Abstract
Background
Multiple myeloma is a plasma cell tumour with approximately 5500 new cases in the UK each year. Ixazomib is a next generation inhibitor of the 20S proteasome and is thought to be an effective treatment for those who have relapsed from bortezomib. The combination of cyclophosphamide and dexamethasone (CD) is a recognised treatment option for patients with relapsed refractory multiple myeloma (RRMM) who have relapsed after treatment with bortezomib and lenalidomide, whilst also often being combined with newer proteasome inhibitors. The most apparent combination for ixazomib is therefore with CD.
Methods
MUK eight is a randomised, controlled, open, parallel group, multi-centre phase II trial that will recruit patients with RRMM who have relapsed after treatment with thalidomide, lenalidomide, and a proteasome inhibitor. The primary objective of the trial is to evaluate whether ixazomib in combination with cyclophosphamide and dexamethasone (ICD) has improved clinical activity compared to CD in terms of progression-free survival (PFS). Secondary objectives include comparing toxicity profiles and the activity and cost-effectiveness of both treatments. Since opening, the trial has been amended to allow all participants who experience disease progression (as per the IMWG criteria) on the CD arm to subsequently switch to receive ICD treatment, once progression has been confirmed with two clinical members of the Trial Management Group (TMG). This ‘switch’ phase of the study is exploratory and will assess second progression-free survival measured from randomisation to second disease progression (PFS2) and progression-free survival from the point of switching to second disease progression (PFS Switch) in participants who switch from CD to ICD treatment.
Discussion
Development of ixazomib offers the opportunity to further investigate the value of proteasome inhibition through oral administration in the treatment of RRMM. Previous studies investigating the safety and efficacy of ICD in patients with RRMM demonstrate a toxicity profile consistent with ixazomib in combination with lenalidomide and dexamethasone, whilst the combination showed possible activity in RRMM patients. Further investigation of the anti-tumour effect of this drug in RRMM patients is therefore warranted, especially since no trials comparing CD with ICD have been completed at present.
Trial registration
ISRCTN number: ISRCTN58227268. Registered on 26 August 2015.
Similar content being viewed by others
Background
Multiple myeloma (MM) is a malignancy of plasma cells, characterised by proliferation of these cells in the bone marrow and, usually, abnormal secretion of monoclonal immunoglobulins. In 2015, there were 5540 new cases of MM in the UK, an age-standardised incidence of 9.3 per 100,000 population in patients with a new cancer diagnosis, and in 2014, there were 2928 deaths from the disease [1]. Survival rates for MM have improved significantly in recent decades, with 77% of patients in England and Wales currently surviving for at least 1 year following diagnosis, compared to 37% 40 years ago. Ten-year survival rates have increased from 6 to 33% in the same time period [1]. Despite these improvements, which can be attributed to advances in both diagnostics and treatment, MM is incurable and the majority of patients will at some point require further therapy for relapsed disease.
Treatment options for relapsed patients include both conventional cytotoxic agents, newer immunomodulatory agents and proteasome inhibitors, and autologous stem cell transplantation (ASCT). As with treatment for primary disease, a combination of treatments is commonly employed. However, many patients are either refractory to treatment using existing approved regimens, or will relapse after an initial response. Investigation of further treatment options for these patients is therefore required.
Ixazomib is a next generation, small molecule inhibitor of the 20S proteasome that is under development for the treatment of non-haematological malignancies, lymphoma, MM, and other plasma cell dyscrasias. Inhibition of the 20S proteasome has previously been validated as a therapeutic target for the treatment of malignancies using bortezomib [2]; however, some patients do not respond to bortezomib or develop resistance to this drug. Ixazomib is structurally and pharmacologically distinct from bortezomib and is orally bioavailable. Furthermore, it has already been shown to be well-tolerated, with a favourable toxicity profile and promising efficacy [3,4,5,6].
