Abstract
Background
Endothelial growth factor receptor (EGFR) mutations are an essential driver of personalized therapy for patients with lung cancer and are detected in approximately 15% of Caucasian and 50% of Asian patients. EGFR tyrosine kinase inhibitors have been developed and used for this set of patients. T790M mutation in exon 20 is usually associated with secondary resistance to EGFR tyrosine kinase inhibitors therapy but is also present in treatment-naïve patients. The frequency for baseline T790M mutation varies from 4 to 35% according to the detection method used. Newer techniques have yielded higher rates, but concerns about false-positive results have been raised. Compound mutations account for 4–14% of all EGFR-mutated tumors, with no studies yet to provide a frequency rate for T790M + 19 deletion association due to the small number of cases. However, there are reports that pretreatment T790M + L858R association is significantly more frequent compared to T790M + exon 19 deletion mutations. Diagnostic challenges, current knowledge on the subject, and therapeutic decisions are discussed.
Case presentation
We present the case of a 43-year-old Hispanic woman, a treatment-naïve patient, with metastasized lung cancer adenocarcinoma harboring a T790M deletion along with the classic 19 mutation. The initial symptoms were monoparesis of her left leg, associated with hyperreflexia, and hypoesthesia. In the absence of third-generation tyrosine kinase inhibitors, a platinum-based therapy was initiated with no response and she died 4 months after diagnosis.
Conclusions
Osimertinib seems to be a suitable therapy for treatment-naïve patients with sensitizing and resistant compound EGFR mutations. More studies regarding the clinical characteristics of these patients and the appropriate management of this condition are needed to provide the highest standard of care.
Similar content being viewed by others
Background
Non-small cell lung cancer (NSCLC) accounts for the majority of lung neoplasms and its mortality in advanced stages is very high, compared with other cancer types [1, 2]. Driver mutations can be found in a high percentage of these cases, including endothelial growth factor receptor (EGFR) alterations [3,4,5]. However, compound mutations in treatment-naïve patients are rare, even more so if the association is that of a T790M mutation and an exon 19 deletion (19-Del) [5, 6]. There are very few cases of this compound mutation found in the literature.
We present the case of a 43-year-old, treatment-naïve, woman with metastasized lung cancer adenocarcinoma harboring a T790M deletion along with the classic 19-Del. The importance of this case lies in the rareness of this compound mutation, the ample variation of T790M incidence in the literature, and the multiple treatment difficulties that arise when, for a particular reason, including no availability, a third-generation EGFR tyrosine kinase inhibitor (TKI) cannot be used.
Case presentation
A 43-year-old Hispanic woman with no past medical or family history of importance, presented to our emergency room (ER) with progressive lumbar pain for the past 4 months, 10/10 in intensity, which irradiated to her left lower limb limiting her functionality. She also referred weakness of her left leg, associated with loss of sensitivity, and had experienced night fevers, chills, and a 23 kg (50 pound) weight loss. A physical examination revealed monoparesis of her left leg, associated with hyperreflexia, and hypoesthesia.
A contrasted pelvis and lumbar magnetic resonance imaging (MRI) showed a solid infiltrative mass in her left sacral and iliac bones, compromising the left sacroiliac joint, the ipsilateral sacral nerve roots, and the pyramidalis and gluteus medius muscles. Other bone lesions compromised the left femoral neck and the right femoral diaphysis (Fig. 1).
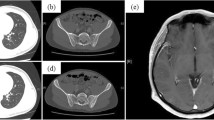
The hypothesis was that these lesions were metastatic, so further studies were ordered. Breast ultrasonography revealed a mass of 2 cm by 3 cm in her left breast, but a subsequent fine-needle biopsy showed benign histopathology. A computed tomography (CT) scan revealed masses in both her liver and lung (Fig. 2). A bronchoalveolar wash was negative for malignancy, and so was a transbronchial biopsy. A decision was made to do a CT-guided percutaneous biopsy of the sacral lesion; the results revealed a metastasized lung adenocarcinoma (Fig. 3), negative for ALK mutation but with a complex mutation of the EGFR gene: a 19-Del associated with a T790M (exon 20) mutation. The genetic assay used was cobas® EGFR Mutation Test v2 (Roche®). The target deoxyribonucleic acid (DNA) was amplified and detected on the cobas® 480 system which measures the fluorescence generated by specific polymerase chain reaction (PCR) products, using the amplification and detection reagents provided in the cobas® EGFR mutation test kit (lightmix®).
