Abstract
Background
In 2014–2015, the largest international survey of insulin injection technique in patients with diabetes taking insulin was conducted in 42 countries, totaling 13,289 participants. In Brazil, patients from five public health centers were included. This study aims to evaluate insulin injection technique in Brazilian patients and compare results with Latin America (LatAm) and World data.
Methods
The insulin Injection Technique Questionnaire (ITQ) survey consisted of an initial patient section (questions applied by an experienced nurse), followed by observation of injection technique and examination of the injection sites by the health care professional.
Results
In Brazil, 255 patients were evaluated: 25% had type 1 diabetes mellitus (T1DM) and 75% had T2DM. In this study, 79% of patients injected less than 4 times a day, and 17.3% used insulin pens, compared to 28% in LatAm and 86% worldwide. Syringes were used by 78% of patients in Brazil, compared to 65% in LatAm and 10% globally. Differences in needle length were substantial—nearly 64% in Brazil inject with 8 mm length needle compared to 48% in LatAm and 27% worldwide. Additionally, 48% of patients in Brazil skip doses, 80% reuse pen needles and 57% reuse syringes with 27% having lipohypertrophy by exam.
Conclusion
Brazilian patients use syringes more and pens less, inject with larger needles and have more lipohypertrophy when compared to Latin America and World data. Their re-use of needles and syringes is also high. This study showed that in Brazil, teaching of proper injection technique has to be more widespread, and more intensive during diabetes educational sessions, and the type of delivered supplies must be updated to smaller, shorter needles preferred by patients, in order to facilitate adherence to treatment. From the ITQ, we conclude that there are many aspects of insulin injection technique that may be improved in Brazil.
Similar content being viewed by others
Background
According to the 2017 international diabetes federation (IDF) Diabetes Atlas, Brazil has about 12.4 million people with diabetes, the highest number compared to South and Central American countries, and nearly 88,300 children and adolescents with type 1 diabetes, making it the country with the third highest number of children with diabetes in the world [1].
Recent nationwide and regional studies showed that glucose control is out of ideal range in the majority of patients. The strongest association of high HbA1c levels was with low or very low socioeconomic backgrounds [2,3,4]. Patients with this background are usually less educated in relation to diabetes care. Many researches have demonstrated that improvement in insulin injection technique after educational interventions has significant impact in glucose control and HbA1c levels, besides also lowering total daily dose of insulin [5,6,7,8]. The correct technique of re-suspension of cloudy insulin, advice on rotation sites, education on avoiding lipohypertrophy and the correct choice of sites of insulin injection have an impact on insulin pharmacodynamics and consequently on glucose variability and control [9,10,11]. So, the knowledge about insulin injection techniques in Brazilian patients is of great interest, to understand if it is one of the components leading to the sub-optimal glycemic control found in our population.
In 2014–2015 an international survey of patients taking insulin for at least 6 months was conducted in 42 countries, with a total of 13,289 patients evaluated. The intention was to study many countries to provide a representative global analysis of diabetes care, epidemiologic aspects, variations in injection techniques and its outcomes. The global results were published in 2016 [12, 13], becoming an important source of information and also providing data for new recommendations of insulin injection [14]. As the raw data of the original study is available, it is possible to individualize the results by country. Our aims were: a- to evaluate Brazil´s results of injection techniques in patients with diabetes, and b- to compare these results with Latin America and Worldwide data.
Methods
In Brazil, a total of 255 patients from five public health centers were included. All centers were specialized in diabetes treatment, serving as secondary and tertiary care from the public national health service, in five Brazilian geographic regions: two from Southeast, one from Mid-west and two from South. There was no financial incentive to enroll [12].