The Myeloma UK (MUK) study, MUK eight, has been developed to further investigate the potential of ixazomib for treatment of relapsed/refractory multiple myeloma (RRMM) (Fig. 1). For patients with RRMM who have relapsed after treatment with thalidomide, lenalidomide and a proteasome inhibitor, the combination of cyclophosphamide and dexamethasone (CD) is a recognised treatment option alternative to a novel therapy. CD is also already regularly used, to good effect, in combination with newer agents including bortezomib. Therefore in the RRMM setting, the most apparent combination for ixazomib is with CD.
The study has been developed through the MUK Early Phase Clinical Trials Network (CTN), an innovative collaboration which brings together clinical specialists and researchers, the pharmaceutical industry and NHS regulatory bodies to conduct a prioritised and strategic portfolio of myeloma clinical trials [7].
Current protocol: V3.0, 23/05/2017.
Methods
Study aim
The MUK eight study will evaluate the clinical effectiveness of ixazomib in combination with cyclophosphamide and dexamethasone (ICD), as compared to the combination of cyclophosphamide and dexamethasone alone (CD), in terms of progression-free survival (PFS): the time from randomisation to first disease progression. MUK eight will recruit patients with RRMM who have relapsed after treatment with thalidomide, lenalidomide and a proteasome inhibitor.
Study design
MUK eight is designed as a randomised, controlled, open, parallel group, multi-centre phase II trial. A maximum of 250 participants will be recruited and randomised on a 1:1 basis to receive either ICD or CD.
Since opening, in order to increase appeal of the control arm, the trial has been amended to allow all participants who experience disease progression (as per the IMWG criteria) on the CD arm to subsequently switch to receive ICD treatment, once progression has been confirmed by two clinical members of the Trial Management Group (TMG).
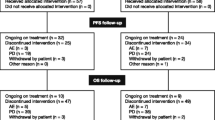
This phase will assess second progression-free survival measured from randomisation to second disease progression (PFS2) and progression-free survival from the point of switching to second disease progression (PFS Switch), as detailed in Fig. 2, in participants who switch from CD to ICD treatment. Participants who progress on the ICD arm will be followed up but treated off-trial as per standard practice.
Explanation of PFS endpoints. *After patients randomised to the CD arm reach disease progression, they are given the option to switch to ICD treatment until they disease progress a second time. Patients randomised to the ICD arm that reach disease progression will be followed-up but treated off-trial as per standard practice
Primary objective
To evaluate whether ICD has improved clinical activity compared to CD in terms of progression-free survival (PFS), in patients with RRMM who have relapsed after treatment with thalidomide, lenalidomide and a proteasome inhibitor.
Secondary objectives
-
To further evaluate the clinical activity of ICD with regard to additional secondary endpoints, detailed in Table 3
-
To determine the safety and toxicity profile of ICD compared to CD
-
To estimate the cost-effectiveness of ICD compared to CD
-
To determine quality of life with ICD compared to CD
-
To assess the impact of baseline Charlson index score on PFS, overall survival and deliverability of planned treatment
Exploratory objectives
-
To identify possible biomarkers of response to ICD
-
To estimate second progression-free survival (PFS2) measured from randomisation to second disease progression for those that switch to ICD treatment following CD treatment
-
To estimate progression-free survival from the point of switching to second disease progression (PFS Switch) for those that switch to ICD treatment following CD treatment
-
To evaluate the clinical activity of ICD with regard to additional exploratory endpoints, detailed in Table 3
-
To determine the safety and toxicity profile of ICD after progressing on CD treatment
Sample size
Using data from previous studies, median PFS in the CD arm is expected to be in the region of 4 to 6 months whilst median overall survival (OS) in the CD arm is expected to be around 8 months [8,9,10,11,12,13]. It is anticipated that the addition of ixazomib to CD (ICD), in RRMM patients who have relapsed after treatment with thalidomide, lenalidomide and a proteasome inhibitor, may improve clinical efficacy by at least 50%, in terms of median PFS. One formal interim efficacy analysis is planned for when 70% of the PFS events (139 events) have been observed, to assess for superiority of ICD.