Metastasized lung adenocarcinoma in sacral bone. Sacral bone biopsy. a Hematoxylin and eosin stain, solid pattern metastatic adenocarcinoma of the lung (× 10). b, c Positive thyroid transcription factor 1 and napsin A immunohistochemistry stain (× 10). d Negative immunohistochemistry stain for EML-4, ALK, and programmed death-ligand 1 rearrangements
Stage IV lung adenocarcinoma was diagnosed. In the absence of third-generation EGFR-TKIs (not approved by the local drug and food administration at the time) and taking into account the performance status of our patient, which was Eastern Cooperative Oncology Group (ECOG) 2, platinum-based chemotherapy of gemcitabine (1000 mg/m2 day 1 and 8) with carboplatin (AUC 6) was initiated. Only grade 1 toxicities were observed.
Our patient suffered from a severe headache 25 days after admission, with no response to analgesia, and a CT scan of her brain was done; the CT scan revealed intraparenchymal bleeding on the left cerebellar hemisphere, with fourth ventricle compression and non-communicant acute hydrocephalus. A brain MRI showed a lesion in the cerebellum, thought to be a metastasis (Fig. 4). After stabilization of the clinical status, whole brain irradiation with three-dimensional conformational radiotherapy (CRT) was done (3 Gy fractions for a total dose of 30 Gy). Radiation therapy (three-dimensional CRT) was also administered to her left sacral and iliac bones for pain management (4 Gy fractions for a total dose of 20 Gy). She died 4 months after diagnosis.
Brain magnetic resonance imaging. A nodular lesion with a cystic component of intra-axial location in the left cerebellar hemisphere is observed, whose enhancement component measures 23 × 31 mm (anteroposterior × transverse), is associated with vasogenic edema in the periphery and conditions the mass effect
Discussion
NSCLC accounts for nearly 85% of all lung neoplasms, and its 5-year survival rate is still low, around 17% dropping to 5%, if the disease is categorized as stage IV [1, 2]. As many as 80% of cases of lung adenocarcinoma have a driver mutation contributing to early carcinogenesis [7]; the identification of these mutations has allowed for a more personalized therapy, improving outcomes in relevant populations. EGFR mutations, detected in approximately 15% of Caucasian and 50% of Asian patients [3, 4], have been targeted since 2004, resulting in EGFR-TKIs such as erlotinib and gefitinib.
EGFR mutations are more frequent in tumors with adenocarcinoma histology, in never-smokers or light smokers of tobacco, in women with NSCLC, and in patients with East Asian ethnicities [8]. The two most common EGFR mutations, also called classic mutations, are the 19-Del and the L858R substitution in exon 21 [9], both of them regarded as positive predictive biomarkers for response to EGFR-TKIs [10]. These mutations are oncogenic because they favor the active state of the kinase, inducing EGFR-mediated antiapoptotic and prosurvival proteins specifically in the Akt/STAT and MAPK signaling pathways [11].
T790M mutation in exon 20 is usually associated with secondary resistance to EGFR-TKIs therapy, being responsible for approximately 50 to 60% of these cases [12, 13]. This point mutation increases the affinity of EGFR for adenosine triphosphate (ATP) and decreases drug binding through steric hindrance, consequently diminishing the binding efficacy of EGFR-TKIs [12, 14,15,16]. If this mutation is present before treatment, then it becomes a rare EGFR mutation. The frequency of this mutation in treatment-naïve patients varies significantly according to the population screened and the method used for detection. The rate fluctuates between 1 and 3% when direct sequencing is used [16]. However, when newer techniques like real-time (RT) PCR, next-generation sequencing (NGS), and highly sensitive matrix-assisted laser desorption/ionization time-of-flight mass spectrometry (MALDI-TOF MS) are used, the frequency rises to 25 to 35% [17, 18]. One study reported a rate of 79% using colony hybridization [19]. However, there are reports of false-positive results with the newer techniques, especially when the sample tested is formalin-fixed paraffin-embedded tumor tissue [20,21,22].
