Abstract
Background
An effective drug to treat cryptosporidial diarrhea in HIV-infected individuals is a global health priority. Promising drugs need to be evaluated in endemic areas which may be challenged by both lack of resources and experience to conduct International Committee of Harmonisation-Good Clinical Practice (ICH-GCP)-compliant clinical trials.
Methods
We present the challenges and lessons learned in implementing a phase 2A, randomized, double-blind, placebo-controlled trial of clofazimine, in treatment of cryptosporidiosis among HIV-infected adults at a single site in Malawi.
Results
Primary challenges are grouped under study initiation, study population, study implementation, and cultural issues. The lessons learned primarily deal with regulatory system and operational barriers, and recommendations can be applied to other human experimental trials in low- and middle-income countries, specifically in sub-Saharan Africa.
Conclusion
This study demonstrated that initiating and implementing human experimental trials in sub-Saharan Africa can be challenging. However, solutions exist and successful execution requires careful planning, ongoing evaluation, responsiveness to new developments, and oversight of all trial operations.
Similar content being viewed by others
Background
Clinical trials, particularly human experimental trials, are critical to learning the safety and efficacy of drugs and therefore to treating diseases [1, 2]. Trials are especially needed to address the high burden of disease in low- and middle-income countries (LMICs), specifically in sub-Saharan Africa. For as much as 50% of the global burden of disease, mostly due to infections, reside in sub-Saharan Africa [3].
Clinical trials testing drugs and vaccines that target specific diseases afflicting people in sub-Saharan Africa are logically best run in those countries. These trials can benefit from local healthcare knowledge and are better able to address context-specific questions that would then lead to more effective interventions [4]. Clinical research conducted in LMICs, particularly sub-Saharan Africa, build both research and health care capacity [4], which has been shown to strengthen health systems, expand health programming, and provide an evidence base for future health crises responses [5]. Major operational benefits of conducting trials in sub-Saharan Africa include the ease of recruiting trial participants and the availability of health workers with clinical research experience [4].
Despite these facts, only 20–30% of global clinical trials are conducted in LMICs and less than 10% in sub-Saharan Africa (Fig. 1) [1]. Several barriers to conducting research in sub-Saharan Africa contribute to this situation. These barriers include financial and human capacity, delays in regulatory and ethical reviews, complex logistical and financial systems, and competing demands [4].
Distribution of clinical studies registered on ClinicalTrials.gov on April 2019 [6]
In the developing world, Cryptosporidium infection and the associated diarrheal disease (cryptosporidiosis) is life-threatening in persons with HIV infection and in children younger than 5 years [7]. Currently, nitazoxanide is the only licensed drug for the treatment of cryptosporidiosis in immunocompetent persons after the first year of life [8].
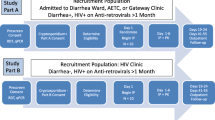
The first human experimental trial to evaluate the therapeutic clofazimine (CFZ) for treatment of cryptosporidiosis was conducted in Malawi, a low-income country with limited experience conducting clinical trials and with even less experience conducting human experimental trials. This study was classified as a phase 2a trial evaluating the safety, tolerability, pharmacokinetics (PK), and efficacy of CFZ in cryptosporidiosis (Cryptofaz). It was a two-part study (A and B) that took place at Queen Elizabeth Central Hospital (QECH) in Blantyre, Malawi [9]. Part A was a randomized, placebo-controlled, double-blind clinical trial with a 1:1 ratio of intervention to control. Part B was an open-label study, comparing the PK of orally administered CFZ in HIV-infected individuals with and without Cryptosporidium diarrhea. Further details on the study protocol can be found elsewhere [9]. Recruitment began in December 2017 and was completed in January 2019.
Similar to the experience of other clinical trials conducted in sub-Saharan Africa, the Cryptofaz team encountered several logistical, operational, and implementation challenges [9]. Addressing these challenges effectively was key to conducting this clinical trial [10]. This article reports on the lessons learned. These lessons can be useful to other human experimental trials being considered or conducted in sub-Saharan African settings.
Challenges
Topic areas are presented according to when they occurred during the clinical study. The challenges, lessons learned, and recommendations are listed in full in Table 1.
