Abstract
Vitamin D is a fat-soluble prohormone best known for its role in maintaining calcium homeostasis. Large numbers of epidemiological studies have shown that vitamin D plays an important role in cancer prevention by regulating cellular proliferation and metabolism. Studies of the cellular mechanism of vitamin D in ovarian cancer strongly suggest that it exhibits protective and antitumorigenic activities through genomic and nongenomic signal transduction pathways. These results indicate that vitamin D deficiency results in an increase in the risk of developing ovarian cancer and that vitamin supplements may potentially be an efficient way of preventing cancer. Consequently, this review describes the epidemiology, molecular mechanism and evidence linking vitamin D deficiency to ovarian cancer.
Similar content being viewed by others
Background
Ovarian cancer is the fifth leading cause of cancer death, with the highest fatality rate among women [1]. It is often diagnosed at an advanced stage in most patients with a survival rate of less than 40% at 5 years [2]. No significant improvement in ovarian cancer therapies using surgical debulking combined with platinum-based drug therapies has emerged over the past few decades. Consequently, new biomarkers that enable the early detection and prevention before disease onset are required for ovarian cancer.
Vitamin D is a fat-soluble prohormone best known for its role in calcium and bone homeostasis. Nearly 3% of the human genome are regulated by the vitamin D endocrine system [3]. Some epidemiological, preclinical and clinical studies have shown that vitamin D exhibited impressive antioncogenic activity and cancer prevention properties. Vitamin D level are determined by sunlight exposure, diet and supplements. Increasing evidences showed that low vitamin D level was associated with an increased risk of developing ovarian cancer [4,5,6]. This review aims to highlight the advancements of vitamin D in ovarian cancer that might provide new therapeutic methods and preventative information. The Literature identification and selection were supplied in supplemental methods (Additional file 1).
Vitamin D and its receptor: Synthesis, sources and metabolism
Synthesis and sources of vitamin D
As shown in Fig. 1, vitamin D is synthesized in skin exposed to sunlight or obtained from dietary sources. Sunlight, specifically ultraviolet-B radiation, is the main pathway for producing adequate levels of vitamin D. It could convert 7-dehydrocholesterol (7-DHC) into vitamin D3 in the skin. Vitamin D3 then enters the blood stream as complexes with vitamin D binding protein (DBP) and albumin. Levels of DBP-bound vitamin D and free vitamin D are maintained at equilibrium to ensure adequate levels of circulating hormone. 1,25(OH)2D3 (calcitriol), the active form of vitamin D3, is synthesized by a series of enzymes that are mainly distributed in the liver and kidney. Firstly, vitamin D3 is converted to 25-hydroxyvitamin D3 (25(OH)D3) in the liver, which is the main vitamin D metabolite present in the blood and the most reliable indicator of vitamin D status. 25(OH)D3 is then converted into 1,25(OH)2D3 in the kidneys or other target tissues through a series of enzymatic reactions. 1,25(OH)2D3 then enters target cells, where it binds to vitamin D receptor (VDR) in the nucleus that regulate cellular function [7].
Synthesis, metabolism and anticancer mechanism of vitamin D. Sunlight, specifically ultraviolet-B radiation, converts 7-dehydrocholesterol (7-DHC) into vitamin D3 in the skin. Vitamin D3 then enters the blood stream as complexes with vitamin D binding protein (DBP) and albumin. Liver mitochondrial and microsomal 25-hydroxylases (25-OHases), encoded by the gene CYP27A1, carry out the first hydroxylation of vitamin D to form 25(OH)D3. 25(OH)D3 is then 1a-hydroxylated by mitochondrial 1a-hydroxylase (1a-OHase) encoded by the CYP27B1 gene to form 1a,25(OH)2D3 in the kidneys and other tissues. The vitamin D receptor (VDR) is a member of the nuclear receptor family that regulates gene transcription by forming a hetero-dimer with RXR, which binds to vitamin D-response elements (VDRE) in the promoter regions of target genes. Several 1,25(OH)2D3 target genes have been reported multiple molecular pathways of anti-tumor actions of 1,25(OH)2D3 in ovarian cancer. These include (1) the up-regulation of cyclin-dependent kinase(CDK) inhibitors P21 and P27 and the subsequent inhibition of G1/S checkpoint; (2) G2/M arrest by 1,25(OH)2D3 through the induction of GADD45; (3) the inhibition of tumor angiogenesis due to suppressive effects on the expression of HIF-1/VEGFR pathway; (4) the suppression of invasion and metastasis via the up-regulation of E-cadherin and the down-regulation of β-catenin; (5) the induction of cell apoptosis by the suppression of hTERT mRNA transcription which miR-498 was a primary target gene of 1,25(OH)2D3; (6) the down-regulation of the expression of COX-1 and COX-2 to inhibit the inflammatory process; (7) 1,25(OH)2D3 can induce a slow increase of Ca2+ that activates CaMKK-β, a Ca2+-activated kinase that was identified as a direct activator of AMPK. DNA-damage-inducible transcript 4 (DDIT4) played a critical role in the cellular response to cell metabolism by the mTOR pathway
The vitamin D receptor is a member of the nuclear receptor family that regulates gene transcription by forming a hetero-dimer with RXR, which binds to vitamin D-response elements (VDRE) in the promoter regions of target genes [8]. VDR is weakly expressed in normal ovarian cells, but it is highly expressed in ovarian cancer cell lines and tumor tissues [9]. High levels of VDR expression was associated with improved survival rates in ovarian cancer [9, 10].
