Abstract
Critical illness results in millions of deaths each year. Care for those with critical illness is often neglected due to a lack of prioritisation, co-ordination, and coverage of timely identification and basic life-saving treatments. To improve care, we propose a new focus on essential emergency and critical care (EECC)—care that all critically ill patients should receive in all hospitals in the world. Essential emergency and critical care should be part of universal health coverage, is appropriate for all countries in the world, and is intended for patients irrespective of age, gender, underlying diagnosis, medical specialty, or location in the hospital. Essential emergency and critical care is pragmatic and low-cost and has the potential to improve care and substantially reduce preventable mortality.
Similar content being viewed by others
Introduction
“Help! This patient is very sick, we must do something immediately!”; a frequently heard cry in hospitals all over the world. Such patients are “critically ill”. The term is commonly used, and yet its definition is elusive. Using a working description of “any immediately life-threatening, reversible condition”, critical illness is the most severe stage of acute illness and, if left untreated, often leads to a poor outcome or death [1]. Critical illness can occur in anyone irrespective of age, gender, or social status, it can begin in the community or in hospital, and does not respect traditional divisions into medical specialties. Patients with conditions such as sepsis, pneumonia, eclampsia, haemorrhage, trauma, peritonitis, asthma, and stroke can all have or develop critical illness and, as such, critical illness has been crudely estimated to result in several million deaths globally each year [2]. In this article, we propose a new concept of essential emergency and critical care (EECC), defined as “the care that all critically ill patients should receive in all hospitals in the world”.
Emergency and critical care
Patients with critical illness require care and require it quickly. This is “emergency and critical care”, the identification and continued observation, assessment, and treatment required to manage critical illness [3]. Emergency and critical care focuses on resuscitating unstable patients and allowing time for recovery or the effect of specific therapies to improve outcomes and prevent death. We use emergency and critical care in the broad sense of care provided to all critically ill patients. Emergency and critical care is therefore for those who are critically ill at arrival, or who were stable and subsequently deteriorated, and can be provided anywhere in the hospital: in the emergency department, the intensive care unit (ICU), general wards, post-operative recovery units, and high-dependency units [2, 3].
Neglected emergency and critical care
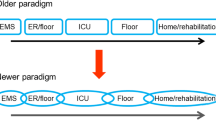
There are several reasons to suspect that emergency and critical care may be neglected. Firstly, the approach used by most medical specialties and health systems is typically “vertical”, meaning that diagnosis-related and specialty-related care are prioritised rather than the severity-related “horizontal” approach of emergency and critical care (Fig. 1). Moreover, in hospitals in low-resource settings and in general wards in high-resource settings, there can be low staffing levels, a lack of equipment, and limited knowledge or awareness of emergency and critical care which can result in a failure to identify critical illness and an under-prioritisation of emergency and critical care [4,5,6,7]. Secondly, there is a lack of commonly agreed definitions and criteria for either the identification of critical illness, or for the provision of emergency and critical care. Thirdly, emergency and critical care can be conflated with technologically advanced and expensive care on ICUs. ICUs have spread worldwide and developed rapidly since their origin in the 1950s and are now specialised units managing patients with multi-organ failure [2, 3, 8,9,10]. ICU treatment is expensive and can cost up to 1% of the economy of a high-income country [11], and is thus rationed. As the number of ICU beds per million population varies substantially—from 292 in Germany, 58 in Sweden, 25 in Sri Lanka, to 1 in Uganda [10, 12]—it is clear that ICUs cannot be the sole providers of care for all critically ill patients. Finally, it can be presumed that the acute care provided at arrival to hospital is sufficient, and deteriorating patients in the hospital can be missed. While a proportion of critically ill patients do receive emergency and critical care in emergency departments, in ICUs, or in other hospital settings, there are many who are not identified or do not receive the care that they so urgently need.
The consequences can be poor quality care for critically ill patients. The co-ordination of emergency and critical care may be difficult within a hospital and within the health system. The basic, life-saving therapies that form the core of emergency and critical care may be forgotten. A focus on expensive ICU beds rather than broader emergency and critical care may drain valuable resources, treating a few individuals at a high cost instead of many critically ill at a low cost, and a focus on acute care in emergency departments can exclude hospital in-patients. The likely result is substantial preventable mortality and morbidity.
Essential emergency and critical care
To improve the care of the critically ill, we propose a new focus on “essential emergency and critical care” (EECC). We define EECC as “care that all critically ill patients should receive in all hospitals in the world”. EECC is a concept that should be a crucial part of universal health coverage; it is low-cost and appropriate for all countries in all settings in the world, and is intended for patients irrespective of age, gender, underlying diagnosis, medical specialty, or location. EECC is a set of actions and treatments plus the system-wide requirements for their provision. For simplicity of definition, we limit EECC to care in hospitals, rather than in primary care clinics or the pre-hospital environment.