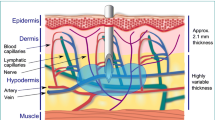
The insulin Injection Technique Questionnaire (ITQ) survey consisted of an initial patient section (applied by an experienced nurse) followed by a second section, performed by the patient’s diabetes educator, nurse or physician, when they observed patient injection technique and carefully examined the injection sites. The technique was considered correct when executed as follows: first gently lift a skinfold, then inject the insulin slowly at a 90° angle to the surface of the skinfold, let the needle remain in the skin for a count of 10 after the plunger is pressed down (when using a pen), withdraw the needle from the skin at the same angle it was inserted, only when the needle is completely removed release the skinfold, and at last dispose of the used needle safely [12, 15]. Detailed information about the development of the survey can be found in the original article [12]. Patient demographic data included age, sex, type of diabetes, years with diabetes, years injecting, and devices used. The key insulin injection parameters selected by our analysis were as follows: current practice (injection device and needle length, number of injections per day, use and characteristics of lifted skinfolds (pinch-up), needle entry angle, site rotation, dwell time of needle under the skin, site inspection by a health care professional, needle reuse, sharps disposal), observed anomalies at injection sites (lipohypertrophy), knowledge about injections (identity of trainer, themes covered in injection training), and disposal habits for used sharps [12, 13].
In this analysis, we report results from Brazil, Latin America, and World data, the latter including those respondents from Brazil, which represent less than 2% of the total survey.
All the participants had diabetes and had been injecting insulin for at least 6 months before taking the survey. Each center applied the questionnaire to roughly 25 patients on a sequential basis as consenting and eligible patients entered the clinic, in order to eliminate any bias in the selection. In a survey of this size, not every question was answered by every patient, and small differences for certain parameters may be statistically significant due to the large numbers.
A total number of 13,289 patients from 42 countries participated, in Latin America were 603 and in Brazil were 255. As this was a global survey, there were questions that were not answered and other were not completely clear, so they were excluded from the analyzed data. When such thing happened, the percentages were calculated according to the data that were considered clearly provided. For that reason, the N may vary from one table to another.
The study was conducted according to Good Clinical Practices and the Helsinki accords, and subject identity was kept confidential at all times. Participants were required to provide verbal consent to participate in the study and were informed that they were not put at risk by the study, and that their care would not be affected. Therefore, ethics committee approval was not generally required, but was obtained whenever specifically requested by a center.
Statistical analysis was IBM SPSS Statistics for Windows software, Version 19 (IBM Corp) was used to perform the data analysis. Descriptive statistics, frequencies, and rankings were calculated. Two-tailed tests were used in all the analyses. Initially, results from each of the 42 countries were analyzed independently, and only when the distributions of key demographic parameters (age, sex, body mass index [BMI], and duration of diabetes) were found to be comparable were all the data pooled into an overall database. The threshold for staying in the model was P < .05.
Results
The sample studied in Brazil, Latin America and World is described in Table 1. From the total of 255 patients in Brazil, 25% of patients had type 1 diabetes mellitus (T1DM) and 73% had type 2 diabetes mellitus (T2DM). Duration of diabetes, years taking insulin, TDD insulin and mean HbA1c were similar in Brazil, Latin America, and worldwide (Table 1).
Regarding the number of injections per day, 79% of patients in Brazil injected less than 4 times a day, compared to 54% worldwide, and 78% in Latin America.
The use of devices to deliver insulin by patients from Brazil was markedly different from the rest of the world (Table 2): syringe use was nearly 8 times more common in Brazil than worldwide.
When questioned about needle length, patients in Brazil were using longer needles than in Latin America and in the world (Table 3). Regarding remix of cloudy insulin, 93% said that they did it, but only 15% reported to roll it 20 times. More importantly, 76% referred to roll 10 times or less.
The nurses assessed the injection techniques in practice, so the information provided by the patient when filling the questionnaire could be compared with what they do in practice. When asked about rotation of application, 86% of patients responded that they did so, but only 59% of them did it correctly when assessed by the nurse. Worldwide, 83.9% reported rotating their injection sites, and 70.6% did so correctly per nurse inspection.
When questioned if sometimes they skipped doses, 48% reported they did, and 37% skipped them several times a month. Almost one third (33%) said the reason for skipping doses was that they forgot to inject.