Enzyme regulation
Enzymatic reactions play an important role in the biosynthesis and degradation of 1,25(OH)2D3. Liver mitochondrial and microsomal 25-hydroxylases (25-OHases), encoded by the gene CYP27A1, carry out the first hydroxylation of vitamin D to form 25(OH)D3. 25(OH)D3 is then 1a-hydroxylated by mitochondrial 1a-hydroxylase (1a-OHase) encoded by the CYP27B1 gene to form 1a,25(OH)2D3 in the kidneys and other tissues. These two enzymes represent the rate-limiting steps for 25(OH)D3 and 1a,25 (OH)2D3 biosynthesis, with their activity regulated by high concentrations of 25(OH)D3 and 1a,25(OH)2D3 respectively, as part of a negative feedback loop [11, 12]. A 24-hydroxylase encoded by the CYP24A1 gene is primarily responsible for catabolizing 1,25(OH)2D3 which is converted into calcitroic acid that is then excreted. In addition, CYP24A1 expression is strongly induced by high levels of 1,25(OH)2D3, with this feedback mechanism operating to maintain appropriate 1,25(OH)2D3 serum level [12]. However, the amount of 1,25(OH)2D3 present in tumor cells is decreased by this feedback loop [8]. The self-regulation of 1,25(OH)2D3 induces its own inactivation.
It has been reported that CYP27A1 and CYP27B1 were overexpressed in ovarian cancer cells, which can result in an increase in localized 1,25(OH)2D3 concentrations in the tumor and promote anticancer activity [7, 13]. Additionally, CYP24A1 has also been found to be highly expressed in many cancers including ovarian cancer, which is associated with the inverse impact of 25(OH)D3 on cancer risk levels [14,15,16]. Another study showed that decreased CYP27B1 was associated with a more aggressive phonotype for ovarian cancer [17]. Therefore, increasing CYP27A1 and CYP27B1 expression and decreasing CYP24A1 production may be beneficial for inhibiting tumor growth.
The epidemiology of vitamin D and ovarian cancer
Circulating vitamin D and ovarian cancer risk
The hypothesis that levels of vitamin D might be related to cancer rates was first proposed by the Garland brothers in 1980, who reported that people living at higher latitudes with vitamin D deficiency had an increased risk of developing malignant tumors [18]. Their subsequent ecologic study provided further evidence that there is a strong inverse correlation between mean daily solar radiation levels and ovarian cancer mortality [19]. 25(OH)2D3 has a longer half-life than 1,25(OH)2D3, whose serum levels are currently the gold standard for evaluating vitamin D status. Yin et al. provided meta-analysis of 10 cohort studies on the incidence of ovarian cancer, finding an average increase in 25(OH)2D3 of 20 ng/ml, with an RR (95% confidence interval, CI) value of 0.83 (0.63–1.08) [4]. Ong et al. used two-sample MR methodology to demonstrate a causal role relating low levels of circulating vitamin D with high-grade serous ovarian cancer [5]. These studies suggested the possibility of an inverse association, however these associations were not considered statistically significant. Different results may be attributed to racial disparities, the season of diagnosis, different cut-off of 25(OH)D concentration, UVB exposure, obesity and socioeconomic status.
A case-control study of 1631 women diagnosed with epithelial ovarian cancer have shown that higher 25(OH)D concentrations are associated with longer survival rates (adjusted HR: 0.93; 95%CI: 0.88–0.99 per 10 nmol/L) [6]. Colorectal cancer patients with high prediagnostic 25(OH)D levels (> 30 ng per mL) have a lower risk of cancer-specific and total mortality [20,21,22]. Vitamin D status at the time of diagnosis may also be an independent predictor of prognosis, implying that vitamin D supplementation may be an effective treatment for early stage cancer.