Even rarer than an uncommon mutation is a compound mutation. This entails a dual mutation on the EGFR gene, comprising a sensitizing mutation (usually 19-Del or a 21 substitution) along with a rare mutation involving other residues of the tyrosine kinase domain of EGFR [5]. In our case, the double mutation was found to be a coexistence of 19-Del and the exon 20 T790M mutation. Compound mutations account for 4–14% of all EGFR-mutated tumors [5, 23, 24]. This frequency variation is due most likely to the fact that multiple methods for mutation detection are used among the studies. One article has independently associated the T790M and drug-sensitive EGFR mutations, establishing the hypothesis that these mutations themselves cause genetic instability, predisposing the cell to more DNA changes [25]. However, there seem to be some combinations that occur more often than others. Some studies have concluded that pretreatment T790M point mutation is significantly more frequent in patients carrying the L858R mutation compared to those harboring deletions in exon 19 [6], making this case even more unusual. Very few case reports of this compound mutation are published. Sakashita et al. [26] presented three cases of EGFR compound mutation, one of them a 19-Del + T790M alteration; their approach was a pathological one. Lou et al. [27] published one similar case but with no clinical description, and Khan et al. published a short report about a 57-year woman harboring the same mutation, with a good response to osimertinib [28]. A summary of cases reported in descriptive studies is presented in Table 1.
There is a paucity of literature about the clinical profile of patients with de novo T790M mutation. Studies in Korea and Japan [34, 35] have described characteristics that are similar to those of patients with an EGFR mutation, regardless of the mutation: female gender, < 65 years of age, never-smoker of tobacco, and adenocarcinoma histology. The differences found were mainly a higher never-smoker of tobacco representation and more brain metastasis. All of these characteristics, including brain metastasis, were present in our patient.
Despite some studies concluding that first-line TKI therapy could benefit patients with a compound mutation harboring a T790M substitution [19, 36], the majority of the literature suggests that compound de novo T790M mutations confer resistance to TKI therapy. Poorer response rates to first-generation and second-generation EGFR-TKIs, along with similar response rates to platinum-based chemotherapy, have been described in this population. However, even though these patients have worse progression-free survival (PFS), there is no statistically significant difference in overall survival (OS) [17, 18, 32, 34,35,36,37]. New therapeutic molecules called third-generation EGFR-TKIs could be the solution for this set of patients, namely osimertinib.
Osimertinib is an orally administered, irreversible EGFR-TKI that is selective for activating EGFR mutations including 19-Del, L858R in exon 21, as well as the common T790M gatekeeper mutation mediating acquired resistance to early generation EGFR-TKIs [38]. Its potency is almost 200-times greater against L858R/T790M than the wild-type EGFR, which minimizes toxicity in patients [39].
Its clinical efficacy has been shown in multiple international trials, namely the AURA1 [40], AURA2 [41], AURA3 [42], and FLAURA [43] trials. The international phase I/II AURA clinical trial (NCT01802632) included patients with locally advanced or metastatic NSCLC with documented EGFR mutation or prior benefit to EGFR-targeted therapy following progression on at least one prior EGFR-TKI. The AURA phase II extension study established the safety and efficacy of osimertinib 80 mg daily as either second-line or third-line therapy in patients with EGFR-mutated NSCLC with confirmed T790M mutation. A pooled study of both the AURA1 extension and the AURA2 revealed a median duration of osimertinib treatment to be 16.4 months, with an improvement in the overall response rate (ORR) which was 66% (262 of 398 patients; 95% CI, 61–70%) and PFS [44]. Of note, there was a trend toward an increased response rate in patients who had co-occurring EGFR T790M mutations with 19-Dels versus EGFR T790M mutations with leucine-to-arginine at codon 858 (L858R) mutations (70 versus 57%) [44].
The AURA3 trial was a randomized international phase III study comparing osimertinib to platinum-pemetrexed chemotherapy combination in patients with T790M-mutated NSCLC following progression on prior EGFR-TKIs [42]. Osimertinib was superior, with a higher ORR (71 versus 31%; p < 0.001) and improved median PFS (10.1 versus 4.4 months, hazard ratio 0.30; 95% CI, 0.23–0.41; p < 0.0001) [42]. Nowadays, upon availability, osimertinib is the therapy of choice for this set of patients.