For the final analysis, assuming median PFS of 6 months in the CD arm, a total of 198 PFS events are required to detect an improvement in median PFS to 9 months with the addition of ixazomib to CD, corresponding to a hazard ratio of 0.67 (80% power, 4.55% 2-sided significance level in order to maintain 5% significance overall when taking into account the interim analysis). A total of approximately 230 patients (115 patients per arm) will be needed for patient enrolment to generate a total of 198 PFS events (Fig. 3). This assumes recruitment over a 24-month period, with an additional minimum 12 months’ follow-up. Allowing for dropout of 8%, a total of 250 participants are required. With 250 patients generating more than a total of 198 PFS events, this will also provide sufficient power (> 80%) to detect an improvement of 50% in median PFS where the control arm median PFS is anywhere in the region of 4 to 6 months.
For the interim analysis, the O’Brien and Fleming [14] approach will be used in order to maintain an overall 5% 2-sided significance level when performing a single interim analysis before final analysis. Superiority at the interim analysis, in terms of PFS, will therefore be tested at a 0.0074 1-sided significance level, whilst the final analysis will be tested at a 0.0455 2-sided significance level.
At the interim analysis, assuming median PFS of 6 months in the CD arm, there will be approximately 47% power to detect a hazard ratio of 0.67. A low power has been used as an early release of data will only take place at this point if an overwhelming treatment effect is seen.
A total of 186 deaths, which are expected from the sample size of 250, provide over 80% power to detect an improvement in median overall survival (OS) from 8 months with CD to 11.5 months with ICD, corresponding to a hazard ratio of 0.7, at the 2-sided 10% significance level.
This ‘switch’ phase of the study is exploratory so no formal sample size calculation has been performed.
Recruitment process
When calculating the sample size, the trial was expected to take 24 months to complete recruitment, at a rate of 15 participants per month, and the first trial participant was randomised on 21 January 2016. However, due to slower recruitment than anticipated, it is likely the trial will take longer than this to complete recruitment. Participants will be recruited from NHS hospitals throughout the UK which are approved research sites within the MUK Early Phase CTN. A full list of study sites can be accessed via the trial registration, ISRCTN58227268.
Research sites will be required to have obtained ethical and management approval and undertake a site initiation meeting with Clinical Trials Research Unit (CTRU) prior to opening to recruitment. Potential participants will be approached by authorised members of staff, usually during standard clinic visits for management of their disease, who will verbally describe and discuss the trial and then provide the patient information sheet.
Participants will be given as long as they need to consider whether they wish to take part and will be able to discuss the study with their family, friends and other healthcare professionals if they wish. Consenting participants will be invited to provide informed, written consent and will be formally assessed for eligibility, according to the inclusion and exclusion criteria detailed in Table 1.
Randomisation
Written informed consent for entry into the trial must be obtained, with eligibility being confirmed prior to randomisation. Randomisation will be administered using an automated 24-h web-based system managed by the CTRU. A computer-generated minimisation programme that incorporates a random element will be used to balance treatment groups for age (< 60 vs. 60–69 vs. ≥ 70), number of prior lines of therapy (≤ 3 vs. > 3) and β2M (< 3.5 mg/L vs. 3.5 mg/L ≤ β2M < 5.5 mg/L vs. ≥ 5.5 mg/L) at randomisation.
Study centre has not been included as a minimisation factor as the primary endpoint is standardly assessed across all centres, as seen from previous trials run through CTRU; therefore, clustering within sites will not likely be an issue. Additionally, the impact of treatment groups not being balanced within a centre is thought to be less problematic than treatment group unbalance across the minimisation factors selected.
Intervention
Patients randomised to ICD will receive the following regimen: ixazomib (oral) 4 mg on days 1, 8 and 15; cyclophosphamide (oral) 500 mg on days 1, 8 and 15; and dexamethasone (oral) 40 mg on days 1–4 and 12–15.
Patients randomised to CD will receive the following regimen: cyclophosphamide (oral) 500 mg on days 1, 8 and 15 and dexamethasone (oral) 40 mg on days 1–4 and 12–15.
For older/less fit patients in both cohorts (as determined by the Principal Investigator), dexamethasone may be given orally at 20 mg on days 1–4 and 12–15.