UVB and ovarian cancer risk
Several ecological studies have shown that ovarian cancer incidence and mortality are inversely associated with UVB exposure that is responsible for vitamin D production in the skin. [10, 23, 24] A population-based case-control study examined the association between lifetime ambient UVR and ovarian cancer risk, which found that women who spent their lives in areas with high levels of ambient UVR had a lower risk of developing epithelial ovarian cancer [25]. They reported a greater incidence of ovarian cancer in North America and northern Europe than in Asia or Africa. Furthermore, increasing latitude is associated with higher mortality levels in the United States [19]. However, a different cohort study using the TOMS database to estimate ambient UVR found no association between UVB exposure and the risk of ovarian cancer [26].
VDR polymorphisms and ovarian cancer risk
Several VDR gene polymorphisms have been identified that may influence cancer risk. The most frequently studied single nucleotide polymorphisms in ovarian cancer is FokI (rs2228570/ rs10735810), which is located at the 5′ end of the VDR gene. This polymorphism results in the VDR protein sequence being altered, producing a protein that is 3 amino acids longer for carriers of the f allele, than for carriers of the F allele. Lurie et al. were the first to report that the FokI f allele was associated with increased risk of ovarian cancer in Caucasian women [27]. It was subsequently found that the incidence of the f allele was highest amongst younger women (age < 50), which may be due to the promoting effect of estrogen on mRNA expression for VDR [28]. Tworoger et al. also observed that the pooled OR comparing ovarian cancer women with ff versus FF genotype was 1.26 (95% CI, 1.01–1.56) [29]. In Indian population, FokI is also associated with the incidence of ovarian cancer [30]. Meta-analysis has also shown that populations with FokI ff allele were associated with a 10% increased cancer risk (pooled OR = 1.10, 95%CI = 0.99–1.22) [31].
BsmI (rs1544410), ApaI (rs7975232), and TaqI (rs731236) are situated in the 3′ untranslated region of the VDR gene, which does not affect VDR protein structure, so these polymorphisms are likely to regulate VDR mRNA stability [32]. Meta-analysis of 7 case-control studies showed that the BsmI G/A gene variant may be a moderate risk factor for the development of ovarian cancer in European populations when compared to North American or Asian populations [33]. ApaI has been shown to affect VDR mRNA stability. Grant et al. detected a significant association between Apa1 and invasive ovarian cancer in African American women [34]. However, no association of the Taq1 variant with ovarian cancer was found. In addition, another single nucleotide polymorphism Cdx2 A allele was found to improve VDR activity and decrease ovarian cancer risk [27]. Therefore, these genetic differences may be important factors that impact VDR association with ovarian cancer. Other factors including circulating vitamin D levels, sun exposure and disease stage may also modify the effect of VDR variants on ovarian cancer risk [35]. Therefore, more studies in different ethnic populations are required to identify the role of VDR gene polymorphisms in the development of ovarian cancer.
The anticancer mechanism of vitamin D in ovarian cancer
Different studies have described several mechanisms through which VDR can inhibit tumor growth including genomic and non-genomic signal transduction pathways. 1,25(OH)2D3 binds to vitamin D receptor (VDR), translocates to nucleus, where it forms a VDR/retinoid X receptor complex that binds to vitamin D response elements (VDREs) that regulate gene transcription (illustrated in Fig. 1). In addition, vitamin D exerts some non-genomic effects including regulation of calcium and phosphate homeostasis pathways, as well as activating protein kinase C, protein kinase A (PKA), phosphatidylinositol-3 kinase (PI3K) and phospholipase C (PLC) [8, 36].
The VDR variant may also be involved in ovarian cancer carcinogenesis. For example, the FokI f allele resulted in three amino acids longer VDR protein than the F allele. This mutant VDR protein was less responsive to 1,25(OH)2D3 and had lower transcriptional activity [37, 38]. Etten et al. reported that this extended VDR results in lower NF-kB transcriptional activation, leading to reduced IL-12 expression and a weaker immune response [39].
Cell cycle and apoptosis
Expression of VDR is an important factor in tumor cell response to 1,25(OH)2D3, which is known to influence gene expression of p53, Ras, MAPK, PI3, MYC, HIF1a, BRCA1, CDKN1A and GADD45 [8, 12, 40,41,42,43]. Jiang et al. have shown that 1,25(OH)2D3 could inhibit cancer growth by arresting cells at the G2–M transition phase and induce cell death through VDR-mediated, p53-independent induction of GADD45 in ovarian cancer cells [44]. They also demonstrated that the 1,25(OH)2D3 analogue EB1089 inhibited the proliferation of ovarian cancer without inducing hypercalcemia in vivo [45]. VDR-mediated induction of BRCA1 was found to be closely correlated with the anti-proliferative activity of 1,25(OH)2D3 in breast and prostate cancer cells [40]. Studies have also shown that profound crosstalk exists between p53 and VDR, with the VDR gene being a direct target of p53 and its family members [41].