The FLAURA phase III, double-blinded, international clinical trial compared osimertinib to either gefitinib or erlotinib as initial therapy for patients with advanced EGFR-mutated NSCLC [43]. Longer median PFS was achieved in the osimertinib compared with treatment with standard-of-care first-line EGFR-TKIs (18.9 versus 10.2 months, hazard ratio, 0.46; 95% CI, 0.37 to 0.57; p < 0.001). However, no significant difference in the ORR was seen (80 versus 76%), but the median duration of response was longer with osimertinib (17.2 months) over standard EGFR-TKIs (8.5 months) [43]. Just as in the previous trials, patients with central nervous system (CNS) metastases had a better response to osimertinib. A study evaluating post-progression outcomes with first-line osimertinib versus standard-of-care EGFR-TKIs, provided further confidence in the interim OS data of the FLAURA study and advocated use of osimertinib as first-line therapy for EGFR mutant (EGFRm) advanced NSCLC [45]. The ELIOS trial (NCT03239340), which is ongoing, will assess the tumor genetic and proteomic markers at the point of disease progression in patients with EGFRm NSCLC who receive first-line osimertinib, hopefully providing better guidelines for the use of this drug as first-line treatment. However, further studies comparing second-generation EGFR-TKIs and osimertinib, and a more mature OS data for osimertinib, are needed to make a final decision [46, 47].
Very few data are available regarding the effectiveness of osimertinib in compound mutated EGFR NSCLC, at least in treatment-naïve patients with T790M/19-Del mutated tumors. Zhang et al. stated that first-generation TKIs, including gefitinib, erlotinib, and icotinib, are ineffective even with the presence of sensitive mutations when accompanied by a resistant mutation, while osimertinib carries survival benefits for those patients [48]. Yu et al. found a PFS of only 1.5 months for patients with sensitive and resistant compound mutation treated with first-generation and second-generation EGFR-TKIs [49]. Similar results were also observed in another prospective study, where the ORR and PFS were only 14.3% and 2.9 months, respectively for this set of patients [50]. With these results in mind, using osimertinib as a first line of treatment for patients with NSCLC harboring de novo compound T790M/19-Del mutation, like the one presented in this report, appears to be a sensible decision.
A choice for platinum-based chemotherapy was made for this patient due to the unavailability of third-generation TKIs, a baseline T790M mutation, the presence of multiple metastases, and a high tumor burden.
Conclusion
Even though the rate of baseline T790M mutation is apparently higher than previously known, compound mutations harboring this point substitution are very rare, more so when accompanied by a 19-Del, making this set of patients particularly hard to manage. Osimertinib seems a good choice of treatment for these patients, but in its absence, and until more mature OS data are available and more comparative studies are made, first-line treatment can continue to be platinum-based chemotherapy, especially if there is a high tumor burden. More studies regarding the clinical characteristics of these patients and the appropriate management of this condition are needed to provide the highest standard of care.
References
Ramalingam SS, Owonikoko TK, Khuri FR. Lung cancer: New biological insights and recent therapeutic advances. CA Cancer J Clin. 2011;61(2):91–112. https://doi.org/10.3322/caac.20102.
O’Kane GM, Bradbury PA, Feld R, et al. Uncommon EGFR mutations in advanced non-small cell lung cancer. Lung Cancer. 2017;109:137–44. https://doi.org/10.1016/j.lungcan.2017.04.016.
Shi Y, Au JS, Thongprasert S, et al. A prospective, molecular epidemiology study of EGFR mutations in Asian patients with advanced non-small-cell lung cancer of adenocarcinoma histology (PIONEER). J Thorac Oncol. 2014;9(2):154–62. https://doi.org/10.1097/JTO.0000000000000033.
Rosell R, Moran T, Queralt C, et al. Screening for Epidermal Growth Factor Receptor Mutations in Lung Cancer. N Engl J Med. 2009;361(10):958–67. https://doi.org/10.1056/NEJMoa0904554.
Kobayashi S, Canepa HM, Bailey AS, et al. Compound EGFR mutations and response to EGFR tyrosine kinase inhibitors. J Thorac Oncol. 2013;8(1):118–22. https://doi.org/10.1097/JTO.0b013e3182781e35.
Chen LY, Molina-Vila MA, Ruan SY, et al. Coexistence of EGFR T790M mutation and common activating mutations in pretreatment non-small cell lung cancer: A systematic review and meta-analysis. Lung Cancer. 2016;94:46–53. https://doi.org/10.1016/j.lungcan.2016.01.019.
