Abstract
Background
We describe a case of pemetrexed toxicities related to reabsorption by an ileal neobladder, which caused prolonged hematotoxicity and nephrotoxicity.
Case presentation
A 59-year-old white man was diagnosed with metastatic wild-type adenocarcinoma of the upper lobe of his right lung. After a first cycle of cisplatin and pemetrexed, he had unusually prolonged aplasia and acute kidney injury.
The prolonged aplasia was caused by pemetrexed reabsorption by the ileal mucosa of the neobladder as pemetrexed was eliminated renally in an active form and is partly lipophilic.
Conclusions
Pemetrexed may be reabsorbed by the ileal mucosa of the neobladder because of its hydrophobic structure and renal excretion in its active form. Acute urinary retention may maintain this phenomenon. Published data excluded a potential role for cisplatin in this toxicity; furthermore, we could not assess pemetrexed concentrations in the blood or urine as these assay techniques are not validated. Thus, care is needed when giving chemotherapy to patients with a neobladder.
Similar content being viewed by others
Background
We present a case of pemetrexed toxicities due to reabsorption by an ileal neobladder that occurred in a 59-year-old white man with wild-type metastatic lung adenocarcinoma. He developed unusually extended aplasia and acute kidney injury after a cycle of cisplatin and pemetrexed. We considered that ileal reabsorption of pemetrexed by the neobladder was responsible for the prolonged hematotoxicity. In fact, ileal mucosa absorption is possible because pemetrexed is partly lipophilic and eliminated in an active form.
Case presentation
We report a case of a 59-year-old white man with a metastatic adenocarcinoma of the lung diagnosed in April 2013. This tumor was EGFR (epidermal growth factor receptor), ALK (anaplastic lymphoma kinase), KRAS (V-Ki ras2 Kirsten rat sarcoma viral oncogene homolog), ERBB2 (erb-b2 receptor tyrosine kinase 2), and B-Raf (V-raf murine sarcoma viral oncogene homolog B1) wild-types. He had a previous history of radical cystectomy, prostatectomy, and vesiculectomy and received a Hautmann neobladder in 2001. The neobladder was constructed from ~ 70 cm of distal ileum, which was anastomosed to his ureters and urethra. He initiated cisplatin and pemetrexed chemotherapy, and a vitamin B12 and folic acid supplementation had been prescribed prior to the initiation of treatment.
After 10 days of chemotherapy he was hospitalized because of fever above 39.9 °C. A blood sample showed neutropenia > 0.3 G/L and thrombocytopenia > 21 G/L. Thus, amoxicillin-clavulanate plus ciprofloxacin treatment was started.
On the 4th day after hospitalization he had acute renal failure, metabolic acidosis, hyponatremia, and hyperchloremia.
An abdominopelvic computed tomography (CT) scan showed major distension of the neobladder and bilateral pyelocaliceal dilatation. Urethral catheterization collected 2 L of a gelatinous liquid.
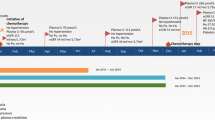
The electrolyte disorders were corrected by 23 days after hospitalization and his renal function was restored at 16 days of hospitalization (Fig. 1). His neutrophil levels became standardized by 22 days after hospitalization and platelets by 34 days after hospitalization. He received several transfusions with platelets (Figs. 2 and 3).
Discussion
Our patient presented unusual hematological adverse effects after a first cycle of chemotherapy. In patients with an advanced stage of non-small-cell lung cancer, pemetrexed is known to cause grade 3 and 4 neutropenia in 15% of cases, grade 3 and 4 thrombocytopenia in 4% of cases [1], and all grades of acute renal failure in 2.4% of cases [2]. In contrast, cisplatin can cause anemia [3], but medullary aplasia is rarely described after only cisplatin [4].
It is to be noted that in patients with locally advanced or metastatic bladder cancer treated with pemetrexed, the hematotoxicity rate is more significant so that cases of grade 3 to 4 neutropenia are up to 75% [5,6,7,8,9,10]. The hematotoxicity seems more important in patients who had cystectomy. Another study, testing intravesical injections of pemetrexed in pigs, highlighted no myelosuppression and no systemic absorption [11].
Because of the hydrophilicity and the low oral bioavailability of cisplatin, it can be assumed that cisplatin was not absorbed by the ileal mucosa. In a phase I study of pemetrexed, 78% of the administrated dose was found in its active form within the urine. Its plasma half-life is ~ 3.1 hours when renal function is normal [12].
During our patient’s urine-retention episode, we supposed that pemetrexed was stored in an active form by the ileal neobladder due to its lipophilic nature, which maintains toxicities. Cisplatin could not have caused this prolonged toxicity because of its hydrophilicity and so could not be reabsorbed by the ileal mucosa.
Conclusions
Pemetrexed was the main cause of the adverse effects observed because of its absorption by the ileal neobladder, with this being exacerbated by our patient’s urinary retention.
It was not possible to determine the plasma and urine concentrations of pemetrexed as these techniques are not routinely validated.
References
Scagliotti GV, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J Clin Oncol Off J Am Soc Clin Oncol. 2008;26:3543–51.
Hazarika M, White RM, Johnson JR, Pazdur R. FDA drug approval summaries: pemetrexed (alimta). Oncologist. 2004;9:482–8.
Kuzur ME, Greco FA. Cisplatin-induced anemia. N Engl J Med. 1980;303:110–1.
Rabik CA, Dolan ME. Molecular mechanisms of resistance and toxicity associated with platinating agents. Cancer Treat Rev. 2007;33:9–23.
von der Maase H. A phase II trial of pemetrexed plus gemcitabine in locally advanced and/or metastatic transitional cell carcinoma of the urothelium. Ann Oncol. 2006;17:1533–8.
Dreicer R, et al. Phase 2 trial of pemetrexed disodium and gemcitabine in advanced urothelial cancer (E4802): a trial of the eastern cooperative oncology group. Cancer. 2008;112:2671–5.
Sweeney CJ, Phase II. Study of pemetrexed for second-line treatment of transitional cell cancer of the urothelium. J Clin Oncol. 2006;24:3451–7.
Choi YJ, et al. Phase II study of pemetrexed in combination with cisplatin in patients with advanced urothelial cancer: the PECULIAR study (KCSG 10–17). Br J Cancer. 2015;112:260–5.
Galsky MD, et al. Phase II trial of pemetrexed as second-line therapy in patients with metastatic urothelial carcinoma. Invest New Drugs. 2007;25:265–70.
Hutson TE, et al. Phase I study of a 3-drug regimen of gemcitabine/cisplatin/pemetrexed in patients with metastatic transitional cell carcinoma of the urothelium. Invest New Drugs. 2008;26:151–8.
Hendricksen K. Potential and toxicity of intravesical pemetrexed: a preclinical study in pigs. Clin Cancer Res. 2006;12:2597–601.
Rinaldi DA, et al. A phase I evaluation of multitargeted antifolate (MTA, LY231514), administered every 21 days, utilizing the modified continual reassessment method for dose escalation. Cancer Chemother Pharmacol. 1999;44:372–80.
Acknowledgements
Not applicable.
Funding
None.
Availability of data and materials
Available.
Author information
Authors and Affiliations
Contributions
LS, JP, and HP wrote the article; DMS helped with patient management and medical reasoning when writing the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sakhri, L., Pinsolle, J., Moro-Sibilot, D. et al. Unusually prolonged pemetrexed cytotoxicity in a patient with a lung adenocarcinoma: a case report. J Med Case Reports 11, 262 (2017). https://doi.org/10.1186/s13256-017-1436-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-017-1436-7