1,25(OH)2D3 promotes the expression of cyclin-dependent kinase(CDK) inhibitors P21 and P27 with reduced CDK activity. Li et al. demonstrated that 1,25(OH)2D3 arrested ovarian cancer cells at the G1/S checkpoint and stabilized the p27 protein through downregulation of cyclin E/cyclin-dependent kinase 2 and Skp1-Cullin-F-box protein/Skp2 ubiquitin ligase [46]. Bai et al. identified that 1,25(OH)2D3 suppressed ovarian cancer cells at the G1/S checkpoint through downregulation of epidermal growth factor receptor (EGFR) transcription [47]. Collectively, these studies confirmed that vitamin D suppressed cell proliferation through inhibitory effects on several regulators of the cell cycle.
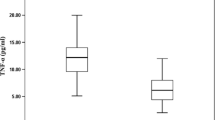
Down-regulation of telomerase activity by vitamin D that induce apoptosis and suppress ovarian cancer cell growth may occur via other pathways [48]. Studies by Kasiappan et al. showed that 1,25(OH)2D3 decreased hTERT mRNA transcription to induce cell apoptosis, suggesting that miR-498 was a primary target gene of 1,25(OH)2D3 for ovarian cancer [49]. Microarray analysis has also revealed that 1,25(OH)2D3 regulated the extrinsic apoptotic pathway through tumor necrosis factor such as TRAIL, Fas and caspase-7 in ovarian cancer cells [50].
Angiogenesis
Growing evidence indicates that vitamin D has a potential role for inhibiting tumor angiogenesis [51,52,53,54]. Hypoxic regions exist in most solid tumors is a major pathophysiologic condition that regulates angiogenesis. Increased angiogenesis occurs as a cellular adaptation to hypoxia, which is controlled by hypoxia inducible factor-1(HIF-1). HIF1 target genes, such as vascular endothelial growth factor (VEGFR), are inhibited by 1,25(OH)2D3, and this molecular inhibition is mediated via a HIF-dependent pathway [55]. A study by Chung et al. has shown that vitamin D decreased growth inhibition of tumor-derived endothelial cells from VDR knockout mice. Moreover, loss of VDR resulted in an increase in HIF-1α, VEGF, angiopoietin 1 and platelet-derived growth factor levels [56].
Invasion and metastasis
Tumor metastasis is the primary factor for treatment failure in patients with ovarian cancer. The omentum is the most common tissue type affected by ovarian cancer metastasis, because it is comprised of large numbers of adipocytes, immune cells, microvascular cells and fibroblasts, which create a good microenviroment for cancer cell growth. In vivo and vitro experiments suggested that 1,25(OH)2D3 and its analog EB1089 could suppress the spread of cancer cells through the omentum by binding to VDR present in epithelial cancer and stromal cells [57]. Moreover, Liu et al. found that 1,25(OH)2D3 upregulated the expression of E-cadherin and VDR and downregulated the expression of β-catenin in ovarian cancer induced by 7,12-dimethylbenz[a]anthracene (DMBA) [58].
Inflammatory response
Increased inflammation has been recognized as a risk factor for the development of cancer [59]. Mantovani et al. proposed that a continuous inflammatory environment would result in reduced levels of 25(OH)D, which may provide an explanation why cancer is associated with low levels of 25(OH)D [60, 61]. The two isoenzymes cyclooxygenase 1 and 2 (COX-1 and COX-2) are involved in inflammatory process arrised in ovarian cancer. High-expression levels of COX-2 was associated with poor survival rates in ovarian cancer patients [62]. Vitamin D combined with the COX-2 inhibitor celecoxib was shown to obviously decrease ovarian cancer growth rates when compared to celecoxib alone [63].
Tumor metabolism
Dysregulated tumor cell metabolism has recently been identified to play an important role in the development of cancer. Several studies have shown that vitamin D influences regulation of glucose and fatty acid metabolism in cancer cells. Santos et al. have reported that 1,25(OH)2D3 inhibited the expression of glycolytic enzymes including hexokinase II (HKII) and lactate dehydrogenase A (LDHA) in breast cancer [64]. Tomasz et al. described that 1,25(OH)2D3 also inhibited de novo fatty acid synthesis through down-regulation of pyruvate carboxylase, while acetyl-CoA carboxylase (ACC) and fatty acid synthase (FASN) were not altered in breast cancer cell [65]. 1,25(OH)2D3 has also been shown to decrease the expression of genes regulating glucose, fatty acid and glutamine metabolism in prostate cancer cells [66]. Moreover, glutamine metabolism in breast cancer was also decreased by 1,25(OH)2D3 intervention [67]. However, no studies were found about the impact of 1,25(OH)2D3 on ovarian cancer cell metabolism.