In both cohorts, the cycle is repeated every 28 days with response being assessed at the end of each cycle. Before commencing, a new cycle of treatment the participant must meet the parameters set in the eligibility criteria (including laboratory results), given in Table 1. Participants will continue on the trial regimen until disease progression, death, unacceptable toxicity or withdrawal of consent, whichever is sooner.
Participants randomised to CD alone may switch to receive ICD, according to the same schedule above, once disease progression is confirmed both by two TMG clinical members and two consecutive assessments (as defined by the IMWG response criteria), and eligibility has been confirmed as detailed in Table 2.
If a participant’s cyclophosphamide and/or dexamethasone doses have been reduced during the CD only phase of the trial, they will remain at the same dose when moving on to ICD.
Trial assessments
Written informed consent must be obtained prior to the commencement of trial-specific assessments, and baseline assessments are to be performed within 14 days prior to randomisation. The required baseline assessments include a physical examination, ECOG performance status, medical history, ISS stage and ECG, as well as haematology, biochemistry and bone marrow sample tests. Participants must also complete the EQ-5D (5-level) and EORTC QLQ-C30 quality of life questionnaires prior to randomisation.
Assessments to be carried out within 48 h prior to the start of each cycle of treatment include a physical examination, peripheral neuropathy assessment, ECOG performance status, recording of adverse reactions and concomitant medications, and haematology and biochemistry tests. Participants will also complete the EQ-5D (5-level), EORTC QLQ-C30 and Resource Use questionnaires every 3 cycles. Laboratory results must be available and reviewed by the clinical team before dosing on day 1 of each cycle of treatment. Full blood counts will also be performed on days 8, 15 and 22 of cycles 1–3, and for the first 3 cycles of ICD following CD treatment. Blood samples for central investigations will be taken in cycle 4. Haematology and biochemistry results must remain within the parameters outlined in the eligibility criteria to proceed with each cycle of treatment.
End of treatment assessments, at the end of initial randomised treatment (CD or ICD) and at the end of the switch to ICD treatment, include a physical examination, peripheral neuropathy assessment, ECOG performance status, recording of adverse reactions and concomitant medications, and haematology, biochemistry and bone marrow tests. Participants will also complete the three quality of life questionnaires as before.
All participants will be followed up 4-weekly post the end of treatment until second disease progression. Follow-up will involve a response assessment and reporting of adverse reactions and SAEs will occur until 60 days post the last dose of trial treatment. Participants will be asked to complete the questionnaires at 3-month intervals until second disease progression. Participants who switch to ICD after treatment with CD will be followed up for 60 days post the end of treatment for toxicity (even if they stop treatment for (second) disease progression). After first disease progression, all participants will be followed up for a minimum of 12 months post-randomisation for survival only, until the time of final analysis.
Data collection, management and monitoring
Participants will be identified by hospital sites during haematology clinic visits, and consent forms will be collected and checked to ensure all participants are consented fully. All data collected will be anonymised with a participant trial ID and sent with date of birth and initials to ensure accurate identification of participants for data entry. Data entry will be performed from paper Case Report Forms (CRFs) completed by each hospital site by internal staff and stored on the secure trial database accessed only by authorised members of CTRU staff. EORTC EQ-5D and QLQ-C30 will be used to collect quality of life data, in accordance with the EORTC instructions provided, therefore deemed valid and reliable.
Data management processes are fully documented in a trial work instructions document. Data will be 100% data checked for all items relating to trial endpoints and safety, i.e. doses of treatment and adverse reactions, for data quality. For any participant reaching the end of the trial on the CD arm and switching to the ICD arm, laboratory reports will be collected to verify this.
Adverse reactions will be collected on the CRF and 100% checked and data managed in the hope that this will ensure the data is accurate. Serious adverse events and suspected unexpected serious adverse events will be collected in real time with all being reviewed by the Chief Investigator within 24 h to guard against harm coming to the patient. Bleeding events will be closely monitored for the first 5 patients receiving ixazomib due to concerns regarding a low platelet count at inclusion.
