Abstract
Background
Although several cases of hepatitis B virus reactivation have been described in patients with a history of hepatitis B virus infection while undergoing treatment for hepatitis C virus infection with direct acting antivirals, the question of whether hepatitis B virus surface antigen immune-escape mutations might play a role has not been addressed so far.
Case presentation
We report a case of hepatitis B virus reactivation in a Caucasian patient infected with hepatitis C virus during treatment with sofosbuvir and velpatasvir. A 50-year-old man with a genotype 1a hepatitis C virus infection was considered for therapy. His serological profile was hepatitis B virus surface antigen-negative, hepatitis B virus core antibody-positive, hepatitis B virus surface antibody-negative, and anti-hepatitis D virus-positive. The detection of hepatitis B virus deoxyribonucleic acid (DNA) indicated active viral replication during the direct acting antiviral treatment that spontaneously returned to undetectable levels after treatment completion. Starting from week 12 after the end of treatment, hepatitis B virus surface antibody titers and hepatitis B virus e antibody developed. Sequencing analysis revealed the hepatitis B virus genotype D3 and the presence of two relevant immune-escape mutations (P120S and T126I) in the major hydrophilic region by analyzing the S region.
Conclusions
We speculate that the presence of the hepatitis B virus surface antigen mutations, endowed with the enhanced capability to elude the immune response, could play a role in hepatitis B virus reactivation. This observation confirms that occult hepatitis B infection should also be carefully monitored, through surveillance of the hepatitis B virus viral load before and during direct acting antiviral treatment of hepatitis C virus.
Similar content being viewed by others
Background
Chronic infection with either hepatitis B virus (HBV) or hepatitis C virus (HCV) is responsible for a high morbidity and mortality burden worldwide. Since these viruses share common transmission routes, HBV and HCV coinfection is not rare, and it is estimated that 1–15% of patients with HCV infection might be coinfected with HBV [1]. In developed countries, people who use drugs (PWUD) are particularly exposed to HBV-HCV coinfection, and epidemiological studies suggest that approximately half of the PWUD who are HCV-positive may have an occult HBV infection (OBI) [2]. OBI, defined by the detection of HBV deoxyribonucleic acid (DNA) in hepatocytes or in the serum of patients who are hepatitis B virus surface antigen (HBsAg)-negative, can contribute to accelerated evolution of cirrhosis or the development of hepatocellular carcinoma (HCC) in patients coinfected with HCV [3, 4]. The interaction between HBV and HCV can give rise to a wide spectrum of virological patterns [5]; in the majority of cases, HCV predominates over HBV replication and transcription via immunological and virological mechanisms [5, 6]. Recently, several cases of HBV reactivation (HBVr) [7, 8] have been described in patients with a history of HBV infection while undergoing treatment for HCV infection with direct acting antivirals (DAAs), suggesting that the clearance of HCV abrogates the inhibitory effect exerted by HCV on HBV replication. Despite increasing awareness of the risk of DAA-induced HBVr, the question of whether HBsAg immune-escape mutations might play a role in this process has not been addressed so far. Previous studies have shown that immune-escape mutations can play a role in HBV reactivation driven by immunosuppression [9]. Here, we report a case of HBVr in a patient infected with HCV, with resolved HBV infection, treated with sofosbuvir and velpatasvir for 12 weeks. Surprisingly, the patient had reactivated HBV infection and the virus developed two mutations localized in an immune-active HBsAg region, thus making ineffective HBV-specific immune response and favoring HBV viral load (VL) flare. The clinical relevance of the case is also due to the difficulty in the diagnosis of HBVr since the mutations in HBsAg did not allow its detection by the usual laboratory tests.