Table 4 shows that needle reuse—with both pens and syringes—is common worldwide (56% and 39%), but even more so in Brazil (80% and 57%) and in LatAm (71% and 61%). Saving money and convenience were frequent explanations.
When examined by the nurse, 27% had lipohypertrophy (LH) − 39% reported to inject into LH sometimes or always, and 69% justified that they did it because it was a routine. When asked about examination of their injection sites, 55% of the patients said that they could not recall it ever being done, compared to 38.9% worldwide.
Of all the patients, 37% were trained by a diabetes nurse, 31% by a general nurse, and the others don’t remember having been trained. Regarding some specific topics, more than 40% don’t remember to have ever been trained about how long they should keep the needle (44%), how to mix insulin (41%), what is the injection depth (44%) or how long to keep skin fold (49%).
Regarding the time patients maintained the needle under the skin during injection, 25% kept the injection for less than 5 s, 44% between 5 and 10 s, and 26% more than 10 s (5% didn´t know). About skin fold, 70% did it correctly, but only 39% released the skin fold only when the needle is removed.
In Brazil, the initial disposal for sharps (where do you put the used sharp?) was into specially made containers in 38% and home container (such as a used one for laundry detergent) in 38% of the patients, compared to 21% and 23%, respectively, worldwide. Roughly one-fifth (21%) of Brazil patients said they put their used sharp into the trash, with the cap on—less than half of the 48% who reported this, worldwide. The final disposal (what do you do with the waste?) was to take it to the hospital in 74% of the surveys.
Discussion
Insulin injection technique is part of diabetes education and essential for achieving optimal diabetes control. The ITQ survey involved 13,289 patients from 42 countries and revealed many important aspects of insulin injection all over the world. The amount of data obtained generated important information and was used to revise guidelines in the light of new recommendations [14, 16]. Due to its large size, it is possible to extract data to evaluate individual countries separately, provided the specific number of patients is sufficient. In this study, we wanted to know Brazil-specific data, and also compare its results with other regions. We opted to evaluate Latin America and the World results, so we would have a taste of regional and global practices, and see if they differed from ours.
While there are a number of interesting findings revealed by the ITQ survey, the most striking difference between insulin-taking patients in Brazil and the rest of the world is the nature of the devices that patients use. In Brazil, approximately, only 17% uses insulin pens, compared to 86% worldwide. Syringes, approximately, are used by 78% of injecting patients in Brazil (with a small number using both), compared to 9% globally. Needle length is also notable—nearly 64% in Brazil inject with an 8 mm length needle, compared to 27% worldwide. The 4 mm pen needle, introduced in 2010, is now used by more than one-fifth of injecting patients globally—a notable change—whereas less than 8% do so in Brazil. Most of the world has undergone a major “shift-to-short” in terms of insulin delivery needles, whereas this has lagged in Brazil. The likely reason is that the public health system provides most of the devices used by patients, and usually those devices are syringes with 8 mm needles. The published literature consistently shows favorable findings for use of short needles instead of longer ones, including in obese patients taking large injections of insulin [17,18,19,20]—glycemic control is the same, there is no increase in leakage or backflow of insulin from the skin, and pain is reduced. Patients consistently prefer the shorter needles, overall. The risk of inadvertent IM injection is also lowest with the 4 mm length needle (or 6 mm for syringes). Based on this evidence, the post-FITTER Injection Technique Recommendations [14] strongly recommend use of the 4 mm needles as the safest for all patients, including both children and adults, and these have been reflected in the official Brazilian Diabetes Society (SBD) Positioning Statement published online in March 2017 [16].
Most patients in Brazil with T2DM uses NPH and Regular insulin and, on average, spend more years in treatment on oral medicines than the world average. When they are already taking insulin, basal insulin doses (NPH or analogues) are higher than the world average, and the doses of bolus insulin (R and fast analogues) are much lower. Considering that 85.8% of patients use NPH insulin, knowing that only 15% report re-suspending cloudy insulin correctly is alarming. The recommendations suggest performing at least 20 soft movements, and not doing it properly may influence the absorption and action of the injected insulin, substantially [9,10,11].