Statistical methods and analysis
For all statistical analyses, the analysis population (participants that are evaluable for the primary endpoints), as well as the safety population (participants that are evaluable for the toxicity and safety endpoints), are defined as those who receive at least one dose of any trial treatment. Toxicity and safety endpoints will be assessed according to the treatment actually received whilst effectiveness endpoints will be assessed by treatment the patient is randomised to. For example, patients on the ICD arm that do not receive ixazomib will be analysed together with the ICD patients that have received ixazomib.
Interim analysis
One formal interim efficacy analysis is planned for when 70% of the PFS events (139 events) have been observed, to assess for superiority of ICD in terms of PFS, and is estimated to take place at the same time as completing recruitment. This interim analysis is detailed in a Data Monitoring and Ethics Committee (DMEC) Interim Statistical Analysis Plan, and if, at the time of this interim analysis, ICD is found to be significantly superior when compared to CD, the DMEC may report to the Trial Steering Committee (TSC) with a recommendation of early release of data, rather than a recommendation of early trial closure. If the timing of this interim analysis falls before the end of recruitment, the DMEC may report to the TSC with a recommendation of early trial closure if appropriate.
Primary endpoint analysis
The primary endpoint analysis will compare the ICD arm to the CD arm in terms of PFS, with a null hypothesis of no difference between ICD and CD, and an alternative hypothesis of a difference between ICD and CD with ICD expected to be superior to CD. PFS curves will be calculated using the Kaplan-Meier method and the median PFS estimates and PFS estimates at 6 and 12 months with corresponding 95% confidence intervals will be presented by treatment group. A log-rank test, stratifying for the minimisation factors, will be used to compare PFS between the treatment groups.
The proportional hazards assumption will be assessed by plotting the hazards over time for each treatment arm, in addition to using the methods of Lin et al. [15] to check the adequacy of the Cox regression model. If the assumptions for Cox’s proportional hazards (Cox PH) model can be verified, a Cox PH model will be used. This model will adjust for the minimisation factors and other important prognostic factors identified by the TMG, in order to identify factors predictive of PFS between the treatment arms. Parameter estimates, standard errors, hazard ratios and 95% CIs, and p values will be presented for treatment and all other covariates included in the model.
Secondary endpoint analysis
For secondary endpoint analyses, maximum response is defined as the proportion of participants achieving each of the response categories sCR, CR, VGPR, PR, MR, SD or PD as their maximum response to initial treatment. Logistic regression adjusting for treatment group and minimisation factors will be used to predict the proportion of patients achieving at least a PR, and ordered logistic regression will be used to analyse the proportion of patients in each maximum response category, where appropriate (i.e. should the number of events in each maximum response level be sufficient).
The Kaplan-Meier method and log-rank test will be used to summarise the difference between treatment arms in terms of time to maximum response, duration of response and overall survival. If the Cox PH assumptions are confirmed as valid, a Cox PH model will also be fitted for these endpoints, in addition to the time to progression endpoint, provided no competing risk events have occurred. Residuals and predicted values produced from any multivariate models will be examined to assess the assumptions of the model. Competing risk analyses using cumulative incidence functions will be conducted for time to progression and time to maximum response endpoints. For these endpoints respectively, patients that have died with no previous evidence of disease progression and patients that have died prior to achieving a maximum response will be classed as having had a competing risk. Those not evaluable for maximum response (i.e. those with no response assessments following commencement of treatment) will be summarised as ‘no maximum response’ and excluded from analyses.
The cost-effectiveness analysis will consist of a decision model analysis informed by the trial data (patient reported resource use and the EQ-5D-5L) along with data from the wider literature and other sources where necessary. The primary analysis will be conducted from the healthcare provider perspective and report cost per quality-adjusted life year (QALY) gain over a lifetime horizon. Deterministic and stochastic sensitivity analyses will be performed. The analysis will be outlined in full in a health economics analysis plan ahead of analysis commencing.
Quality of life (QoL) will be summarised descriptively for each post-randomisation time-point using bar charts, box plots, plots of mean QoL over time and summary tables. Differences between treatment groups will also be obtained using a multi-level repeated measures model accounting for data at all post-baseline time points, assuming missing data at random (MAR). Missing data patterns will be examined, and sensitivity analyses using different missing data assumptions will be performed where appropriate, as described below.
