tchanque-Fossuo CN, Eisen DB. A systematic review on the use of cryotherapy versus other treatments for basal cell carcinoma. Dermatol Online J. 2018;24(11):13030/qt49k1c38t.
Acknowledgements
Not applicable.
Funding
No funding was received from any source for this study.
Author information
Authors and Affiliations
Contributions
DH and SM performed the search and collection of cases. MG and NB performed the data analysis. AA and JE performed the literature search. All authors participated in the elaboration of the manuscript. SD and MG made the final corrections of the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No identifying information of the patients has been included. No animals were involved or harmed in the study. The Ethics Committee at the National Cancer Institute, Bogota, Colombia, does not require evaluation of case series of fewer than ten patients.
Consent for publication
Written informed consent was obtained from the patients for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Garcia, M., Hernandez, D., Mendoza, S. et al. Tumors associated with radiotherapy: a case series. J Med Case Reports 14, 179 (2020). https://doi.org/10.1186/s13256-020-02482-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-020-02482-x