As for the number of injections/day, in Brazil 21% make 4 or more injections/day while in the world 46% do so. In a large previous study in Brazil, from the 5750 patients with Type 2 diabetes, 35% injected insulin and 58% of those did 2 injections/day [3, 4]. This suggests that we have more difficulty in establishing intensive insulin therapy, which is currently recommended for patients DM1 or DM2 (when indicated). Mean HbA1c in Brazil, Latin America and the world is still far from the 7% value related to a lower risk of progression of microvascular damage. The attainment of this target of treatment is achieved far more effectively with intensive treatment [21].
The assessment of the injection technique is also very relevant in this study, since the information filled out by the patient in the questionnaire was confirmed with the observation of the nurses in practice. The difference between what the patient “thinks he does” and what he “actually does” shows how important it is to review the technique regularly and not only briefly question it theoretically. The main protective factor for the development of lipohypertrophy is the proper rotation of application sites or regions [22, 23]. In the questionnaire, 86% of the patients referred to doing the rotation, but according to the nurse only 59% did it correctly. Correct site rotation involves moving from one injection to the next by at least one finger-width (about 1 cm) in a pattern such as a line, or a circle, or a square within a region, and between regions as well [13, 14]. The main reasons for incorrect rotation, according to other studies, could be not only the lack of information, but also the assumption that lipohypertrophic areas are less painful and also rooted habits [24]. As for the skin fold, which is very important when using needles longer than 5 mm [25], 70% of the patients did the pinch correctly, but only 39% removed the needle before releasing the skin fold.
A major fact in this aspect is that more than 40% of patients report never having received guidance on how long they should keep the needle on the skin after the application, how deep the needle should penetrate, how long they should keep the fold.
Results showed that reuse of needles and syringes are higher in Brazil than in other parts of the world, mainly due to costs and convenience. Interestingly, the reuse of pen needles is higher than syringes, probably due to government supply of syringes, but not pen needles. Important to mention that there is a current debate, confronting the positions of the Ministry of Health, allowing the reuse of needles and the Brazilian Diabetes Society, which recommends no reuse [16, 26]. The main issue, costs aside, is that although patients can reuse needles and do not get local infections or abscesses, the needles do become duller, and using needles by roughly 5 times or more is strongly associated with prevalence of lipohypertrophy [13, 14].
Regarding lipohypertrophy (LH), nearly 32% said they “have lumps at injection sites that have been present for weeks, months, or years”, and 27% presented a lump at one or more of the injection sites on physical examination. The presence of LH is mainly related to incorrect rotation of sites, but also to the frequency of reuse of needles and therapy with insulin for longer periods [13, 22,23,24, 27]. The presence of LH is associated with higher glycated hemoglobin values (up to 0.5% higher) and higher total daily insulin doses (5–15 U/day) [5, 6, 8, 22, 23, 27]. Intervention with intensive educational measures regarding insulin delivery techniques has shown a reduction in LH, glycated hemoglobin and daily insulin doses, thus promoting improved quality of life for the patient, therapeutic efficacy and lower costs related to insulin therapy and chronic complications due to poor glycemic control, although there are limitations to each of these reports [5, 6, 8, 22, 23, 27].
The information about sharps disposal seems to be clearer, though. While in the world about 48% of patients put used needles (recapped) in the common garbage, according to ITQ in Brazil more than 76% is discarded in appropriate containers at home and at health services, which are committed to properly dispose of waste. In another Brazilian study, in Ceará, 50% of the patients reported having received guidance about sharps disposal, but 57.1% did so in common trash [28]. These discrepancies could be explained by the fact that this study was done in reference centers, and also because the distribution of proper containers by the government is variable, results depending on which State of the Federation the survey was performed.
