Abstract
Background
Case–control studies show that mammographic density is a better risk factor when defined at higher than conventional pixel-brightness thresholds. We asked if this applied to interval and/or screen-detected cancers.
Method
We conducted a nested case–control study within the prospective Melbourne Collaborative Cohort Study including 168 women with interval and 422 with screen-detected breast cancers, and 498 and 1197 matched controls, respectively. We measured absolute and percent mammographic density using the Cumulus software at the conventional threshold (Cumulus) and two increasingly higher thresholds (Altocumulus and Cirrocumulus, respectively). Measures were transformed and adjusted for age and body mass index (BMI). Using conditional logistic regression and adjusting for BMI by age at mammogram, we estimated risk discrimination by the odds ratio per adjusted standard deviation (OPERA), calculated the area under the receiver operating characteristic curve (AUC) and compared nested models using the likelihood ratio criterion and models with the same number of parameters using the difference in Bayesian information criterion (ΔBIC).
Results
For interval cancer, there was very strong evidence that the association was best predicted by Cumulus as a percentage (OPERA = 2.33 (95% confidence interval (CI) 1.85–2.92); all ΔBIC > 14), and the association with BMI was independent of age at mammogram. After adjusting for percent Cumulus, no other measure was associated with risk (all P > 0.1). For screen-detected cancer, however, the associations were strongest for the absolute and percent Cirrocumulus measures (all ΔBIC > 6), and after adjusting for Cirrocumulus, no other measure was associated with risk (all P > 0.07).
Conclusion
The amount of brighter areas is the best mammogram-based measure of screen-detected breast cancer risk, while the percentage of the breast covered by white or bright areas is the best mammogram-based measure of interval breast cancer risk, irrespective of BMI. Therefore, there are different features of mammographic images that give clinically important information about different outcomes.
Similar content being viewed by others
Background
Mammographic images can be used for more than identifying existing breast tumours – they contain information that predicts both (1) the risk of future breast cancers and (2) the likelihood of existing tumours being missed due to masking [1]. This has important implications for future breast cancer control because of the widespread use of mammography screening. Women could be triaged according to their risk of disease and/or masking so as to implement tailored screening, and deal with the ongoing need to improve cost-effectiveness, minimise harm [2, 3], and help address the issue of “dense breasts” [4].
Conventionally, mammographic density has been defined as the white or bright areas on a mammogram and, after adjusting for age and body mass index (BMI), has been found to be a risk factor for both interval and screen-detected breast cancers [1, 5, 6]. Screen-detected breast cancers are cancers detected via a screening programme and interval breast cancers are those detected within 2 years of a mammographic screen that did not detect any breast cancer. Interval cancers are in general more aggressive [6,7,8,9,10,11], so it is important to understand if the relationship between mammographic density measures and breast cancer risk differs by mode of detection [12].
We previously found, from case-control studies of both Australian [13] and Korean [14, 15] women, that by defining mammographic density at higher than conventional pixel-brightness thresholds we obtained better discrimination between women with and without breast cancer. This applied for both film and digital mammograms. It is not known, however, if this observation differs according to mode of detection. In this study, we have used a prospective cohort and asked if, and how well, the conventional and our new mammographic density measures apply to interval and screen-detected breast cancers.
Materials and methods
Subjects
We used the prospective Melbourne Collaborative Cohort Study of Australian-born, Italian-born, and Greek-born male and female adult residents of Melbourne [16, 17]. We conducted a nested case–control study in which cases were women who had been diagnosed with a first diagnosis of ductal carcinoma in situ or invasive adenocarcinoma of the breast (C50.0-C50.9) since the baseline survey. Cases were ascertained by record linkage to the population-complete Victorian Cancer Registry and to the Australian Cancer Database. Controls had been matched for year at birth, year of baseline interview, and country of origin [12, 18]. Controls were selected randomly from those who had not been diagnosed with breast cancer at the age of diagnosis of the case. Participants completed interviewer-administered questionnaires that captured standard risk factors for breast cancer, including reproductive history. Height and weight were measured directly according to standard protocols and BMI was calculated from these. We studied only those female cohort members who had attended BreastScreen Victoria (the state-organised, free, 2-yearly, mammographic screening service for women aged 50 to 69 years) at least once for a mammogram, and did not have a diagnosis of breast cancer when they completed their baseline questionnaire. Family history of breast cancer in any blood relative, as collected by BreastScreen Victoria, was available for all participants.