A summary of the main comparisons and analysis methods for each secondary endpoint are given in Table 3.
Sensitivity analyses for PFS and OS will be performed using imputed dates if there are > 5% of participants with a completely missing date of death/progression. Sensitivity analyses will also be conducted if there are > 5% of partially missing dates, using the earliest and latest possible day of the month. Sensitivity analyses for QoL may be carried out using methods such as multiple imputation, pattern-mixture multi-level models categorising participants into strata based on clinical information which is believed to represent the reasons for missing data (assuming MAR data conditional upon participants’ clinical data), and pattern mixture models for bivariate (baseline and 9 week) data fitted using a variety of restrictions reflecting the missing data pattern ranging from complete case missing variable restriction (MAR) to Brown’s protective restriction (assuming data are missing not at random (MNAR)).
PFS and OS will also be analysed adjusting for baseline Charlson Comorbidity Index [16] score (0, 1–2, > 2), which is calculated by assigning scores to each participant’s age and any comorbidities they exhibit, then summing the total of these scores. By including the Charlson Comorbidity Index scores in the Cox’s proportional hazards model for PFS and OS, this will determine the prognostic value of baseline Charlson index score on these outcomes. An interaction between baseline Charlson index score and treatment will also be included in the Cox proportional hazards models to assess the impact of the baseline score on treatment’s effect on the outcome. Deliverability of planned treatment according to baseline Charlson index score will be assessed by summarising the treatment compliance and toxicity endpoints according to participants’ baseline score (0, 1–2, > 2).
Exploratory analyses to investigate biomarkers of response will also be performed. These analyses will be detailed in full in a separate statistical analysis plan prior to any analysis undertaken.
Further exploratory analyses, detailed in Table 3, will be conducted for the switch phase of the trial, where patients on the CD arm may receive ICD treatment after confirmed progression on CD. These will include PFS2, PFS Switch, treatment compliance, and safety and toxicity. The definitions of PFS, PFS2 and PFS Switch are visualised in Fig. 2.
Frequency of analyses
A DMEC (made up of at least two clinicians and one statistician that are independent of the study team) will be set up to review data on safety, activity, protocol adherence and recruitment. The DMEC will review safety data for all participants entered into the trial after 12 participants have been recruited, and 3-monthly thereafter. Interim reports containing safety data, protocol adherence and recruitment will be presented to the DMEC in strict confidence at, at least, yearly intervals. This committee, in light of the interim data, and any advice and evidence they wish to request, will if necessary report to the TSC if there are any concerns regarding the activity or safety of the trial treatments.
The DMEC may also report to the TSC, with a recommendation of early release of data, should ICD be found to be significantly superior to CD during the interim analysis (once 70% of PFS events have been observed).
Final analysis will take place in two stages. Analysis of the primary endpoint will take place when at least 198 PFS events have been observed. At this time, all other endpoints relating to the first ‘phase’ of the study, with the exception of OS, will be analysed. A decision will be made based on the overall number of deaths observed as to whether OS will be analysed at the same time as PFS, or whether additional follow-up is required prior to analysis. Analyses relating to the switch phase of the study will take place after a minimum of 6 months follow-up after the last CD participant to switch treatments has started ICD treatment.
Discussion
Despite advances in treatment options and improvements in survival rates over recent years, the overall prognosis for MM patients remains poor. Most patients will respond to initial treatment, potentially entering a plateau phase for a number of years, but relapse is inevitable. Subsequent response can be obtained by re-treating with the same or different regimens; however, some patients will become refractory to existing standard treatments. Ixazomib offers the opportunity to further investigate the value of proteasome inhibition in the treatment of RRMM whilst carrying the benefits of oral administration.