Recent studies have demonstrated the effects of 1,25(OH)2D3 on metabolism-related signaling molecules, including AMPK, DDIT4, mTOR and AKT [68,69,70,71]. 1,25(OH)2D3 can induce a slow increase in Ca2+ concentration that activates CaMKK-β, which is a Ca2+-activated kinase that was identified as a direct activator of AMPK [72]. DNA-damage-inducible transcript 4 (DDIT4), also known as REDD1/Dig2/RTP801, was over-expressed in high-grade ovarian cancer and significantly linked with late stage cancer patients [73]. DDIT4 played a critical role in cellular response to energy stress via the TSC/mTOR pathway [74]. It has been reported that 1,25(OH)2D3 regulates mTOR signaling through inducing DDIT4 expression [75]. In addition, study found that AKT S473 activation was associated with over-expression of DDIT4 in ovarian cancer tissues [73]. These observations implied that the action of 1,25(OH)2D3 on the mTOR signal pathway may have a key role in cancer metabolism. Therefore, it is clear that further understanding of the pathway relating vitamin D to cancer cell metabolism is required.
Obesity has been proposed to lead to low body vitamin D status, because vitamin D is a fat soluble molecule that can be stored in excess adipose tissue [76]. Strong links between vitamin D and obesity have been further established [77]. It was reported that vitamin D deficiency was associated with an increased risk of ovarian cancer in overweight and obese women [78, 79]. Obesity has been a significant risk factor for ovarian cancer [80]. It was meaningful to elucidate the regulatory mechanisms of vitamin D in the metabolic pathway between obesity and cancer. Leptin is an adipocyte-derived adipokine that plays a crucial role in regulating appetite and energy balance, that is strongly elevated in obese ovarian cancer patients [81]. Bai et al. reported evidence that 1,25(OH)2D3 had a suppressive effect on leptin and HFD-induced ovarian cancer through miR498 pathway [82]. This means that appropriate control of 1,25(OH)2D3 levels may offer an effective strategy for reducing ovarian cancer risk in obese women.
Vitamin D for the treatment and prevention of ovarian cancer
Compared with traditional chemotherapy regiments, the use of 1,25(OH)2D3 or its analogs as a treatment for cancer is not an effective therapy. However, increased antitumor effects using 1,25(OH)2D3 combination therapies offer an opportunity for developing clinical treatments for ovarian cancer [12]. Administration of 1,25(OH)2D3 in vitro, has been shown to significantly enhance antitumor efficacy in the presence of chemotherapeutic agents such as cisplatin, carboplatin, docetaxel or paclitaxel [36, 83].
Growing evidence suggests that vitamin D deficiency is correlated to ovarian cancer, 1,25(OH)2D3 and its analogs have been shown to be promising agents for cancer prevention. Excess exposure to sunlight can result in skin diseases, however vitamin D supplementation can be used to improve the vitamin D status of patients. A healthy blood level of 25-hydroxyvitamin D of > 30 ng/mL has been recommended by the Endocrine Society’s Practice Guidelines [84]. Vitamin D supplementation alone was found no association with a decreased risk of ovarian cancer in African-American women [85]. Trivedi et al. reported no effects of 4 monthly doses of 100,000 IU vitamin D on cancer incidence or mortality in 2686 people over a 5-year period [86]. However, randomized controlled trials using vitamin D and calcium on post-menopausal women have found more beneficial effect in reducing the incidence of cancer compared with vitamin D supplement alone. Lappe et al. have reported 4-year trials on the RR of patients developing cancer. They compared patients who took an average of 1450 mg/day calcium with those taking 1450 mg/day calcium plus 1000 IU/day vitamin D3, which gave values of 0.532 (95%CI: 0.27 to 1.03; P = 0.063) and 0.40 (95%CI, 0.20 to 0.82; P = 0.013), respectively [87, 88]. Bolland et al. have reported that women who took 1000 mg/day calcium and 400 IU/day vitamin D for 8 years had a 14–20% reduced risk of developing breast cancer, and a 17% reduced risk of developing colorectal cancer [89]. In addition, Bolland suggested that higher doses of Ca plus vitamin D did not decrease cancer incidence when compared with lower doses of Ca plus vitamin D. Conversely, a case-control study involving supplementation of 2303 healthy postmenopausal women (55 years and older) with vitamin D (2000 IU/day) and calcium (1500 IU/day) did not result in a significant decrease in cancer rates over a 4 year period [90]. Collectively, there exsits a possibility that vitamin D and calcium combination therapy may be benefit for cancer prevention. Further research is needed in order to select the right clinical dose in preventing the occurrence of ovarian cancer.