Case description
A Caucasian 50-year-old man, in a stable relationship and employed, was considered for HCV treatment at our center. In 1996, during a hospitalization for jaundice, he received a diagnosis of acute hepatitis B/hepatitis D virus (HDV) infection. At that time, an HCV infection genotype 1a was also diagnosed, which had never been treated. The patient had a hystory of previous use of injected heroin and inhaled cocain, and he was in opiate substitution therapy (OST) with buprenorphine. Except for this, he did not use other drugs. He smoked tobacco, reported a previous alcohol abuse, and at the first assessment he stated that he drank 1–2 drinks a day. His medical history was notable for a sinus tachycardia and he underwent inguinal hernioplasty and appendectomy. No liver disease was documented in his family history.
His serological profile at admission to our center was HBsAg-negative, HBV core antibody (anti-HBc)-positive, HBV surface antibody (anti-HBs)-negative, and hepatitis D virus antibody (anti-HDV)-positive.
On presentation, he did not report any symptoms and denied previous episodes of ascites, hematemesis, melena, hepatic encephalopathy, and vomiting. A physical examination excluded signs of hepatic decompensation; in particular, it did not reveal ascites, splenomegaly, leg swelling, jaundice, and spider angiomas. The remainder of the examination was normal.
In the HCV pre-treatment assessment, he had F0–F1 fibrosis stage (Metavir score) evaluated by transient elastography (median liver stiffness 6.9 kPa) and an abdominal ultrasound excluded the presence of HCC and signs of portal hypertension. Laboratory analysis showed that alanine aminotransferase (ALT) was 51 IU/L, aspartate aminotransferase (AST) was 52 IU/L, and glucose 108 mg/dL. The count of white cells and platelets, and levels of hemoglobin, creatinine, alpha-fetoprotein, and electrolytes were normal; liver function tests were normal. HCV VL was 7,014,213 IU/ml and no HCV resistance-associated substitutions were found. His FIB-4 score was 2.13. Other laboratory test results are shown in Table 1; data regarding the HBV VL were not available.
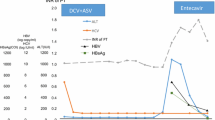
In October 2017, he started once daily sofosbuvir/velpatasvir (400/100 mg) without ribavirin (RBV) for 12 weeks. HCV ribonucleic acid (RNA) was 37 IU/ml at week 4, below the limit of quantification (< 12 IU/ml) at week 8 and undetectable at the end of treatment (EOT) (Fig. 1). The detection of HBV DNA showed active viral replication and values of 16, 20, and 14 IU/ml were found at weeks 4, 8, and 12, respectively, of DAA treatment. Of note, the HBsAg and hepatitis B virus e antigen (HBeAg) remained negative despite evidence of ongoing HBV replication. The sequencing analysis of the HBV reverse transcriptase (RT)/S regions revealed the presence of the HBV genotype D3 and the absence of amino acid substitutions conferring resistance to any anti-HBV drugs. In contrast, by analyzing the S region, two relevant mutations, P120S and T126I, localized in the major hydrophilic region, an immune-active HBsAg domain, were found. He reached a sustained virological response (SVR) for HCV at 12 and 24 weeks after the EOT. An abdomen ultrasound performed at week 24 after the EOT showed hepatic steatosis but excluded the presence of nodular lesions. At the same time-point, non-invasive measurement of liver fibrosis, through transient elastography, confirmed the starting fibrosis stage (median liver stiffness 5.0 kPa, F0/F1 Metavir stage). At weeks 4 and 12 after the EOT, the HBV VL, in the absence of antiviral therapy, was < 10 IU/ml and 12 IU/ml, respectively, but returned below the limit of quantification at weeks 16, 20, and 24 after the EOT. A search for HDV RNA, performed at week 8 after the EOT, was negative. HBsAg and HBeAg remained negative despite the HBVr at all tested time-points; however, starting from week 12 after the EOT, the anti-HBs and hepatitis B virus e antibody (anti-HBe) titers spontaneously developed.