Breast cancers were identified by BreastScreen Victoria, or by linkage with the Victorian Cancer Registry. Breast cancers diagnosed outside the screening service before the next scheduled scan (2 years) after a negative scan were classified as interval cancers, and those subsequently identified by BreastScreen Victoria at a scheduled scan were classified as screen-detected. Consequently, the study included two subgroups: 422 women with screen-detected breast cancers (357 of which were invasive) with 1197 matched controls and 168 women with interval breast cancers (148 of which were invasive) with 498 matched controls. For this study, we selected the mammogram closest to baseline (average 2 years difference [18]), and this was on average 5 or 6 years prior to diagnosis for interval and screen-detected cases, respectively; see Table 1 in a previous publication [12]. The study was approved by the human research ethics committees of the University of Melbourne and the Cancer Council Victoria.
Measurement of mammographic density
The cases’ contralateral mammograms that had been taken at or before diagnosis were used for analysis. All mammograms were screen-film and were digitised by the Australian Mammographic Density Research Facility using an Array 2905 Laser Film Digitizer at 12-bit depth.
The Cumulus computer-assisted thresholding method was used to measure mammographic density [19]. Five of the authors (TLN, YKA, SL, CFE, and NHT) independently measured mammographic density blinded to case-control status, mode of detection, and any other density measures already performed on the mammogram. Mammographic density was measured using the conventional definition of the white or bright areas, and we call these measures Cumulus. Mammographic density was further defined as the bright or brighter areas, in effect at higher pixel-brightness thresholds, and we call these measures Altocumulus and Cirrocumulus, respectively. These measurements have been described in our previous publications [13,14,15]. As when using the programme Cumulus, the measurer moves a toggle to select two thresholds (grey-level values). The first threshold distinguishes the breast from the background and the programme calculates the total area of the breast. The second threshold, known as the pixel density threshold, is based on what the measurer considers to be the dense tissue and the programme calculates the absolute dense area. This is done separately for the three density measures, each according to their different definitions of density, given above.
Figure 1 shows, for a particular section of the same mammogram, how the dense areas (outlined in green) vary depending on the definition of mammographic density. The left panel shows the region classified as Cumulus, and the centre panel shows that within this region there are brighter areas that are classified as Altocumulus. Similarly, within the latter regions, the right panel shows that there are even brighter areas that are classified as Cirrocumulus.
For each definition of mammographic density, we used the average over all measurers of their transformed, age-adjusted, BMI-adjusted and standardised measures so as to maximise the accuracy; see “Statistical methods”. Correlation between the resulting dense area and percent density measures was 0.87, 0.92, and 0.96 for Cumulus, Altocumulus, and Cirrocumulus, respectively. Correlation between the Cumulus and Altocumulus measures was 0.86 for dense area and 0.88 for percent density. The corresponding correlation between the Cumulus and Cirrocumulus measures was 0.82 and 0.82, respectively, and the corresponding correlation between the Altocumulus and Cirrocumulus measures was 0.82 and 0.82, respectively.
Repeatability was assessed by performing the measurements in 18 sets of 100 mammograms with the same ratio of cases and controls and including 10% repeat samples randomly in each set, to estimate intra-class correlation within the set. In the 5th, 10th, and 15th sets, there was also a 10% repeat sample from the first batch to estimate intra-class correlation between the sets. Consequently, 110 images were included in all batches except for batches 5, 10, and 15, which had 120 images.
For dense area, the within-set repeatability was 0.95 (95% confidence interval 0.94–0.96), 0.96 (0.94–0.97) and 0.94 (0.90–0.94) for the average of Cumulus, Altocumulus, and Cirrocumulus, respectively. For dense area, the between-set repeatability was 0.95 (0.93–0.97), 0.95 (0.94–0.96) and 0.94 (0.92–0.94) for the average of Cumulus, Altocumulus, and Cirrocumulus, respectively. Similar repeatability was obtained for the percent density measures. The average of the inter-observer correlation was 0.90, 0.92, and 0.87 for Cumulus, Altocumulus, and Cirrocumulus, respectively.