As the critically ill are a heterogeneous group it is important to define what is not included in EECC. It is not the diagnosis and definitive treatment that focus on the pathophysiological cause of the critical illness—actions which are also important for the patient—and it is not the “advanced emergency and critical care” that may also be available in high-resource settings (Fig. 2). EECC is the low-cost, most basic level of emergency and critical care and should be provided in all settings. The available resources will determine what additional care is appropriate or possible. EECC is not the palliative care required for dying patients, or care when a patient’s condition is so severe that recovery has been deemed impossible. While the decision to provide palliative care instead of EECC can be very challenging, it is nevertheless of great importance and the adoption of EECC must not be allowed to lead to increased suffering for patients for whom there is no hope of a good recovery.
EECC can be visualised in a framework (Fig. 3), and the elements of EECC are described in Table 1. EECC is divided into two key domains: identification and care. To identify a case and to provide care, “hospital readiness” (the necessary facilities or structures in the hospital) is required. Subsequently, “clinical practice” (the processes of care) is required. The product of the identification and care is the output, or “effective coverage” [13], of EECC: the proportion of all critically ill patients in hospital who receive EECC. Our hypothesis is that a high effective coverage of EECC leads to good outcomes and survival for many critically ill patients.
Essential emergency and critical care (EECC) in hospitals: a conceptual framework. The numbers in circles correspond to the text in Table 1
The principles underlying EECC are not new. Florence Nightingale in the 1850s described more frequent observations of the sickest patients and moved them closest to the nurses’ station, and the first ICUs opened 60 years ago [3]. The specialties of emergency medicine and intensive care medicine have the principles of EECC as core competencies, and several modern initiatives implicitly utilise EECC. Triage systems in emergency departments categorise patients into levels of urgency and may specify the care required for patients at each triage level [14]. Vital sign-based early warning scores and treatment protocols [15,16,17], rapid response teams of ICU outreach staff [18, 19], and initiatives for improving ward care [20, 21] aim to improve processes for the identification and care of sick hospital patients. EECC can provide a unifying concept for such initiatives, ensuring a system-wide emphasis on illness severity and prioritisation for those at highest risk so that the most fundamental care for the critically ill is delivered throughout the hospital. EECC has global relevance: in a low-resource setting, EECC may entail directing scarce human resources towards the sickest patients and ensuring limited medicines and equipment are used where they could have the biggest impact; in a high-resource setting, EECC may ensure that vertical, specialist services do not neglect the identification and care of critically ill patients.
The idea of “essential” services has been used in other disciplines. The World Health Organization (WHO) has had an essential medicines list since 1977 [22]. The WHO guidelines for essential trauma care are defined as “achievable standards for trauma treatment services which could realistically be made available to almost every injured person in the world” [23]. The WHO Guide to Essential Practice for Pregnancy, Childbirth, Postpartum and Newborn Care is now in its third edition [24]. The word “essential” is used to define a minimum set of actions that should always be implemented. It is a conceptual way of “raising-the-bottom”, in contrast to frequently used “lifting-the-top” approaches.
Impact
What would be the impact of improving the effective coverage of EECC? Hospitals providing EECC to all their patients would have a system-wide approach for managing critical illness, an approach that could prevent deterioration and save lives at a low cost. Critically ill patients would be identified and treated quickly throughout the hospital. Critical care gaps that exist between the emergency department and the wards, between the ICU and the wards, and between specialties would be closed. No patient would die from a condition that EECC could prevent.
The way forward
To operationalise EECC, we propose the following research and policy agenda. Firstly, clear definitions of critical illness and emergency and critical care should be established. Secondly, the specific values and contents of EECC should be defined in a transparent way, involving the opinions of diverse stakeholders and experts. Thirdly, a research agenda should be designed, evaluating the current effective coverage of EECC (see Fig. 3), the impact of EECC interventions, and the effectiveness of implementation strategies. Finally, medical educators, policy makers, and health system experts should be involved throughout the process to ensure policy relevance and buy-in, shortening the distance from research findings to curriculum design and policy implementation.
Conclusions
We have described the concept of essential emergency and critical care (EECC). We believe EECC should be a crucial part of universal health coverage, and that EECC has the potential to improve the care given to critically ill patients in hospitals in all settings in the world and substantially reduce preventable mortality.
Abbreviations
- EECC:
-
Essential emergency and critical care
- ICU:
-
Intensive care unit
References
Baker T. Critical care in low resource settings. Stockholm: Karolinska Institutet; 2015.
Adhikari NK, Fowler RA, Bhagwanjee S, Rubenfeld GD. Critical care and the global burden of critical illness in adults. Lancet. 2010;376(9749):1339–46.
Vincent JL. Critical care—where have we been and where are we going? Critical care. 2013;17(Suppl 1):S2.
Baelani I, Jochberger S, Laimer T, Otieno D, Kabutu J, Wilson I, Baker T, Dunser MW. Availability of critical care resources to treat patients with severe sepsis or septic shock in Africa: a self-reported, continent-wide survey of anaesthesia providers. Critical care. 2011;15(1):R10.