Virological and biochemical parameters trend during and after direct acting antiviral treatment. Hepatitis B virus surface antibody, hepatitis B virus surface antigen, hepatitis B virus e antibody, hepatitis B virus e antigen, and hepatitis B virus core antibody results are presented corresponding to the time-point of collection. ALT alanine aminotransferase, anti-HBc hepatitis B virus core antibody, anti-HBe hepatitis B virus e antibody, anti-HBs hepatitis B virus surface antibody, HBeAg hepatitis B virus e antigen, HBsAg hepatitis B virus surface antigen, HBV hepatitis B virus, HCV hepatitis C virus
Discussion and conclusions
To the best of our knowledge, we are the first to report a case of HBVr characterized by the emergence of viral strains with immune-escape mutations in a patient coinfected with HCV with isolated anti-HBc positivity and on a successful treatment with the latest generation of DAAs sofosbuvir and velpatasvir. HBVr is characterized by a sudden increase in HBV replication (> 2 log10 in viremic patients or detectable HBV DNA in patients with resolved HBV infection) or a reversion to an HBsAg-positive status in individuals who are HBsAg-negative and has been extensively reported in patients treated with immunosuppressive agents and/or intensive chemotherapy [10]. HBVr during chronic HCV infection (CHC) was also previously described in patients treated with interferon-based therapies [11], but recent reports demonstrated that HBVr is more frequent and occurs earlier in patients with CHC treated with DAAs. Moreover, a meta-analysis [7] showed that the overall risk of HBVr was 24% in patients who were HBsAg-positive and 1.4% in those with resolved HBV infection. Although HBVr is not uncommon, the occurrence of accompanying hepatitis in patients with resolved HBV infection is a rare event [12,13,14] and only occasionally leads to clinically significant outcomes. According to these previous reports, we observed an early HBV viremia in the absence of a concomitant increase in the hepatic necro-inflammatory markers, which in the following months returned spontaneously below the limit of quantification. Some elements lead us to hypothesize reactivation. First, the viral decay kinetics, and second, the antibody response (anti-HBs and anti-HBe), which developed starting from week 12 after the EOT, were probably induced by the presence of a singular episode of HBV flare. In addition, our patient was also coinfected with HDV, which is known to exert a suppressive role on the replication of HBV [15] and may have prevented a further rise in the HBV viremia. According to the American Association for the Study of Liver Diseases-Infectious Diseases Society of America (AASLD-IDSA) recommendations [16], patients who are HBsAg-positive meeting criteria for treatment of active HBV infection should be started on therapy at the same time or before HCV DAA therapy is initiated, whereas patients with low or undetectable HBV DNA titers can either receive prophylactic treatment or be monitored at regular intervals. Conversely, the same guidelines do not provide clear recommendations for the monitoring of HBV DNA among patients with resolved HBV infection. Despite the lack of indications from the current guidelines, we decided to search for HBV DNA at week 4, in the absence of an increase of transaminases, because of the European Medicines Agency (EMA) warning on the risk of early reactivation in patients with overt HBV infection or OBI (warning letter EMA/795452/2016, 2 December 2016). Furthermore, as reported above, the increase of transaminases related to HBV reappearance is not so frequent; hence, only monitoring the level of transaminases would not be sufficient.
An element of great interest is that, to the best of our knowledge, this is the first report of HBVr characterized by the emergence of viral strains carrying immune-escape mutations in a patient coinfected with HCV with isolated anti-HBc positivity and on successful treatment with the latest generation of DAAs. Immune-escape mutations in HBsAg are clinically relevant since their presence, by enabling the evasion of the adaptive immune response, can promote both viral replication [17] and chronic persistence of HBV infection [18, 19] and may reduce HBsAg diagnostic detection. Interestingly, the presence of the immune-escape mutants was related to HBVr in patients who had undergone immunosuppressive treatments [9]. In recent years, only two case reports have focused on HBVr of the HBsAg mutant strains in patients treated with DAAs for HCV [13, 18]. In the first case [13], genome sequencing revealed a T118K mutation in the S region, but in contrast to our description, the HBV viremia occurred 5 months after the EOT with daclatasvir and asunaprevir. Notably, the serological profile of this patient at baseline was not reported. More recently, Fusco et al. [20] described a reactivation of vaccine-escape HBV mutants during anti-HCV treatment with ledipasvir/sofosbuvir (90/400 mg) for 12 weeks. Similar to our case, the patient had a baseline profile of OBI infection (HBsAg-negative, anti-HBc-positive, HBV DNA 120 UI/L), but, in contrast to our patient, the anti-HBs levels were above the protective threshold before starting the treatment. A limitation of our case description is the lack of measurement of the HBV DNA levels before the start of the DAA treatment, in line with the latest European Association for the Study of the Liver (EASL) recommended guidelines; hence, we cannot exclude pre-existing low-level HBV viremia in the context of OBI.