Statistical methods
Unconditional logistic regression was used to test for differences between independent sub-groups of cases defined by mode of detection. Conditional logistic regression was used to test for differences between cases and matched controls, and to estimate odds ratios between the mammographic density measures and breast cancer risk, separately for screen-detected breast cancer and interval breast cancer, adjusting for covariates. Given the change in direction of association between BMI and breast cancer risk with increasing age, we included an interaction term to test if the odds ratio for BMI in relation to breast cancer risk depended on age at mammogram. Each mammographic density measure was transformed using a Box–Cox power transformation to have an approximately normal distribution by using maximum likelihood to estimate the parameter λ such that (Yλ – 1)/λ is closest to a normal distribution [20]. For each fitted model, the mean of the transformed measures for the controls was adjusted for age and BMI to derive the residuals, from which their standard deviation was calculated.
As in our previous publications [13,14,15], we used this adjusted standard deviation and conditional logistic regression to estimate the odds ratio per adjusted standard deviation (OPERA, [21]). OPERA is a measure of the ability of a risk factor (appropriately adjusted for the covariates taken into account by design and analysis) to discriminate between cases and controls. When we fitted two standardised density measures, X1 and X2, into the same model, we presented the risk estimates in terms of their standard deviation (SD) after adjusting also for the other measure; see (14). We did this by multiplying the log(OR) estimate from fitting Xj by SD = [(1 – r2)]0.5, where r is the correlation between X1 and X2, and then exponentiated it to obtain the appropriate OPERA. The inter-quartile risk ratio (IQQR) corresponding to a given OPERA is approximately OPERA2.5. We also used the area under the receiver operator curve (AUC) to measure the discriminatory ability of measures. All statistical analyses were conducted using the software Stata [22], and following convention, P < 0.05 was considered to be statistically significant.
Parameter estimates were derived under asymptotic maximum likelihood theory. We compared the fits of nested models using the likelihood ratio criteria; under the null hypothesis, twice the absolute difference in the (maximum) log likelihood (ΔLL) has an approximately χ2 distribution with degrees of freedom equal to the difference in number of parameters. The fits of models were also compared based on the differences in the Bayesian information criterion (ΔBIC), which for models with the same number of parameters is 2ΔLL. If ΔBIC is the BIC of model A minus the BIC score of model B, then exp (-ΔBIC) is approximately equal to the posterior odds in favor of model A; for example, ΔBIC = − 6 or − 14 means that model A is roughly 400 or 1,000,000 times, respectively, more likely to be the model that generated the data than model B. The strengths of evidence against the model with the poorest fit are conventionally interpreted as non-existent if < 2, positive if 2–6, strong if 6–10, and very strong if ≥ 10 [23].
Results
Table 1 shows that women with interval breast cancer did not differ from their matched controls in any baseline characteristic, including BMI, except for family history (P ≤ 0.001). Screen-detected cases differed from their matched controls in family history (P < 0.001) and BMI (P = 0.003).
Table 2 shows that the unadjusted Cumulus, Altocumulus and Cirrocumulus measures of dense area were all greater for cases than for controls, for both interval and screen-detected breast cancer (all P < 0.01). Percent dense area measured by Cumulus, Altocumulus and Cirrocumulus was greater for cases with interval breast cancers compared with (1) their controls (all P < 0.001), and (2) cases with screen-detected breast cancers (all P < 0.001).
For interval cancer, the association with BMI did not depend on age at mammogram (P > 0.8). There was no association with BMI overall (see Table 1). Screen-detected cancer was associated with BMI and the association became stronger with age at mammogram (P < 0.02).
Table 3 shows that, for interval breast cancer, after adjusting for age and BMI all of the dense area measures were associated with breast cancer risk (all P < 0.001). The log (OPERA) was 0.61, 0.50 and 0.61 for Cumulus, Altocumulus and Cirrocumulus, respectively (all P < 0.001), There was very strong evidence that the Cumulus and Cirrocumulus measures gave a better fit than the Altocumulus measure (both ΔBIC ≥ 10).
For percent density measures, there was very strong evidence that the OPERA estimates were all higher than for their corresponding absolute density measure (all ΔBIC ≥ 10), especially for Cumulus where log (OPERA) was 0.85 compared with 0.65 and 0.72 for Altocumulus and Cirrocumulus, respectively (all P < 0.001). and that the Cumulus measure gave a better fit than the Cirrocumulus and Altocumulus measures (both ΔBIC ≥ 10). The risk gradient for Cirrocumulus was 30% and 17% higher than for the other two measures, respectively. Furthermore, there was very strong evidence that the Cumulus percent density measure gave a better fit than the Cumulus absolute density measure (ΔBIC = 28), with an estimated risk gradient 39% higher. Univariately, therefore, the Cumulus percent density measure gave a better fit for interval cancers, with an estimated risk gradient equivalent to an IQQR ~ 8-fold (95% CI 5–15).