Kause J, Smith G, Prytherch D, Parr M, Flabouris A, Hillman K. A comparison of antecedents to cardiac arrests, deaths and emergency intensive care admissions in Australia and New Zealand, and the United Kingdom—the ACADEMIA study. Resuscitation. 2004;62(3):275–82.
McQuillan P, Pilkington S, Allan A, Taylor B, Short A, Morgan G, Nielsen M, Barrett D, Smith G, Collins CH. Confidential inquiry into quality of care before admission to intensive care. BMJ. 1998;316(7148):1853–8.
Schell CO, Castegren M, Lugazia E, Blixt J, Mulungu M, Konrad D, Baker T. Severely deranged vital signs as triggers for acute treatment modifications on an intensive care unit in a low-income country. BMC Res Notes. 2015;8:313.
Vincent JL, Marshall JC, Namendys-Silva SA, Francois B, Martin-Loeches I, Lipman J, Reinhart K, Antonelli M, Pickkers P, Njimi H, et al. Assessment of the worldwide burden of critical illness: the Intensive Care Over Nations (ICON) audit. Lancet Respir Med. 2014;2(5):380–6.
Murthy S, Leligdowicz A, Adhikari NK. Intensive care unit capacity in low-income countries: a systematic review. PLoS One. 2015;10(1):e0116949.
Haniffa R, De Silva AP, Iddagoda S, Batawalage H, De Silva ST, Mahipala PG, Dondorp A, de Keizer N, Jayasinghe S. A cross-sectional survey of critical care services in Sri Lanka: a lower middle-income country. J Crit Care. 2014;29(5):764–8.
Halpern NA, Pastores SM, Greenstein RJ. Critical care medicine in the United States 1985–2000: an analysis of bed numbers, use, and costs. Crit Care Med. 2004;32(6):1254–9.
Rhodes A, Ferdinande P, Flaatten H, Guidet B, Metnitz PG, Moreno RP. The variability of critical care bed numbers in Europe. Intensive Care Med. 2012;38(10):1647–53.
Baker U. Closing the quality gap. Stockholm: Karolinska Institutet; 2017.
Farrohknia N, Castren M, Ehrenberg A, Lind L, Oredsson S, Jonsson H, Asplund K, Goransson KE. Emergency department triage scales and their components: a systematic review of the scientific evidence. Scand J Trauma Resusc Emerg Med. 2011;19:13.
Smith GB, Prytherch DR, Meredith P, Schmidt PE, Featherstone PI. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation. 2013;84(4):465–70.
Rylance J, Baker T, Mushi E, Mashaga D. Use of an early warning score and ability to walk predicts mortality in medical patients admitted to hospitals in Tanzania. Trans R Soc Trop Med Hyg. 2009;103(8):790–4.
Baker T, Schell CO, Lugazia E, Blixt J, Mulungu M, Castegren M, Eriksen J, Konrad D. Vital signs directed therapy: improving care in an intensive care unit in a low-income country. PLoS One. 2015;10(12):e0144801.
Chan PS, Jain R, Nallmothu BK, Berg RA, Sasson C. Rapid response teams: a systematic review and meta-analysis. Arch Intern Med. 2010;170(1):18–26.
Winters BD, Weaver SJ, Pfoh ER, Yang T, Pham JC, Dy SM. Rapid-response systems as a patient safety strategy: a systematic review. Ann Intern Med. 2013;158(5 Pt 2):417–25.
Chokotho L, Mulwafu W, Singini I, Njalale Y, Jacobsen KH. Improving hospital-based trauma care for road traffic injuries in Malawi. World J Emerg Med. 2017;8(2):85–90.
Cummings MJ, Goldberg E, Mwaka S, Kabajaasi O, Vittinghoff E, Cattamanchi A, Katamba A, Kenya-Mugisha N, Jacob ST, Davis JL. A complex intervention to improve implementation of World Health Organization guidelines for diagnosis of severe illness in low-income settings: a quasi-experimental study from Uganda. Implement Sci. 2017;12(1):126.
Laing R, Waning B, Gray A, Ford N, t Hoen E. 25 years of the WHO essential medicines lists: progress and challenges. Lancet. 2003;361(9370):1723–9.
WHO. Guidelines for essential trauma care. Geneva: WHO Press; 2004.
WHO: Pregnancy, childbirth, postpartum and newborn care: a guide for essential practice. Geneva: World Health Organization; 2015.
Funding
The article was not funded by any funding source.
Author information
Authors and Affiliations
Contributions
COS and TB contributed to the conception of the article. TB wrote the first and subsequent drafts. All authors contributed to the development and critical revisions of the article, and read and approved the final manuscript.
Corresponding author
Ethics declarations
Authors’ information
The authors are an experienced group of researchers and clinicians working in Malawi and Sweden.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Schell, C.O., Gerdin Wärnberg, M., Hvarfner, A. et al. The global need for essential emergency and critical care. Crit Care 22, 284 (2018). https://doi.org/10.1186/s13054-018-2219-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13054-018-2219-2