Study initiation
Contracts and regulatory approvals
Agreements between key international institutions took more time (several months when there was a need to accomplish this within several weeks) than anticipated. Similar to the experience of other clinical trials being conducted in developing countries, obtaining ethics and regulatory approvals in Malawi required significant time and effort from study staff [4].
Trial insurance
In order to get the required trial insurance in Malawi, the sponsor and local site had to contract with four insurance companies. We were required to work through an institutionally sanctioned insurance broker and this created complications. The multiple layers of bureaucracy involved in getting the policy approved increased the time to trial commencement.
Staffing
Hiring expert clinical trial personnel was a lengthy process. Identifying seasoned candidates with clinical trial experience is especially challenging in a less-developed setting. Local populations generally have limited experience conducting clinical trials—though this is increasing.
Study population
The study population involved HIV-infected adults with three or more days of diarrhea who met all the inclusion and none of the exclusion criteria [10].
Slow enrollment
Initial enrollment projections (66 subjects enrolled in 9 months) were based on a preliminary study previously conducted in Blantyre, Malawi, where a rapid diagnostic test was used on patients hospitalized with diarrhea over a 3-month period to obtain rough estimates of the prevalence of Cryptosporidium in the hospitalized population (17%). The preliminary study captured information on HIV status and clinical stage, diarrhea duration, and age, but not information on the laboratory and clinical exclusion criteria, such as electrolyte abnormalities or tuberculosis testing. Unfortunately, the actual enrollment rate for the Cryptofaz study (15 subjects in the first 10 months) did not match the projections.
There are several factors that accounted for the slow enrollment. Initial recruitment was based on a diarrhea duration of > 14 days, and it was difficult to find subjects with this diarrhea duration who were also Cryptosporidium positive by PCR. Therefore, the study team modified the inclusion criteria in an effort to increase enrollment. The required diarrhea duration was shortened as well as the duration an individual could be on antiretroviral therapy (ART). In addition, outreach was expanded to include referrals from health clinics in the surrounding urban Blantyre area. Furthermore, an unusually dry season during the recruitment period appeared to play a role in the low infection rate in the Blantyre population.
However, even with these study modifications, the enrollment rate did not increase to the anticipated level. Ultimately, the study team determined that this enrollment rate was too slow to be feasible, and the study was stopped due to an insufficient recruitment rate after enrolling 20 subjects in part A of the trial (instead of the anticipated 56 subjects). Correspondingly, the interim analysis, planned at 20 subjects, became the final analysis.
Health status
The design of Cryptofaz was based on a pilot study that did not include information on the health status of potential subjects. Therefore, we were not aware of potential laboratory abnormalities and occult disease until screening. The study identified multiple potential subjects who were failing their antiretroviral treatment (ART) despite being on treatment for months or years. Related to the low CD4 counts, many subjects were found to have undiagnosed TB. Also, many potential subjects were found to be severely hypokalemic because of their diarrhea and had to receive potassium supplementation prior to enrollment. The study provided care and close clinical follow-up to these subjects.
High mortality rate
In this resource-limited setting, the team found that many subjects who fit the inclusion and exclusion criteria were extremely ill and some did not survive the study period. Hence, the mortality rate (20%) was slightly higher than initially estimated (15%). With the addition of LAM TB screening, enrollment was affected (decreased) as more cases of undiagnosed TB were detected and the mortality rate also decreased.
Study implementation
Lab equipment
The study required acquisition and installation of critical lab equipment. Most of this equipment had to be procured from outside Malawi. Therefore, lengthy shipping times had to be worked into the study timeframe.
Lab testing
Commonly, sites new to clinical research will require new skill sets. Cryptofaz was a technically complex study with multiple new laboratory tests and procedures. For example, examination for reliability of qPCR data was a new procedure for the study team, and the team required ongoing review, feedback, and troubleshooting support from one of the study’s partner institutions.
Randomization timing
The original protocol required randomization to occur simultaneously with study investigational product, preparation, and dispensation. This required both the pharmacist and data manager to be available nights and weekends, times outside of these staff normal working hours. Therefore, staffing schedules were modified to accommodate any potential out-of-hours study-related work needed.
Protocol amendments
Cryptofaz was an experimental study that had not been performed before. Thus, the characteristics of the potential participants and the enrollment rate were unknown. For these reasons, the trial required four protocol amendments to optimize the clinical trial recruitment, enrollment, and completion.