Table 4 shows that, for screen-detected breast cancer, all the dense area measures were associated with risk, after adjusting for age and BMI as an interaction due to the aforementioned findings (paragraph 3, “Results”) (P < 0.001). The log OPERA was 0.22, 0.22 and 0.28 for the transformed, normalized and standardized Cumulus, Altocumulus and Cirrocumulus measures, respectively (all P < 0.001). There was strong evidence that the Cirrocumulus measure gave a better fit than the Cumulus and Altocumulus measures (ΔBIC = 8). On the log odds scale, the risk gradient for Cirrocumulus was 24% higher than for the other two measures. Results were similar for the percent density measures adjusted for age and BMI.
Table 5 shows that, for interval breast cancer, once we adjusted for Cumulus as a percentage, using the likelihood ratio test and comparing with the log likelihood of 192.48 from Table 3 showed there was no evidence that adding one or both of the other measures improved the fit (all P > 0.1). For example, when fitted together the OPERAs for the Cumulus attenuated but remained significant (P < 0.001) whereas the Altocumulus and Cirrocumulus estimates were reduced substantially and were no longer significant (all P > 0.07). In particular, adding the Cirrocumulus measure made no improvement to the fit (ΔLL = 0.7).
On the other hand, Table 5 shows that for screen-detected breast cancer it was Cirrocumulus that was a significant predictor (all P < 0.01) irrespective of which other measure(s) were in the model, and for both dense area and percent dense area measures. After adjusting for Cirrocumulus, using the likelihood ratio test and comparing with the log likelihoods of − 538.21 and − 536.75 from Table 4, respectively, showed no evidence that adding the other measures improved the fit (all ΔLL < 0.1). In particular, the Cumulus measures no longer predicted risk in all multivariable models; their OPERAs were close to 1.0 and not significant whether considered as percent or absolute dense area.
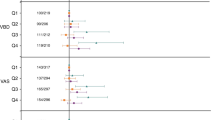
Figures 2 and 3 illustrate the relative stability of the risk measures by plotting the OPERAs and their confidence intervals as reported in Table 3, 4 and 5, on the log scale. For the percentage measures and interval cancers, the Cumulus measure dominates (see Fig. 2), while for dense measures and interval cancers the Cirrocumulus measure dominates (see Fig. 3). The patterns in estimates across the models are seen to be clearly different for the two outcomes.
Log odds ratio per adjusted standard deviation (Log OPERA) estimates, 95% confidence intervals (CI) and goodness-of-fit relative to the null model, given by twice the absolute change in log likelihood (2ΔLL) for the univariable, bivariable and trivariable model fits presented in Tables 3 and 5, for interval breast cancer and percent density measures of Cumulus, Altocumulus and Cirrocumulus
Log odds ratio per adjusted standard deviation (Log OPERA) estimates, 95% confidence intervals (CI) and goodness-of-fit relative to the null model, given by twice the absolute change in log likelihood (2ΔLL) for the univariable, bivariable and trivariable model fits presented in Tables 4 and 5 , for screen-detected breast cancer and density measures of Cumulus, Altocumulus and Cirrocumulus
Additional file 1: Tables S1 and S2 show the results of analyses when restricted to invasive cancers only. The aforementioned general patterns observed were maintained.
Additional file 1: Table S3 shows that fitting different models to different modes of detection made a highly significant improvement in fit compared with fitting one model to the combined data - which assumes that estimates are the same for both screen-detected and interval cancers - for all models (all P < 0.005).
Discussion
We found that the risk predictors for breast cancer differ by mode of detection. First, there was very strong evidence that interval breast cancers are best predicted when mammographic density was defined conventionally as the white or bright areas, the more so when defined as a percentage. It was more than 20,000 times more likely to be the measure that generated the data than either of the other two measures. Addition of the other measures did not add information, and BMI did not appear to be a predictor of interval disease. On the other hand, we found very strong evidence that screen-detected breast cancers are best predicted by mammographic density when defined as the brighter areas on a mammogram, whether as an absolute or percentage measure. The Cirrocumulus measure was more than 3000 times more likely to be the measure that generated the data than either of the other two measures. Addition of the conventional measures did not add information. Also, in contrast to risk of interval disease, the risk of screen-detected breast cancer associated with BMI increased with age, similar to previous findings on the risk of breast cancer per se [24].