To conclude, we speculate that the presence of the antigen S mutations, endowed with enhanced capability to elude immune response, could play a role in HBVr. This observation confirms that OBI should also be carefully monitored, through the surveillance of HBV VL, before and during DAA treatment of hepatitis C. This approach could enable early identification of HBVr and find a pre-existing detectable HBV viremia in the context of OBI, which may be at higher risk of reactivation. Further studies are warranted to confirm the hypothesis regarding the role of HBsAg immune-escape mutants in predisposing HBVr during DAA regimens for CHC.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AASLD-IDSA:
-
American Association for the Study of Liver Diseases-Infectious Diseases Society of America
- ALT:
-
Alanine aminotransferase
- anti-HBc:
-
Hepatitis B virus core antibody
- anti-HBe:
-
Hepatitis B virus e antibody
- anti-HBs:
-
Hepatitis B virus surface antibody
- anti-HDV:
-
Hepatitis D virus antibody
- AST:
-
Aspartate aminotransferase
- CHC:
-
Chronic hepatitis C virus infection
- DAAs:
-
Direct acting antivirals
- EASL:
-
European Association for the Study of the Liver
- EMA:
-
European Medicines Agency
- EOT:
-
End of treatment
- HBeAg:
-
Hepatitis B virus e antigen
- HBsAg:
-
Hepatitis B virus surface antigen
- HBV:
-
Hepatitis B virus
- HBVr:
-
Hepatitis B virus reactivation
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- HDV:
-
Hepatitis D virus
- OBI:
-
Occult hepatitis B infection
- OST:
-
Opiate substitution therapy
- PWUD:
-
People who use drugs
- RBV:
-
Ribavirin
- RT:
-
Reverse transcriptase
- SVR:
-
Sustained virological response
- VL:
-
Viral load
References
Konstantinou D, Deutsch M. The spectrum of HBV/HCV coinfection: epidemiology, clinical characteristics, viral interactions and management. Ann Gastroenterol. 2015;28:221–8.
Teti E, Foroghi L, Malagnino V, et al. Real world adherence to Direct-Acting Antivirals in a cohort of drug users in Rome, Italy. J Hepatol. 2018;68:S285–6. (Poster presentation at the International Liver Congress 2018
Squadrito G, Spinella R, Raimondo G. The clinical significance of occult HBV infection. Ann Gastroenterol. 2014;27:15–9.
Pollicino T, Raimondo G. Occult hepatitis B infection. J Hepatol. 2014;61:688–9. 2014
Caccamo G, Saffioti F, Raimondo G. Hepatitis B virus and hepatitis C virus dual infection. World J Gastroenterol. 2014;20:14559–67.
Coppola N, Onorato L, Pisaturo M, et al. Role of occult hepatitis B virus infection in chronic hepatitis C. World J Gastroenterol. 2015;21:11931–40.
Mücke MM, Backus LI, Mücke MM, et al. Hepatitis B virus reactivation during direct-acting antiviral therapy for hepatitis C: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2018;3:172–80.
Calvaruso V, Ferraro D, Licata A, et al. HBV reactivation in patients with HCV/HBV cirrhosis on treatment with direct-acting antivirals. J Viral Hepat. 2018;25:72–9.
Salpini R, Colagrossi L, Bellocchi MC, et al. Hepatitis B surface antigen genetic elements critical for immune escape correlate with hepatitis B virus reactivation upon immunosuppression. Hepatology. 2015;61:823–33.