Conclusion
The role of Vitamin D in human cancers, including ovarian cancer, has been widely investigated, where it was proposed to play a protective and antitumorigenic role by regulating cellular proliferation and metabolism. In this review, we have shown that vitamin D status may be an independent predictor of prognosis in ovarian cancer patients.Vitamin D combination therapy improves antitumor effects allowing for potential clinical application. Supplement of vitamin D and calcium combination may be an efficient method for cancer prevention.
Abbreviations
- 1a-OHase:
-
1a-hydroxylase
- 25(OH)D3:
-
25-hydroxyvitamin D3
- 25-OHases:
-
25-hydroxylases
- 7-DHC:
-
7-dehydrocholesterol
- ACC:
-
Acetyl-CoA carboxylase
- CDK:
-
Cyclin-dependent kinase
- COX-1:
-
Cyclooxygenase 1
- COX-2:
-
Cyclooxygenase 2
- DBP:
-
Vitamin D binding protein
- DMBA:
-
7,12-dimethylbenz[a]anthracene
- EGFR:
-
Epidermal growth factor receptor
- FASN:
-
Fatty acid synthase
- HIF-1:
-
Hypoxia inducible factor-1
- HKII:
-
Hexokinase II
- LDHA:
-
Lactate dehydrogenase A
- PI3K:
-
Phosphatidylinositol-3 kinase
- PKA:
-
Protein kinase A
- PLC:
-
Phospholipase C
- VDR:
-
Vitamin D receptor
- VDRE:
-
Vitamin D-response elements
- VEGFR:
-
Vascular endothelial growth factor
References
Gloss BS, Samimi G. Epigenetic biomarkers in epithelial ovarian cancer. Cancer Lett. 2014;342(2):257–63.
Mirandola L, J Cannon M, Cobos E, Bernardini G, Jenkins MR, Kast WM, et al. Cancer testis antigens: novel biomarkers and targetable proteins for ovarian cancer. Int Rev Immunol. 2011;30(2–3):127–37.
Bouillon R, Carmeliet G, Verlinden L, van Etten E, Verstuyf A, Luderer HF, et al. Vitamin D and human health: lessons from vitamin D receptor null mice. Endocr Rev. 2008;29(6):726–76.
Yin L, Grandi N, Raum E, Haug U, Arndt V, Brenner H. Meta-analysis: circulating vitamin D and ovarian cancer risk. Gynecol Oncol. 2011;121(2):369–75.
Ong J-S, Cuellar-Partida G, Lu Y, Fasching PA, Hein A, Burghaus S, et al. Association of vitamin D levels and risk of ovarian cancer: a Mendelian randomization study. Int J Epidemiol. 2016;45(5):1619–30.
Webb PM, de Fazio A, Protani MM, Ibiebele TI, Nagle CM, Brand AH, et al. Circulating 25-hydroxyvitamin D and survival in women with ovarian cancer. Am J Clin Nutr. 2015;102(1):109–14.
Feldman D, Krishnan AV, Swami S, Giovannucci E, Feldman BJ. The role of vitamin D in reducing cancer risk and progression. Nat Rev Cancer. 2014;14(5):342–57.
King AN, Beer DG, Christensen PJ, Simpson RU, Ramnath N. The vitamin D/CYP24A1 story in cancer. Anti Cancer Agents Med Chem. 2010;10(3):213–24.
Silvagno F, Poma CB, Realmuto C, Ravarino N, Ramella A, Santoro N, et al. Analysis of vitamin D receptor expression and clinical correlations in patients with ovarian cancer. Gynecol Oncol. 2010;119(1):121–4.
Campbell MJ, Trump DL. Vitamin D Receptor Signaling and Cancer. Endocrinol Metab Clin N Am. 2017;46(4):1009–38.
Brenza HL, DeLuca HF. Regulation of 25-hydroxyvitamin D3 1alpha-hydroxylase gene expression by parathyroid hormone and 1,25-dihydroxyvitamin D3. Arch Biochem Biophys. 2000;381(1):143–52.
Deeb KK, Trump DL, Johnson CS. Vitamin D signalling pathways in cancer: potential for anticancer therapeutics. Nat Rev Cancer. 2007;7(9):684–700.
Friedrich M, Rafi L, Mitschele T, Tilgen W, Schmidt W, Reichrath J. Analysis of the vitamin D system in cervical carcinomas, breast cancer and ovarian Cancer. Recent Results Cancer Res. 2003;164:239–46.