Most importantly, the conventional conception of mammographic density (which we call Cumulus) was not predictive of screen-detected cancers once we fitted mammographic density defined at, in effect, a high pixel-brightness threshold. We have observed this before in case-control studies of breast cancer, for both Australian and Korean women, and when using screen-film and digital mammograms [13,14,15].
Our general observation that risk prediction can be improved by defining density at a higher pixel-brightness threshold has been replicated by Wang and colleagues [25] using digital mammograms. They found, as we have repeatedly found, that once the measure at a higher threshold was included, addition of the conventional measure made no improvement to the fit.
We previously argued that screen-detected cancers mostly reflect inherent risk [12]. We found accumulating evidence that the conventional concept of mammographic density does not apply to risk per se and might be only a surrogate for those aspects of a mammographic image that truly predict risk.
We had also previously noted that interval cancers could be influenced by masking, more rapid growth and/or inherent risk [12]. In this regard, our finding (as previously reported [12]) that the association between BMI and risk of interval cancer did not depend on age, whereas the association between BMI and screen-detected cancer increased with age, is important. The latter is consistent with the epidemiological literature on inherent breast cancer risk (see most recently [26]). This is consistent with risk of interval cancers being more due to masking and more rapid growth than to an increased inherent risk per se and might help explain why we found different mammographic density measures better predicted the different outcomes.
It is not true that, because the three measures are correlated, they are equal proxies of the same underlying exposure. If this was true then the estimates of association would all move towards the null and the width of the confidence intervals would increase substantially when the measures were modelled together. But this did not happen. For screen-detected cancers, when absolute Cirrocumulus was fitted with the other two measures, its association remained significant while the other estimates collapsed, and the standard error of its association of the log scale increased by only 17% from 0.058 to 0.068. On the other hand, the standard error for the now null Cumulus and Altocumulus associations increased by 31% and 30%, respectively. Similar patterns were observed for interval cancer, this time with the Cumulus estimate being the stable one. In the previous study of breast cancer and mammographic density using the Melbourne Collaborative Cohort Study [18], a different set of investigators applied the conventional definition to measure mammographic density (correlation between the Cumulus measure used in this study and the Cumulus measure used in the previous study was 0.86 for dense area and 0.87 for percent dense area). The consistency of our findings on interval cancers with our previous findings based on measurements by other investigators [12], gives confidence in the ability of our investigators performing the measurements in the current study.
The major implication of our findings is that analyses of mammographic images can be used to predict both masking and risk, but that different aspects of the image need to be considered. To date, prediction of masking has been based on BI-RADS, which has in effect been defined in terms of percent density as a categorical variable. Given that we and others [1] have now found that the most informative predictor of masking is a continuous variable, Cumulus as a percentage, this raises issues about whether the current thresholds for defining dense breasts for the purposes of recommending other screening modalities are appropriate. Moreover, the implications of having mammographically dense breasts depend on a woman’s underlying risk of breast cancer, and we have shown that the Cirrocumulus, rather than the Cumulus, measure is an important predictor of risk. Therefore, in order to deal more effectively with the issue of mammographically dense breasts protocols should be devised that take into account that there are multiple and different features of mammographic images that give clinically-important information about different outcomes.
Potential limitations of this study include the older age at baseline of the cohort and, hence, the diagnosis of breast cancer at older ages. It is interesting to note that the OPERA for our predictors of screen-detected cancers was about 1.4, even for Cirrocumulus, consistent with the literature on conventional measures of risk [21], whereas we previously found stronger risk discrimination for predicting breast cancers at younger ages for both Australian [13] and Korean [14, 15] women. It is therefore plausible that the risk discrimination (in the sense we have defined it) is weaker the older the age at measurement, and the longer the time interval between measurement and diagnosis (despite the very strong tracking in age-adjusted mammographic density risk measures over time [27]).
Another limitation is that this study used screen-film images, whereas digital mammography is now the norm. Our previous case–control studies have shown that similar findings on risk arise from studies of digital and film mammograms, but it is nevertheless important to replicate our findings using digital mammography, and for diagnoses at different ages and with different time intervals in different populations. This requires new prospective studies, and we and others are working on developing such resources. Another limitation of this study is that we were not able to divide the period of 2 years used to define interval breast cancers occurring into shorter time periods, such as 12 months as in Boyd et al. [1].