Perrillo RP, Gish R, Falck-Ytter YT. American Gastroenterological Association Institute Technical Review on Prevention and Treatment of Hepatitis B Reactivation During Immunosuppressive Drug Therapy. Gastroenterology. 2014; https://doi.org/10.1053/j.gastro.2014.10.038.
Chen G, Wang C, Chen J, et al. Hepatitis B reactivation in hepatitis B and C coinfected patients treated with antiviral agents: A systematic review and meta-analysis. Hepatology. 2017;66:13–26.
De Monte A, Courjon J, Anty R, et al. Direct-acting antiviral treatment in adults infected with hepatitis C virus: Reactivation of hepatitis B virus coinfection as a further challenge. J Clin Virol. 2016;78:27–30.
Hayashi K, Ishigami M, Ishizu Y, et al. A case of acute hepatitis B in a chronic hepatitis C patient after daclatasvir and asunaprevir combination therapy: hepatitis B virus reactivation or acute self-limited hepatitis? Clin J Gastroenterol. 2016;9:252–6.
Belperio PS, Shaoumian TA, Mole LA, et al. Evaluation of Hepatitis B Reactivation Among 62,920 Veterans Treated With Oral Hepatitis C Antivirals. Hepatology. 2017;66(1):27–36. https://doi.org/10.1002/hep.29135.
Alfaiate D, Lucifora J, Abeywickrama-Samarakoon N, et al. HDV RNA replication is associated with HBV repression and interferon-stimulated genes induction in super-infected hepatocytes. Antivir Res. 2016;136:19–31.
Hepatitis C. Guidance 2018 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. 2018;67:1477–92. https://doi.org/10.1093/cid/ciy585. www.hcvguidelines.org.
Colagrossi L, Hermans LE, Salpini R, et al. Immune-escape mutations and stop-codons in HBsAg develop in a large proportion of patients with chronic HBV infection exposed to anti-HBV drugs in Europe. BMC Infect Dis. 2018;18:2511–2.
Velay A, Jeulin H, Eschlimann M, et al. Characterization of hepatitis B virus surface antigen variability and impact on HBs antigen clearance under nucleos(t)ide analogue therapy. J Viral Hepat. 2016; https://doi.org/10.1111/jvh.12498.
Charuworn P, Hengen PL, Schall RA, et al. Baseline Interpatient Hepatitis B Viral Diversity Differentiates HBsAg Outcomes in Patients Treated With Tenofovir Disoproxil Fumarate. J Hepatol. 2014; https://doi.org/10.1016/j.jhep.2014.12.008.
Fusco RH, Ganova-Raeva L, Khudyakov Y, et al. Reactivation of a Vaccine escape Hepatitis B Virus Mutant in a Cambodian patient During anti-Hepatitis C Virus therapy. Front Med. 2018; https://doi.org/10.3389/fmed.2018.00097.
Acknowledgements
The authors thank the patient and all the members of Infectious Diseases unit and Virology unit of University of Rome Tor Vergata for the helpful collaboration.
Funding
No source of funding had a role in the study’s design, conduct, or reporting.
Author information
Authors and Affiliations
Contributions
LFB, VM, and LS contributed to conception of the study. LFB and LF drafted the manuscript. ET, CC, AG, MAr, RS, and VS have been involved in acquiring, analyzing, and interpreting clinical and virological data. VM, ET, CC, RS, VS, MAn, and LS reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
It was not required to submit the case to the institutional ethics committee.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images. Copies of the written consent are available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Foroghi Biland, L., Ferrari, L., Malagnino, V. et al. Hepatitis B virus reactivation sustained by a hepatitis B virus surface antigen immune-escape mutant isolate in a patient who was hepatitis B core antibody positive during treatment with sofosbuvir and velpatasvir for hepatitis C virus infection: a case report. J Med Case Reports 13, 299 (2019). https://doi.org/10.1186/s13256-019-2232-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-019-2232-3