Two phase I studies have already investigated ixazomib in the RRMM setting [3, 5, 17]. These studies both incorporated a dose escalation phase followed by a dose expansion phase and indicated that ixazomib is well tolerated, with manageable toxicities. Dose limiting toxicities seen in these studies were skin rash, thrombocytopenia, nausea, diarrhoea, vomiting and erythema multiforme. Additionally a phase II study has investigated the safety and efficacy of ICD in patients with RRMM [18]. This study demonstrated a toxicity profile consistent with that seen in ixazomib in combination with lenalidomide and dexamethasone, whilst the combination appeared to have activity in RRMM patients. The promising clinical activity demonstrated in these studies, with durable responses and disease control, prove that further investigation of the anti-tumour effect of this drug in RRMM patients is warranted, especially given that no trials comparing CD with the combination of ixazomib and CD have been completed at present. As of today, there has been no evidence of impact on trial recruitment of ixazomib (Ninlarao) being available through the Cancer Drugs fund in England and SMC in Scotland. Ixazomib is not accessible in Northern Ireland. We therefore believe that demonstration of an improvement in PFS and overall survival for patients treated with ICD compared to CD would act as supporting evidence for the use of ixazomib in the UK.
Availability of data and materials
Not applicable—this is a protocol paper outlining the study being conducted.
Abbreviations
- ASCT:
-
Autologous stem cell transplant
- CD:
-
Cyclophosphamide and dexamethasone
- CR:
-
Complete response
- CTN:
-
Clinical Trials Network
- CTRU:
-
University of Leeds Clinical Trials Research Unit
- DMEC:
-
Data Monitoring and Ethics Committee
- ECG:
-
Electrocardiogram
- ECOG:
-
Eastern Cooperative Oncology Group
- EORTC:
-
European Organisation for Research and Treatment of Cancer
- EQ-5D:
-
EuroQol five-dimension scale
- QLQ-C30:
-
Quality of life questionnaire
- ICD:
-
Ixazomib, cyclophosphamide and dexamethasone
- IMWG:
-
International Myeloma Working Group
- ISS:
-
International Staging System
- MM:
-
Multiple myeloma
- MR:
-
Minimal response
- MUK:
-
Myeloma UK
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- PFS2:
-
Second progression-free survival measured from randomisation
- PFS Switch:
-
Progression-free survival measured from the point of switching to second progression
- PR:
-
Partial response
- RRMM:
-
Relapsed/refractory multiple myeloma
- sCR:
-
Stringent complete response
- SD:
-
Stable disease
- TMG:
-
Trial Management Group
- TSC:
-
Trial Steering Committee
- VGPR:
-
Very Good Partial Response
References
Cancer Research UK. Available from: http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/myeloma. Accessed 21 Feb 2018.
Kouroukis TC, et al. Bortezomib in multiple myeloma: systematic review and clinical considerations. Curr Oncol. 2014;21(4):e573–603.
Richardson PG, et al. Phase 1 study of twice-weekly ixazomib, an oral proteasome inhibitor, in relapsed/refractory multiple myeloma patients. Blood. 2014;124(7):1038–46.
Chauhan D, et al. In vitro and in vivo selective antitumor activity of a novel orally bioavailable proteasome inhibitor MLN9708 against multiple myeloma cells. Clin Cancer Res. 2011;17(16):5311–21.
Kumar SK, et al. Phase 1 study of weekly dosing with the investigational oral proteasome inhibitor ixazomib in relapsed/refractory multiple myeloma. Blood. 2014;124(7):1047–55.
Nooka AK, et al. Treatment options for relapsed and refractory multiple myeloma. Blood. 2015;125(20):3085–99.
Brown SR, et al. Experiences of establishing an academic early phase clinical trials unit. Clinical Trials. 2017;14(4):349–56.
Richardson PG, et al. Bortezomib or high-dose dexamethasone for relapsed multiple myeloma. N Engl J Med. 2005;352(24):2487–98.
Kortuem KM, Stewart AK. Carfilzomib. Blood. 2013;121(6):893–7.
Dimopoulos MA, et al. Pomalidomide in combination with low-dose dexamethasone: demonstrates a asignificant progression free survival and overall survival advantage, in Relapsed/Refractory MM: A Phase 3, Multicenter, Randomized, Open-Label Study. Blood. 2012;120(21):LBA-6.