A potential limitation of the translation of our findings into clinical settings is that the measurements require person time and expertise. With respect to expertise, the investigators who performed the measurements are not radiologists but have achieved high repeatability within and between measurers, as aforementioned. We have been funded to train radiologists using the online, and therefore globally relevant, BreastScreen Reader Assessment Strategy initiative [28]. We are also working with colleagues on developing automated measures.
One strength of this study is the highly statistically significant and consistent results observed despite the fact that multiple measurers have been used and the definitions of the different density measurements involve subjective judgements. This is testament to the high repeatability of the average of risk measures across our trained measurers. It also suggests that there is the potential to derive even better predictors of risk, as random measurement error contributes to underestimation of risk gradients. For example, the measurers were blinded to their previous mammographic density measurements on the same mammogram, and better risk prediction might be possible if Cumulus, Cirrocumulus and Altocumulus were measured in that order at the same time, un-blinded to the previous measure. Automated methods would allow multiple thresholds to be considered and, thus, could determine an optimal risk-predicting threshold.
Another strength has been our use of the OPERA concept, which allows us to put risk factors into perspective in terms of their ability to differentiate cases from controls. OPERA relies on deriving the standard deviation of the risk factor after adjusting for other covariates and design variables. Not taking into account the need to adjust the standard deviation for covariates can make a substantial difference. For example, for unadjusted transformed percent mammographic density, the cross-sectional standard deviation was 0.63 for controls. However, after adjusting for age and body mass index, the standard deviation of the residuals became 0.34. Consequently, the log (OPERA) was 44% less than the log (OR) per cross-sectional standard deviation; not adjusting the standard deviation leads to an almost 50% overestimate of the risk-predicting ability of percent mammographic density.
Conclusion
In summary, we have found that more risk-predicting information can be obtained from a mammogram than from the conventional concept of mammographic, or breast, density defined by the white or bright areas. We have also confirmed that the conventional measure of percent mammographic density applies to interval cancers and the masking phenomenon. When it comes to risk per se, however, we have confirmed our previous findings that the conventional measures are not the most informative mammography-based predictors, given that they are no longer significant after adjustment for our new measures based on higher pixel-brightness thresholds. Our newer measures could also be clinically useful given that we have shown that non-specialists can be easily trained and achieve high repeatability within and between measurers. For scientific accuracy, we have used the average of five measurements by five investigators, but reasonable accuracy was obtained by each individual investigator (data not shown); see Fig. 2 of [15] which shows an example of measures of the same mammograms conducted by different investigators.
Our finding that areas of high pixel brightness might better represent the breast tissue with a causal role in breast cancer is very important for multiple disciplines, such as biological research to identify specific tissue markers [29], genetic research to try to find pathways implicated in disease risk [30] and public health initiatives aimed towards targeted, or tailored screening, by identifying women at increased risk of masking and/or of the disease itself.
Abbreviations
- AUC:
-
Area under the receiver operating characteristic curve
- BIC:
-
Bayesian information criterion
- BMI:
-
Body mass index
- CC:
-
Cranio-caudal
- CI:
-
Confidence interval
- HRT:
-
Hormone replacement therapy
- LL:
-
Log likelihood
- OPERA:
-
Odds ratio per adjusted standard deviation
References
Boyd NF, Guo H, Martin LJ, Sun L, Stone J, Fishell E, Jong RA, Hislop G, Chiarelli A, Minkin S, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med. 2007;356(3):227–36.
Kerlikowske K, Grady D, Rubin SM, Sandrock C, Ernster VL. Efficacy of screening mammography. A meta-analysis. JAMA. 1995;273(2):149–54.
Kerlikowske K, Grady D, Ernster V. Benefit of mammography screening in women ages 40-49 years: current evidence from randomized controlled trials. Cancer. 1995;76(9):1679–81.
Dehkordy SF, Carlos RC. Dense breast legislation in the United States: state of the States. J Am Coll Radiol. 2016;13(11S):R53–7.
Mandelson MT, Oestreicher N, Porter PL, White D, Finder CA, Taplin SH, White E. Breast density as a predictor of mammographic detection: comparison of interval- and screen-detected cancers. J Natl Cancer Inst. 2000;92(13):1081–7.