Dearden S, Stevens J, Wu YL, Blowers D. Mutation incidence and coincidence in non small-cell lung cancer: Meta-analyses by ethnicity and histology (mutMap). Ann Oncol. 2013;24(9):2371–6. https://doi.org/10.1093/annonc/mdt205.
Shigematsu H, Lin L, Takahashi T, et al. Clinical and Biological Features Associated With Epidermal Growth Factor Receptor Gene Mutations in Lung Cancers. JNCI J Natl Cancer Inst. 2005;97(5):339–46. https://doi.org/10.1093/jnci/dji055.
Jorge SEDC, Kobayashi SS, Costa DB. Epidermal growth factor receptor (EGFR) mutations in lung cancer: preclinical and clinical data. Braz J Med Biol Res. 2014;47(11):929–39. https://doi.org/10.1590/1414-431X20144099.
Paez JG, Jänne PA, Lee JC, et al. EGFR mutations in lung cancer: correlation with clinical response to gefitinib therapy. Science. 2004;304(5676):1497–500. https://doi.org/10.1126/science.1099314.
Sharma SV, Bell DW, Settleman J, Haber DA. Epidermal growth factor receptor mutations in lung cancer. Nat Rev Cancer. 2007;7(3):169–81. https://doi.org/10.1038/nrc2088.
Kobayashi S, Boggon TJ, Dayaram T, et al. EGFR Mutation and Resistance of Non–Small-Cell Lung Cancer to Gefitinib. N Engl J Med. 2005;352(8):786–92. https://doi.org/10.1056/NEJMoa044238.
Yu HA, Arcila ME, Rekhtman N, et al. Analysis of tumor specimens at the time of acquired resistance to EGFR-TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin Cancer Res. 2013;19(8):2240–7. https://doi.org/10.1158/1078-0432.CCR-12-2246.
Morgillo F, Della Corte CM, Fasano M, Ciardiello F. Mechanisms of resistance to EGFR-targeted drugs: lung cancer. ESMO Open. 2016;1(3):e000060. https://doi.org/10.1136/esmoopen-2016-000060.
Yun C-H, Mengwasser KE, Toms AV, et al. The T790M mutation in EGFR kinase causes drug resistance by increasing the affinity for ATP. Proc Natl Acad Sci. 2008;105(6):2070–5. https://doi.org/10.1073/pnas.0709662105.
Yu HA, Arcila ME, Hellmann MD, Kris MG, Ladanyi M, Riely GJ. Poor response to erlotinib in patients with tumors containing baseline EGFR T790M mutations found by routine clinical molecular testing. Ann Oncol. 2014;25(2):423–8. https://doi.org/10.1093/annonc/mdt573.
Su KY, Chen HY, Li KC, et al. Pretreatment Epidermal Growth Factor Receptor (EGFR) T790M mutation predicts shorter EGFR tyrosine kinase inhibitor response duration in patients with non-small-cell lung cancer. J Clin Oncol. 2012;30(4):433–40. https://doi.org/10.1200/JCO.2011.38.3224.
Rosell R, Molina MA, Costa C, et al. Pretreatment EGFR T790M Mutation and BRCA1 mRNA Expression in Erlotinib-Treated Advanced Non-Small-Cell Lung Cancer Patients with EGFR Mutations. Clin Cancer Res. 2011;17(5):1160–8. https://doi.org/10.1158/1078-0432.CCR-10-2158.
Fujita Y, Suda K, Kimura H, et al. Highly sensitive detection of EGFR T790M mutation using colony hybridization predicts favorable prognosis of patients with lung cancer harboring activating EGFR mutation. J Thorac Oncol. 2012;7(11):1640–4. https://doi.org/10.1097/JTO.0b013e3182653d7f.
Roma C, Esposito C, Rachiglio AM, et al. Detection of EGFR mutations by TaqMan mutation detection assays powered by competitive allele-specific TaqMan PCR technology. Biomed Res Int. 2013;2013 https://doi.org/10.1155/2013/385087.
Jenkins S, Yang JC, Ramalingam SS, et al. Plasma ctDNA Analysis for Detection of the EGFR T790M Mutation in Patients with Advanced non-small Cell Lung Cancer. J Thorac Oncol. 2017; https://doi.org/10.1016/j.jtho.2017.04.003.