Anderson MG, Nakane M, Ruan X, Kroeger PE, Wu-Wong JR. Expression of VDR and CYP24A1 mRNA in human tumors. Cancer Chemother Pharmacol. 2006;57(2):234–40.
Ge N, Chu XM, Xuan YP, Ren DQ, Wang Y, Ma K, et al. Associations between abnormal vitamin D metabolism pathway function and non-small cell lung cancer. Oncol Lett. 2017;14(6):7538–44.
Rodriguez GC, Turbov J, Rosales R, Yoo J, Hunn J, Zappia KJ, et al. Progestins inhibit calcitriol-induced CYP24A1 and synergistically inhibit ovarian cancer cell viability: an opportunity for chemoprevention. Gynecol Oncol. 2016;143(1):159–67.
Brozyna AA, Jozwicki W, Jochymski C, Slominski AT. Decreased expression of CYP27B1 correlates with the increased aggressiveness of ovarian carcinomas. Oncol Rep. 2015;33(2):599–606.
Holick MF. Vitamin D, sunlight and cancer connection. Anti Cancer Agents Med Chem. 2013;13(1):70–82.
Lefkowitz ES, Garland CF. Sunlight, vitamin D, and ovarian cancer mortality rates in US women. Int J Epidemiol. 1994;23(6):1133–6.
Fedirko V, Riboli E, Tjonneland A, Ferrari P, Olsen A, Bueno-de-Mesquita HB, et al. Prediagnostic 25-hydroxyvitamin D, VDR and CASR polymorphisms, and survival in patients with colorectal cancer in western European ppulations. Cancer Epidemiol Biomark Prev. 2012;21(4):582–93.
Gong C, Long Z, Yu Y, Zhu L, Tian J, Li S, et al. Dietary factors and polymorphisms in vitamin D metabolism genes: the risk and prognosis of colorectal cancer in Northeast China. Sci Rep. 2017;7(1):8827.
Zhu Y, Wang PP, Zhai G, Bapat B, Savas S, Woodrow JR, et al. Vitamin D receptor and calcium-sensing receptor polymorphisms and colorectal cancer survival in the Newfoundland population. Br J Cancer. 2017;117(6):898–906.
Garland CF, Mohr SB, Gorham ED, Grant WB, Garland FC. Role of ultraviolet B irradiance and vitamin D in prevention of ovarian cancer. Am J Prev Med. 2006;31(6):512–4.
Boscoe FP, Schymura MJ. Solar ultraviolet-B exposure and cancer incidence and mortality in the United States, 1993–2002. BMC Cancer. 2006;6:264.
Tran B, Jordan SJ, Lucas R, Webb PM, Neale R. Association between ambient ultraviolet radiation and risk of epithelial ovarian cancer. Cancer Prev Res (Phila). 2012;5(11):1330–6.
Lin SW, Wheeler DC, Park Y, Cahoon EK, Hollenbeck AR, Freedman DM, et al. Prospective study of ultraviolet radiation exposure and risk of cancer in the United States. Int J Cancer. 2012;131(6):E1015–23.
Lurie G, Wilkens LR, Thompson PJ, McDuffie KE, Carney ME, Terada KY, et al. Vitamin D receptor gene polymorphisms and epithelial ovarian cancer risk. Cancer Epidemiol Biomark Prev. 2007;16(12):2566–71.
Lurie G, Wilkens LR, Thompson PJ, Carney ME, Palmieri RT, Pharoah PD, et al. Vitamin D receptor rs2228570 polymorphism and invasive ovarian carcinoma risk: pooled analysis in five studies within the ovarian cancer association consortium. Int J Cancer. 2011;128(4):936–43.
Tworoger SS, Gates MA, Lee IM, Buring JE, Titus-Ernstoff L, Cramer D, et al. Polymorphisms in the vitamin D receptor and risk of ovarian cancer in four studies. Cancer Res. 2009;69(5):1885–91.
Mohapatra S, Saxena A, Gandhi G, Koner BC, Ray PC. Vitamin D and VDR gene polymorphism (FokI) in epithelial ovarian cancer in Indian population. J Ovarian Res. 2013;6(1):37.
Liu Y, Li C, Chen P, Li X, Li M, Guo H, et al. Polymorphisms in the vitamin D receptor (VDR) and the risk of ovarian cancer: a meta-analysis. PLoS One. 2013;8(6):e66716.
Jurutka PW, Whitfield GK, Hsieh JC, Hompson PD, Haussler CA, Haussler MR. Molecular nature of the vitamin D receptor and its role in regulation of gene expression. Rev Endocr Metab Disord. 2001;2(2):203–16.
Qin X, Lu Y, Qin A, Chen Z, Peng Q, Deng Y, et al. Vitamin D receptor BsmI polymorphism and ovarian cancer risk: a meta-analysis. Int J Gynecol Cancer. 2013;23(7):1178–83.