Lacy MQ, et al. Pomalidomide plus low-dose dexamethasone in myeloma refractory to both bortezomib and lenalidomide: comparison of 2 dosing strategies in dual-refractory disease. Blood. 2011;118(11):2970–5.
Leleu X, et al. Pomalidomide plus low-dose dexamethasone is active and well tolerated in bortezomib and lenalidomide–refractory multiple myeloma: Intergroupe xrjrncophone du Myélome 2009-02. Blood. 2013;121(11):1968–75.
Damaj G, et al. Results from a prospective, open-label, phase II trial of Bendamustine in refractory or relapsed T-cell lymphomas: the BENTLY trial. J Clin Oncol. 2013;31(1):104–10.
O'Brien PC, Fleming TR. A multiple testing procedure for clinical trials. Biometrics. 1979;35(3):549–56.
Lin DY, Wei LJ, Ying Z. Checking the cox model with cumulative sums of martingale-based residuals. Biometrika. 1993;80(3):557–72.
Charlson ME, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83.
Moreau P. Oral therapy for multiple myeloma: ixazomib arriving soon. Blood. 2014;124(7):986–7.
Kumar S, et al. Phase 2 study of the all-Oral combination of Ixazomib plus cyclophosphamide and low-dose dexamethasone (ICd) in patients (Pts) with relapsed/refractory multiple myeloma (RRMM). Blood. 2016;128(22):3327.
Acknowledgements
The study drug, ixazomib, is provided by Millennium Pharmaceuticals, Inc., Cambridge, MA, USA, a wholly owned subsidiary of Takeda Pharmaceutical Company Limited, who also provide funding to Myeloma UK, who in turn fund the MUK eight study. Millennium Pharmaceuticals approved the design of the study but have no input in the collection, analysis or interpretation of data. Millennium Pharmaceuticals will receive manuscripts arising from the study publishing trial outcomes for review. Through the Myeloma UK Clinical Trials Network, Myeloma UK were involved in the study design and are actively involved in the collection and interpretation of data, as well as in the review of manuscripts arising from the study publishing trial outcomes.
Funding
The study is funded by Myeloma UK, who receive funding from Millennium Pharmaceuticals, Inc., Cambridge, MA, USA, a wholly owned subsidiary of Takeda Pharmaceutical Company Limited.
Author information
Authors and Affiliations
Consortia
Contributions
SH, DS, LF, BD, DM, HWA, MC, SB and GC designed the study and wrote the protocol. KW, SH and SB developed the statistical analysis plan. HWA, MC and GC perform the research and collect data. DS, LB, SR, LF, SM and FBS perform trial and data management. BD and DM developed the health economics analysis plan. MFK and GC co-ordinate sample biobanking. SH, KW, LB and SB wrote the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The trial has received national research ethics approval from the NHS National Research Ethics Service North West, Liverpool East (REC Number: 15/NW/0416). All patients provide written informed consent prior to randomisation in to the trial.
Consent for publication
Not applicable.
Competing interests
SH, KW, DS, LB, SR, LF, SM, FBS, BD, DM and SB declare they have no competing interests. HWA declares research support from Amgen, consultancy fees and honoraria from Amgen, Takeda, and Novartis, and Karyopharm. MFK has served as a consultant and received honoraria from Celgene, Takeda, Amgen, Chugai, BMS, and Janssen, and has received research funding from Celgene. MC declares honoraria and travel fees from Janssen, Celgene, Takeda, Amgen and Chugai and has received research support from Celgene, CRUK and Janssen. GC has served as a consultant and speaker for Takeda, Amgen, Janssen and Seattle Genetics and has received research funding from Takeda and Celgene. The trial is sponsored by the University of Leeds (contact details accessible via the trial registration, ISRCTN58227268).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hinsley, S., Walker, K., Sherratt, D. et al. The MUK eight protocol: a randomised phase II trial of cyclophosphamide and dexamethasone in combination with ixazomib, in relapsed or refractory multiple myeloma (RRMM) patients who have relapsed after treatment with thalidomide, lenalidomide and a proteasome inhibitor. Trials 21, 826 (2020). https://doi.org/10.1186/s13063-020-04739-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-020-04739-8