Tatematsu T, Okuda K, Suzuki A, et al. The detectability of the pretreatment EGFR T790M mutations in lung adenocarcinoma using CAST-PCR and digital PCR. J Thorac Dis. 2017;9(8):2397–403. https://doi.org/10.21037/jtd.2017.07.02.
Wu J-Y, Yu C-J, Chang Y-C, Yang C-H, Shih J-Y, Yang P-C. Effectiveness of tyrosine kinase inhibitors on “uncommon” epidermal growth factor receptor mutations of unknown clinical significance in non-small cell lung cancer. Clin Cancer Res. 2011;17(11):3812–21. https://doi.org/10.1158/1078-0432.CCR-10-3408.
Kosaka T, Yatabe Y, Endoh H, Kuwano H, Takahashi T, Mitsudomi T. Mutations of the epidermal growth factor receptor gene in lung cancer: Biological and clinical implications. Cancer Res. 2004;64(24):8919–23. https://doi.org/10.1158/0008-5472.CAN-04-2818.
Hashida S, Soh J, Toyooka S, et al. Presence of the minor EGFR T790M mutation is associated with drug-sensitive EGFR mutations in lung adenocarcinoma patients. Oncol Rep. 2014;32(1):145–52. https://doi.org/10.3892/or.2014.3197.
Sakashita S, Shiba-Ishii A, Murata Y, Sekimoto R, Minami Y, Sato Y, et al. Case report of three EGFR TKI naïve lung adenocarcinoma containing double EGFR mutations (L858R/T790M or Exon 19 Deletion/T790M); Comparing genetic information and histology. Pathol Res Pract. 2018;214:1224–30.
Lou Y, Pecot CV, Tran HT, DeVito VJ, Tang XM, Heymach JV, et al. Germline Mutation of T790M and Dual/Multiple EGFR Mutations in Patients With Lung Adenocarcinoma. Clin Lung Cancer. 2016;17:e5–11.
Khan J, Pritchard CC, Martins RG. Tissue Is the Issue for Diagnosis of EGFR T790M Mutation. J Thorac Oncol. 2016;11(7):e91–2.
Yu X, Zhang X, Zhang Z, Lin Y, Wen Y, Chen Y, et al. First-generation EGFR tyrosine kinase inhibitor therapy in 106 patients with compound EGFR-mutated lung cancer: A single institution’s clinical practice experience. Cancer Commun. 2018;38(1):1–13.
Illei PB, Belchis D, Tseng L-H, Nguyen D, De Marchi F, Haley L, et al. Clinical mutational profiling of 1006 lung cancers by next generation sequencing. Oncotarget. 2017;8(57):96684–96.
Tezel GG, Şener E, Aydın Ç, Önder S. Prevalence of epidermal growth factor receptor mutations in patients with non-small cell lung cancer in Turkish population. Balkan Med J. 2017;34(6):567–71.
Tu H-Y, Ke E-E, Yang J-J, et al. A comprehensive review of uncommon EGFR mutations in patients with non-small cell lung cancer. Lung Cancer. 2017;114(November):96–102. https://doi.org/10.1016/j.lungcan.2017.11.005.
Tang Y, Wang WY, Zheng K, Jiang L, Zou Y, Su XY, et al. EGFR mutations in non-small cell lung cancer: an audit from West China Hospital. Expert Rev Mol Diagn. 2016;16(8):915–9.
Kawamura T, Kenmotsu H, Omori S, et al. Clinical Factors Predicting Detection of T790M Mutation in Rebiopsy for EGFR-Mutant Non-small-cell Lung Cancer. Clin Lung Cancer. 2017; https://doi.org/10.1016/j.cllc.2017.07.002.
Lee Y, Lee GK, Hwang JA, Yun T, Kim HT, Lee JS. Clinical likelihood of sporadic primary EGFR T790M Mutation in EGFR-mutant Lung Cancer. Clin Lung Cancer. 2015;16(1):46–50. https://doi.org/10.1016/j.cllc.2014.09.002.
Fukuoka M, Wu YL, Thongprasert S, et al. Biomarker analyses and final overall survival results from a phase III, randomized, open-label, first-line study of gefitinib versus carboplatin/paclitaxel in clinically selected patients with advanced non-small-cell lung cancer in Asia (IPASS). J Clin Oncol. 2011;29(21):2866–74. https://doi.org/10.1200/JCO.2010.33.4235.