Data collection forms and data entry
While the clinical team reviewed each data collection form (DCF) and a data entry plan was developed before study implementation, ensuring an accurate data entry process required substantial effort and subsequent cleaning up of the data after entry.
Physical space
The study required dedicated space for inpatient treatment as well as for administration of the study. At the time of study initiation, QECH did not have available space to dedicate to the study.
Site Internet connectivity
The study relied on an electronic data system whereby data was to be transferred to the Contract Research Organization (CRO) in a timely manner for oversight and monitoring. The local site Internet was unreliable, and this slowed down training and data entry.
Cultural issues
Blood draws
Cryptofaz required blood draws for the PK studies. In Malawi, as in many sub-Saharan African countries, collecting blood comes with challenges. This relates to the conception of blood as a “life force” (thus strength is drained by losing blood) and to rumors of “blood suckers” (vampires) who come at night and suck people’s blood, thereby removing power and fertility from the person [11].
A few months before the study was to begin, groups of people in and near Blantyre attacked several persons (including health care workers) that were accused of being “blood suckers.” During study implementation, these fears threatened to interfere with the study. During a regular blood draw of a subject, her guardian became agitated about the number of tubes and accused the clinician of being a “blood sucker.” Others in the ward joined in with the accusations. Extensive sensitization and counseling of both ward staff and guardians were required to improve expectations of study procedures.
Food supplement palatability
The Cryptofaz study required nutritional consistency, both in terms of content and timing of meals. However, as nutritional consistency and quality of meals provided by QECH or guardians could not be ensured, the study team identified “Plumpy’Nut” [12] and “Plumpy’Soy” [13] as alternative appropriate food supplements and found a local source for these products. Some subjects found the supplement to be unpalatable, and therefore, the team had to identify ways to make the taste more acceptable.
Conclusion
The Malawian Cryptofaz study is an example of a successful human experimental trial conducted in a low-income country. Barriers to the conduct of clinical trials in developing countries have been systematically reviewed and fall under five unifying themes: lack of financial and human capacity, ethical and regulatory system obstacles, lack of research environment, operational barriers, and competing demands [2]. However, few of the clinical trials listed in the reviews were from Africa and even fewer from the “least developed” countries as designated by the Development Assistance Committee (DAC) [14].
Sub-Saharan African countries face enormous challenges in conducting high-quality clinical trials. However, in the case of the Cryptofaz trial in Malawi, the study team encountered challenges, particularly in the area of regulatory system and operational barriers, but were able to overcome most. As a result, the capacity at the investigational site for conducting clinical trials was built and/or strengthened. This was particularly true in relation to the site’s capabilities in clinical services, data management, pharmacy, study coordination, governance, and human resources. The challenges, lessons, and recommendations from Cryptofaz are specific to the study’s context, but may prove useful to other human experimental trials in sub-Saharan Africa.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Singh N. Benefits of conducting clinical trials in developing countries like India. Pharmaceutical Regulatory Affairs. 2018;7(2):1–2.
Alemayehu C, Mitchell G, Nikles J. Barriers for conducting clinical trials in developing countries- a systematic review. Int J Equity Health. 2018;17(1):37.
Michaud C. Global burden of infectious diseases. Encycl Microbiol. 2009:444–54. https://doi.org/10.1016/B978-012373944-5.00185-1.
Franzen SR, Chandler C, Enquselassie F, Siribaddana S, Atashili J, Angus B, Lang T. Understanding the investigators: a qualitative study investigating the barriers and enablers to the implementation of local investigator-initiated clinical trials in Ethiopia. BMJ Open. 2013;3(11):e003616.
Kelaher M, Ng L, Knight K, Rahadi A. Equity in global health research in the new millennium: trends in first-authorship for randomized controlled trials among low- and middle-income country researchers 1990-2013. Int J Epidemiol. 2016;45(6):2174–83.
Studies on Map-Clinical Trials.gov [https://www.clinicaltrials.gov/ct2/search/map]. Accessed 30 Apr 2019.