Brazil is a country with continental dimensions, and therefore presents particularities when the demographic profile is evaluated. In this study, the five participating centers were from predominantly urbanized regions and referenced care for diabetes treatment. It is possible that the national scenario is even less favorable in some respects, similar to the ITQ data presented in India [29], where primary care and insulin delivery guidelines are also performed by general practitioners in very quick consultations, without the support of nurses specialized in diabetes and having only the medications and supplies available in the public health system.
The characteristic of the Brazilian health system has also unique characteristics, difficult to balance in the development of a study like this one. About 24% of the Brazilian population relies on private healthcare, varying from 5% to more than 70% of coverage depending on the state [30]. There is evidence that the patients who receive diabetes medical care at private services have lower HbA1c than those who depends of the public health system [4]. Interestingly, in this survey we found similar HbA1c in Brazil, Latin America and the World, regardless of all the differences found in injection technique, type of insulin, devices used and total insulin daily dose. This is in accordance with the known difficulties patients with diabetes have in obtaining a good metabolic control all over the globe [1, 4, 21]. The public health system provides NPH and Regular insulin for free, and needles, syringes, lancets and reagent strips for blood glucose monitoring. In special cases some patients also receive free analog insulin, pens and needles for pens for application. Generally speaking, most patients uses what is provided by the state, while those who have some financial capacity buy their own medicines and supplies and often can choose between spending with better insulin or with pen needles. This shows that the choice of insulin and the devices may not be what the doctor considers best for that patient specifically, but what he or she has available for use according to the health system and the patient’s purchasing power.
The limitation of this study is related to the fact that the participating centers may not reflect the reality of all the regions of the country. The strengths are the large number of patients evaluated, the appraisal about many aspects of insulin treatment and the possibility to compare different countries within the same protocol. Its results can contribute to the comprehension of the care of diabetes in the country, helping the development of better health policies.
Conclusions
Data from ITQ Brazil allow us to conclude that there are many aspects of insulin injection that need to be improved. Brazilian patients are using more syringes and less pens, are being exposed to larger needles and are having more lipohypertrophy when compared to Latin America and World data. Their re-use of needles and syringes is also higher than worldwide. After the ITQ was published, the Brazilian Diabetes Society proposed a new guideline about insulin injections [16], and the information is being spread by many kinds of media. The ITQ study showed that, in Brazil, teaching of proper injection techniques has to be more intensively widespread during diabetes educational sessions, and the delivery of supplies updated, in order to increase adherence to treatment.
Abbreviations
- BMI:
-
body max index
- DM:
-
diabetes mellitus
- HbA1c:
-
glycated hemoglobin
- ITQ:
-
Insulin Injection Technique Questionnaire
- LatAm:
-
Latin America
- LH:
-
lipohypertrophy
- NPH:
-
neutral protamine Hagedorn
- T1DM:
-
type 1 diabetes mellitus
- T2DM:
-
type 2 diabetes mellitus
- TDD:
-
total daily dose
References
IDF DIABETES ATLAS. Eighth edition. 2017. http://www.diabetesatlas.org. Accessed 17 Dec 2017.
Viana LV, Leitão CB, Kramer CK, et al. Poor glycemic control in Brazilian patients with type 2 diabetes attending the public healthcare system: a cross-sectional study. BMJ Open. 2013;3:e003336. https://doi.org/10.1136/bmjopen-2013-003336.
Andrade CS, Ribeiro GS, Santos CAST, et al. Factors associated with high levels of glycated haemoglobin in patients with type 1 diabetes: a multicentre study in Brazil. BMJ Open. 2017;7(12):e018094. https://doi.org/10.1136/bmjopen-2017-018094.
Gomes MB, Cobas RA, Matheus AS, et al. Regional differences in clinical care among patients with type 1 diabetes in Brazil: Brazilian Type 1 Diabetes Study Group. Diabetol Metab Syndr. 2012;4(1):44. https://doi.org/10.1186/1758-5996-4-44.