Inukai M, Toyooka S, Ito S, et al. Presence of epidermal growth factor receptor gene T790M mutation as a minor clone in non-small cell lung cancer. Cancer Res. 2006;66(16):7854–8. https://doi.org/10.1158/0008-5472.CAN-06-1951.
Carlisle J, Ramalingam S. Role of osimertinib in the treatment of EGFR-mutation positive non-small-cell lung cancer. Future Oncol. 2019;15:805–16.
Cross DA, Ashton SE, Ghiorghiu S, et al. AZD9291, an irreversible EGFR TKI, overcomes T790M-mediated resistance to EGFR inhibitors in lung cancer. Cancer Discov. 2014;4(9):1046–61.
Janne PA, Yang JC, Kim DW, et al. AZD9291 in EGFR inhibitor-resistant non-small-cell lung cancer. N Engl J Med. 2015;372(18):1689–99.
Yang JC, Ahn MJ, Kim DW, et al. Osimertinib in pretreated T790M-positive advanced non-small-cell lung cancer: AURA study Phase II extension component. J Clin Oncol. 2017;35(12):1288–96.
Mok T, Wu YL, Ahn MJ, Garassino MC, Kim HR, Ramalingam S, et al. Osimertinib or Platinum-Pemetrexed in EGFR T790M-Positive Lung Cancer. N Engl J Med. 2017;376:629–40.
Soria JC, Ohe Y, Vansteenkiste J, et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N Engl J Med. 2018;378(2):113–25.
Ahn MY, Tsai CM, Shepherd FA, Bazhenova L, Sequist LV, Hida T. Osimertinib in Patients With T790M Mutation-Positive, Advanced Non-Small Cell Lung Cancer: Long-Term Follow-Up From a Pooled Analysis of 2 Phase 2 Studies. Cancer. 2019;125:892–901.
Planchard D, Boyer MJ, Lee JS, Dechaphunkul A, Cheema PK, Takahashi T. Post-Progression Outcomes for Osimertinib versus Standard-of-Care EGFR-TKI in Patients with Previously Untreated EGFR-3 Mutated Advanced Non-Small Cell Lung Cancer. Clin Cancer Res. 2019;25:2058–63.
Roeper J, Griesinger F. Epidermal growth factor receptor tyrosine kinase inhibitors in advanced non-small cell lung cancer: what is the preferred first-line therapy? Curr Opin Oncol. 2019;31(1):1–7.
Scott LJ. Osimertinib as first-line therapy in advanced NSCLC: a profile of its use. Drugs Ther Perspect. 2018;34(8):351–7.
Zhang B, Xu JL, Zhang X, Gu P, Wang HM, Wang SY. Coexistence of sensitive and resistant epidermal growth factor receptor (EGFR) mutations in pretreatment non-small cell lung cancer (NSCLC) patients: First or third generation tyrosine kinase inhibitors (TKIs)? Lung Cancer. 2018;117(1):27–31.
Yu HA, Arcila ME, Hellmann MD, et al. Poor response to erlotinib in patients with tumors containing baseline EGFR T790M mutations found by routine clinical molecular testing. Ann Oncol. 2014;25(1):423–8.
Yang JC, Sequist LV, Geater SL, et al. Clinical activity of afatinib in patients with advanced non-small-cell lung cancer harbouring uncommon EGFR mutations: a combined post-hoc analysis of LUX-Lung 2, LUX-Lung 3, and LUX-Lung 6. Lancet Oncol. 2015;16(7):830–8.
Funding
Not applicable.
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
ARZ was the primary caregiver of this oncological patient and was involved in the making of the manuscript. LXR was the geneticist in charge of the diagnostic test and was involved in the making of the manuscript. LFS was the pathologist in charge of the histopathologic diagnostic and was involved in the making of the manuscript. JCB, DE, and JCF were in charge of gathering the information and making the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Falla-Martinez, J.C., Espinosa, D., Baena, J.C. et al. An endothelial growth factor receptor compound mutation of T790M substitution with exon 19 deletion in a previously untreated patient: a case report. J Med Case Reports 13, 144 (2019). https://doi.org/10.1186/s13256-019-2075-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-019-2075-y