Khalil IA, Troeger C, Rao PC, Blacker BF, Brown A, Brewer TG, Colombara DV, De Hostos EL, Engmann C, Guerrant RL, et al. Morbidity, mortality, and long-term consequences associated with diarrhoea from Cryptosporidium infection in children younger than 5 years: a meta-analyses study. Lancet Glob Health. 2018;6(7):e758–68.
Love MS, Beasley FC, Jumani RS, Wright TM, Chatterjee AK, Huston CD, Schultz PG, McNamara CW. A high-throughput phenotypic screen identifies clofazimine as a potential treatment for cryptosporidiosis. PLoS Negl Trop Dis. 2017;11(2):e0005373.
Nachipo P, Hermann D, Quinnan G, Gordon MA, Van Voorhis WC, Iroh Tam PY. Evaluating the safety, tolerability, pharmacokinetics and efficacy of clofazimine in cryptosporidiosis (CRYPTOFAZ): study protocol for a randomized controlled trial. Trials. 2018;19(1):456.
Iroh Tam PY, Arnold SLM, Barrett LK, Chen CR, Conrad TM, Douglas E, Gordon MA, Hebert D, Henrion M, Hermann D, et al. Clofazimine for treatment of cryptosporidiosis in HIV-infected adults (CRYPTOFAZ): an experimental medicine, randomized, double-blind, placebo-controlled phase 2a trial. Clin Infect Dis. 2020:ciaa421. https://doi.org/10.1093/cid/ciaa421. Online ahead of print.PMID: 32277809.
Peeters Grietens K, Ribera JM, Erhart A, Hoibak S, Ravinetto RM, Gryseels C, Dierickx S, O'Neill S, Muela SH, D'Alessandro U. Doctors and vampires in sub-Saharan Africa: ethical challenges in clinical trial research. Am J Trop Med Hyg. 2014;91(2):213–5.
Nutriset Plumpy’Nut ready-to-use therapeutic food (RUTF). [https://www.nutriset.fr/products/en/plumpy-nut]. Accessed 30 Apr 2019.
Nutriset Plumpy’Soy ready-to-use supplementary food (RUSF) – lipid-based nutrient supplement (LNS) [https://www.nutriset.fr/products/en/plumpy-soy]. Accessed 30 Apr 2019.
DAC list of ODA recipients. [http://www.oecd.org/dac/financing-sustainable-development/development-finance-standards/daclist.htm]. Accessed 30 Apr 2019.
Acknowledgements
We thank the Cryptofaz team members for their hard work on the study (SLM Arnold, CR Chen, TM Conrad, MA Gordon, D Hebert, M Henrion, D Hermann, B Hollingsworth, E Houpt, KC Jere, MS Love, CW McNamara, J Nyirenda, DJ Operario, A Winter). MLW conducted the study in conjunction with several partners, including the University of Washington (sponsor), Emmes (Contract Research Organization), University of Virginia, Q2 Solutions, TechLabs, Calibr, Liverpool School of Tropical Medicine, and Novartis.
Funding
This experimental medicine trial was funded by the Bill and Melinda Gates Foundation (OPP1172544).
Author information
Authors and Affiliations
Contributions
NT and ED researched the data and wrote the first draft, with substantial contributions from MG, LKB, WVV, and PI. All authors were involved in the conduct of the clinical trial, and all authors reviewed the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This manuscript does not directly contain human data; however, its topic is a clinical trial in which all patients were appropriately consented and ethics approval was granted from the NHSRC (reference 17/05/1821) and by the Liverpool School of Tropical Medicine Research Ethics Committee (reference 17-031).
Consent for publication
There was no specific informed consent sought for this publication because it does not contain any patient data. However, as part of the Cryptofaz clinical trial, full informed consent was obtained before any patient started the study.
Competing interests
PI and WVV have received grants from Bill & Melinda Gates Foundation (BMGF) outside of the submitted work. WVV has patents issued for bumped kinase inhibitors (BKIs) for the therapeutic treatment of cryptosporidiosis diarrhea and is a founder and has stock of ParaTheraTech LLC, a company that is developing BKIs for animal health indications. All other authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Toto, N., Douglas, E., Gmeiner, M. et al. Conducting clinical trials in sub-Saharan Africa: challenges and lessons learned from the Malawi Cryptosporidium study. Trials 21, 680 (2020). https://doi.org/10.1186/s13063-020-04620-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13063-020-04620-8