Grassi G, Scuntero P, Trepiccioni R, et al. Optimizing insulin injection technique and its effect on blood glucose control. J Clin Transl Endocrinol. 2014;1(4):145–50. https://doi.org/10.1016/j.jcte.2014.07.006.
Campinos C, Le Floch JP, Petit C, et al. An effective intervention for diabetic lipohypertrophy: results of a randomized, controlled, prospective multicenter study in France. Diabetes Technol Ther. 2017;19(11):623–32. https://doi.org/10.1089/dia.2017.0165.
Guo XH, Ji LN, Lu JM, et al. Efficacy of structured education in patients with type 2 diabetes mellitus receiving insulin treatment. J Diabetes. 2014;6(4):290–7. https://doi.org/10.1111/1753-0407.12100.
Nakatani Y, Matsumura M, Monden T, et al. Improvement of glycemic control by re-education in insulin injection technique in patients with diabetes mellitus. Adv Ther. 2013;30(10):897–905. https://doi.org/10.1007/s12325-013-0066-8.
Milech A, Angelucci AP, Golbert A, et al. Sociedade Brasileira de Diabetes. Práticas seguras para o preparo e aplicação de insulinas. Diretrizes da Sociedade Brasileira de Diabetes 2014–2015. http://www.diabetes.org.br/profissionais/images/pdf/diabetes-tipo-1/002-Diretrizes-SBD-Aplicacao-Insulina-pg219.pdf. Accessed 16 Feb 2018.
Brown A, Steel JM, Duncan C, et al. An assessment of the adequacy of suspension of insulin in pen injectors. Diabet Med. 2004;21(6):604–8. https://doi.org/10.1111/j.1464-5491.2004.01206.x.
Kaiser P, Maxeiner S, Weise A, et al. Assessment of the mixing efficiency of neutral protamine Hagedorn cartridges. J Diabetes Sci Technol. 2010;4(3):652–7. https://doi.org/10.1177/193229681000400320.
Frid AH, Hirsch LJ, Menchior AR, et al. Worldwide injection technique questionnaires study: population parameters and injection practices. Mayo Clin Proc. 2016;91(9):1212–23. https://doi.org/10.1016/j.mayocp.2016.06.011.
Frid AH, Hirsch LJ, Menchior AR, et al. Worldwide injection technique questionnaire study: injecting complications and the role of the professional. Mayo Clin Proc. 2016;91(9):1224–30. https://doi.org/10.1016/j.mayocp.2016.06.012.
Frid AH, Kreugel G, Grassi G, et al. New insulin delivery recommendations. Mayo Clin Proc. 2016;91(9):1231–55. https://doi.org/10.1016/j.mayocp.2016.06.010.
Vianna MS, Silva PAB, Nascimento CVD, Soares SM. Self-care competence in the administration of insulin in older people aged 70 or over. Rev Lat Am Enfermagem. 2017;30(25):e2943. https://doi.org/10.1590/1518-8345.2080.2943.
Posicionamento Oficial SBD número 01/2017. Recomendações sobre o tratamento injetável do diabetes: insulinas e incretinas. http://www.diabetes.org.br/profissionais/publicacoes/diretrizes-e-posicionamentos-1. Accessed 16 Feb 2018.
Schwartz S, Hassman D, Shelmet J, et al. Multicenter, open-label, randomized, two-period crossover trial comparing glycemic control, satisfaction, and preference achieved with a 31 gauge × 6 mm needle versus a 29 gauge × 12.7 mm needle in obese patients with diabetes mellitus. Clin Ther. 2004;26(10):1663–78. https://doi.org/10.1016/j.clinthera.2004.10.007.
Hirsch LJ, Gibney MA, Albanese J, et al. Comparative glycemic control, safety and patient ratings for a new 4 mm × 32 G insulin pen needle in adults with diabetes. Curr Med Res Opin. 2010;26(6):1531–41. https://doi.org/10.1185/03007995.2010.482499.