Eriksson L, Czene K, Rosenberg LU, Tornberg S, Humphreys K, Hall P. Mammographic density and survival in interval breast cancers. Breast Cancer Res. 2013;15(3):R48.
Porter PL, El-Bastawissi AY, Mandelson MT, Lin MG, Khalid N, Watney EA, Cousens L, White D, Taplin S, White E. Breast tumor characteristics as predictors of mammographic detection: comparison of interval- and screen-detected cancers. J Natl Cancer Inst. 1999;91(23):2020–8.
Gilliland FD, Joste N, Stauber PM, Hunt WC, Rosenberg R, Redlich G, Key CR. Biologic characteristics of interval and screen-detected breast cancers. J Natl Cancer Inst. 2000;92(9):743–9.
Kirsh VA, Chiarelli AM, Edwards SA, O'Malley FP, Shumak RS, Yaffe MJ, Boyd NF. Tumor characteristics associated with mammographic detection of breast cancer in the Ontario breast screening program. J Natl Cancer Inst. 2011;103(12):942–50.
Domingo L, Blanch J, Servitja S, Corominas JM, Murta-Nascimento C, Rueda A, Redondo M, Castells X, Sala M. Aggressiveness features and outcomes of true interval cancers: comparison between screen-detected and symptom-detected cancers. Eur J Cancer Prev. 2013;22(1):21–8.
Holm J, Humphreys K, Li J, Ploner A, Cheddad A, Eriksson M, Tornberg S, Hall P, Czene K. Risk factors and tumor characteristics of interval cancers by mammographic density. J Clin Oncol. 2015;33(9):1030–7.
Krishnan K, Baglietto L, Apicella C, Stone J, Southey MC, English DR, Giles GG, Hopper JL. Mammographic density and risk of breast cancer by mode of detection and tumor size: a case-control study. Breast Cancer Res. 2016;18(1):63.
Nguyen TL, Aung KY, Evans CF, Dite GS, Stone J, Maclnnis RJ, Dowty JG, Bickerstaffe A, Aujard K, Rommens J, et al. Mammographic density definded by higher than conventional brightness thresholds better predicts breast cancer risk. Int J Epidemiol. 2016. https://doi.org/10.1093/ije/dyw212.
Nguyen TL, Aung YK, Evans CF, Yoon-Ho C, Jenkins MA, Sung J, Hopper JL, Song YM. Mammographic density defined by higher than conventional brightness threshold better predicts breast cancer risk for full-field digital mammograms. Breast Cancer Res. 2015;17(1):142.
Nguyen TL, Choi YH, Aung YK, et al. Breast cancer risk associations with digital mammographic density by pixel brightness threshold and mammographic system. Radiology. 2018;286(2):433–42.
Ireland P, Jolley D, Giles G, O'Dea K, Powles J, Rutishauser I, Wahlqvist ML, Williams J. Development of the Melbourne FFQ: a food frequency questionnaire for use in an Australian prospective study involving an ethnically diverse cohort. Asia Pac J Clin Nutr. 1994;3(1):19–31.
Giles GG, English DR. The Melbourne Collaborative Cohort Study. IARC Sci Publ. 2002;156:69–70.
Baglietto L, Krishnan K, Stone J, Apicella C, Southey MC, English DR, Hopper JL, Giles GG. Associations of mammographic dense and nondense areas and body mass index with risk of breast cancer. Am J Epidemiol. 2014;179(4):475–83.
Byng JW, Yaffe MJ, Jong RA, Shumak RS, Lockwood GA, Tritchler DL, Boyd NF. Analysis of mammographic density and breast cancer risk from digitized mammograms. Radiographics. 1998;18(6):1587–98.
Box GEP, Cox DR. An analysis of transformations. J Royal Stat Soc Series B. 1964;26(2):211–52.
Hopper JL. Odds per Adjusted Standard Deviation: Comparing Strengths of Associations for Risk Factors Measured on Different Scales and Across Diseases and Populations. Am J Epidemiol. 2015;182(10):863–7.
StataCorp: Stata statistical software. In. Edited by 12 R. College Staion: StataCorp LP; 2009.
Kass RE, Raftery AE. Bayes Factors. J Am Stat Assoc. 1995;90(430):773–95.
Macinnis RJ, English DR, Gertig DM, Hopper JL, Giles GG. Body size and composition and risk of postmenopausal breast cancer. Cancer Epidemiol Biomark Prev. 2004;13(12):2117–25.