Bergenstal RM, Strock ES, Peremislov D, et al. Safety and efficacy of insulin therapy delivered via a 4mm pen needle in obese patients with diabetes. Mayo Clin Proc. 2015;90(3):329–38. https://doi.org/10.1016/j.mayocp.2014.12.014.
Kreugel G, Keers JC, Kerstens MN, et al. Randomized trial on the influence of the length of two insulin pen needles on glycemic control and patient preference in obese patients with diabetes. Diabetes Technol Ther. 2011;13(7):737–41. https://doi.org/10.1089/dia.2011.0010.
Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86. https://doi.org/10.1056/NEJM199309303291401.
Blanco M, Hernández MT, Strauss KW, et al. Prevalence and risk factors of lipohypertrophy in insulin-injecting patients with diabetes. Diabetes Metab. 2013;39(5):445–53. https://doi.org/10.1016/j.diabet.2013.05.006.
Ji L, Sun Z, Li Q, et al. Lipohypertrophy in China: prevalence, risk factors, insulin consumption, and clinical impact. Diabetes Technol Ther. 2017;19(1):61–7. https://doi.org/10.1089/dia.2016.0334.
Partanen T, Rissanen A. Insulin injection practices. Pract Diab Int. 2000;2000(17):252–4. https://doi.org/10.1002/pdi.91.
Hirsch L, Byron K, Gibney M. Intramuscular risk at insulin injection sites—measurement of the distance from skin to muscle and rationale for shorter-length needles for subcutaneous insulin therapy. Diabetes Technol Ther. 2014;16(12):867–73. https://doi.org/10.1089/dia.2014.0111.
BRASIL. Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Diabetes Mellitus. Brasília, 2006 (Cadernos de Atenção Básica, n. 16).
Misnikova IV, Gubkina VA, Lakeeva TS, et al. A randomized controlled trial to assess the impact of properinsulin injection technique training on glycemic control. Diabetes Ther. 2017;8(6):1309–18. https://doi.org/10.1007/s13300-017-0315-y.
Cunha GHD, Barbosa RVA, Fontenele MSM, et al. Insulin therapy waste produced in the households of people with diabetes monitored in Primary Care. Rev Bras Enferm. 2017;70(3):618–25. https://doi.org/10.1590/0034-7167-2016-0406.
Kalra S, Mithal A, Sahay R, et al. Indian injection technique study: population characteristics and injection practices. Diabetes Ther. 2017;8(3):637–57. https://doi.org/10.1007/s13300-017-0243-x.
Agencia Nacional de Saúde - downloaded from http://www.ans.gov.br/perfil-do-setor/dados-gerais. Accessed Feb 2018.
Authors’ contributions
LEC participated in analyzing the data and writing the article. LC was responsible for capturing the data and writing. BT, HCP, RR, and APN generated data and participated in the writing. LH and KS idealized the survey, pooled data and participated in the writing. All authors read and approved the final manuscript.
Acknowledgements
We thank the patients and the centers that participated of the study: Diabetes, Education and Control Group, Kidney Hospital—São Paulo/SP; Endocrinology Unit and Research Center at Taguatinga Regional Hospital, Brasília, DF; Diabetes Unit, Department of Endocrinology and Metabolism, Federal University of Paraná—Curitiba/PR; Institute of Children with Diabetes—Porto Alegre/RS and Department of Nursing Services, Federal University of Triângulo Mineiro—Uberaba/MG.
Competing interests
LH and KS are employees of BD, sponsor of the study.
Availability of data and materials
The datasets generated and/or analyzed during the current study are available in the ITQ survey data Tableau Public Adam Young’s Profile website [http://tabsoft.co/23V6ofi].
Consent for publication
Not applicable.
Ethics approval and consent to participate
Obtained upon request. Not applicable in this data mining method.
Funding
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Calliari, L.E., Cudizio, L., Tschiedel, B. et al. Insulin Injection Technique Questionnaire: results of an international study comparing Brazil, Latin America and World data. Diabetol Metab Syndr 10, 85 (2018). https://doi.org/10.1186/s13098-018-0389-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-018-0389-3