Wang C, Brentnall AR, Cuzick J, Harkness EF, Evans DG, Astley S. Exploring the prediction performance for breast cancer risk based on volumetric mammographic density at different thresholds. Breast Cancer Res. 2018;20(1):49.
Hopper JL, Dite GS, MacInnis RJ, et al. Age-specific breast cancer risk by body mass index and familial risk: prospective family study cohort (ProF-SC). Breast Cancer Res. 2018;20(1):132.
Krishnan K, Baglietto L, Stone J, et al. Longitudinal Study of Mammographic Density Measures That Predict Breast Cancer Risk. Cancer Epidemiol Biomarkers Prev. 2017;26(4):651–60.
Suleiman WI, Rawashdeh MA, Lewis SJ, McEntee MF, Lee W, Tapia K, Brennan PC. Impact of breast reader assessment strategy on mammographic radiologists’ test reading performance. J Med Imaging Radiat Oncol. 2016;60(3):352–8.
Shawky MS, Martin H, Hugo HJ, Lloyd T, Britt KL, Redfern A, Thompson EW. Mammographic density: a potential monitoring biomarker for adjuvant and preventative breast cancer endocrine therapies. Oncotarget. 2017;8(3):5578–91.
Stone J, Thompson DJ, Dos Santos Silva I, Scott C, Tamimi RM, Lindstrom S, Kraft P, Hazra A, Li J, Eriksson L, et al. Novel Associations between common breast cancer susceptibility variants and risk-predicting mammographic density measures. Cancer Res. 2015;75(12):2457–67.
Acknowledgements
We thank the Breast Cancer Network Australia, the Victorian Cancer Registry, BreastScreen Victoria, the Australian Mammographic Density Research Facility and the participants in the Melbourne Collaborative Cohort Study.
Funding
This work was supported by the National Health and Medical Research Council (grant numbers 251533, 209057 and 504711), the Victorian Health Promotion Foundation, Cancer Council Victoria, Cancer Council NSW, Cancer Australia and the National Breast Cancer Foundation. TLN has been supported by a NHMRC Post-Graduate Scholarship, The Richard Lowell Travelling Scholarship, The University of Melbourne, VCCC Picchi Award for Excellence in Cancer Research and a Cancer Council Victoria Post-doctoral Fellowship. YKA has been supported by the Australian Agency for International Development (AusAID). SL is supported by the Australian Postgraduate Award, International Postgraduate Research Scholarship and The Richard Lowell Travelling Scholarship from The University of Melbourne. JS has been supported by the National Breast Cancer Foundation Post-doctoral Training Fellowship. JLH is a NHMRC Senior Principal Research Fellow and a Distinguished Visiting Professor at Seoul National University. MCS and MAJ are NHMRC Senior Research Fellows.
Availability of data and materials
The datasets used for the current study are available upon reasonable request from the corresponding author.
Author information
Authors and Affiliations
Contributions
TLN developed Altocumulus and Cirrocumulus, performed the statistical analysis, interpreted the results and drafted the manuscript. TLN, YKA, SL, NHT and CFE performed all three mammographic density measurements. JLH, MAJ, JoS and YMS advised on statistical analysis and interpretation and contributed to drafting the manuscript. KK, GSD and JeS made substantial contributions to data distribution and drafting the manuscript. JLH, MCS, GGG, MAJ, LB and DRE conceived the study, interpreted the results and contributed to drafting the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the human research ethics committees of the University of Melbourne and the Cancer Council Victoria and consent was obtained from study participants at the time of recruitment.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Table S1. For interval and screen-detected invasive breast cancer, marginal risk estimates for Cumulus, Altocumulus and Cirrocumulus measures of dense area and percent density adjusted for age and BMI. Table S2. For interval and screen-detected invasive breast cancer, multivariable risk estimates for Cumulus, Altocumulus and Cirrocumulus measures of dense area and percent density adjusted for age and BMI. Table S3. Combined (all breast cancer); total (summary of interval and screen-detected); and -2Δ of log likelihood (LL) for Cumulus, Altocumulus and Cirrocumulus measures of dense area and percent density adjusted for age and BMI and P value for the differences. (DOCX 36 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Nguyen, T.L., Aung, Y.K., Li, S. et al. Predicting interval and screen-detected breast cancers from mammographic density defined by different brightness thresholds. Breast Cancer Res 20, 152 (2018). https://doi.org/10.1186/s13058-018-1081-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13058-018-1081-0