Grant DJ, Hoyo C, Akushevich L, Iversen ES, Whitaker R, Marks J, et al. Vitamin D receptor (VDR) polymorphisms and risk of ovarian cancer in Caucasian and African American women. Gynecol Oncol. 2013;129(1):173–8.
Prescott J, Bertrand KA, Reid BM, Permuth-Wey J, De Vivo I, Cramer DW, et al. Evidence of differential effects of vitamin d receptor variants on epithelial ovarian cancer risk by predicted vitamin d status. Front Oncol. 2014;4:286.
Trump DL, Hershberger PA, Bernardi RJ, Ahmed S, Muindi J, Fakih M, et al. Anti-tumor activity of calcitriol: pre-clinical and clinical studies. J Steroid Biochem Mol Biol. 2004;89-90(1–5):519–26.
Uitterlinden AG, Fang Y, Van Meurs JB, Pols HA, Van Leeuwen JP. Genetics and biology of vitamin D receptor polymorphisms. Gene. 2004;338(2):143–56.
Colin EM, Weel AE, Uitterlinden AG, Buurman CJ, Birkenhager JC, Pols HA, et al. Consequences of vitamin D receptor gene polymorphisms for growth inhibition of cultured human peripheral blood mononuclear cells by 1, 25-dihydroxyvitamin D3. Clin Endocrinol. 2000;52(2):211–6.
van Etten E, Verlinden L, Giulietti A, Ramos-Lopez E, Branisteanu DD, Ferrira GB, et al. The vitamin D receptor gene FokI polymorphism: functional impact on the immune system. Eur J Immunol. 2007;37(2):395–405.
Campbell MJ, Gombart AF, Kwok SH, Park S, Koeffler HP. The anti-proliferative effects of 1a,25(OH)2D3 on breast and prostate cancer cells are associated with induction of BRCA1 gene expression. Oncogene. 2000;19(44):5091–7.
Reichrath J, Reichrath S, Heyne K, Vogt T, Roemer K. Tumor suppression in skin and other tissues via cross-talk between vitamin D- and p53-signaling. Front Physiol. 2014;5:166.
Semenza GL. HIF-1: upstream and downstream of cancer metabolism. Curr Opin Genet Dev. 2010;20(1):51–6.
Salehi-Tabar R, Nguyen-Yamamoto L, Tavera-Mendoza LE, Quail T, Dimitrov V, An BS, et al. Vitamin D receptor as a master regulator of the c-MYC/MXD1 network. Proc Natl Acad Sci U S A. 2012;109(46):18827–32.
Jiang F, Li P, Fornace AJ, Nicosia SV, Bai W. G2/M arrest by 1,25-dihydroxyvitamin D3 in ovarian cancer cells mediated through the induction of GADD45 via an exonic enhancer. J Biol Chem. 2003;278(48):48030–40.
Zhang X, Jiang F, Li P, Li C, Ma Q, Nicosia SV, et al. Growth suppression of ovarian cancer xenografts in nude mice by vitamin D analogue EB1089. Clin Cancer Res. 2005;11(1):323–8.
Li P, Li C, Zhao X, Zhang X, Nicosia SV, Bai W. p27Kip1 stabilization and G1 arrest by 1,25-dihydroxyvitamin D3 in ovarian cancer cells mediated through down-regulation of cyclin E/cyclin-dependent kinase 2 and Skp1-Cullin-F-box protein/Skp2 ubiquitin ligase. J Biol Chem. 2004;279(24):25260–7.
Shen Z, Zhang X, Tang J, Kasiappan R, Jinwal U, Li P, et al. The coupling of epidermal growth factor receptor down regulation by 1alpha,25-dihydroxyvitamin D3 to the hormone-induced cell cycle arrest at the G1-S checkpoint in ovarian cancer cells. Mol Cell Endocrinol. 2011;338(1–2):58–67.
Jiang F, Bao J, Li P, Nicosia SV, Bai W. Induction of ovarian cancer cell apoptosis by 1,25-dihydroxyvitamin D3 through the down-regulation of telomerase. J Biol Chem. 2004;279(51):53213–21.
Kasiappan R, Shen Z, Tse AK, Jinwal U, Tang J, Lungchukiet P, et al. 1,25-dihydroxyvitamin D3 suppresses telomerase expression and human cancer growth through microRNA-498. J Biol Chem. 2012;287(49):41297–309.
Zhang X, Li P, Bao J, Nicosia SV, Wang H, Enkemann SA, et al. Suppression of death receptor-mediated apoptosis by 1,25-dihydroxyvitamin D3 revealed by microarray analysis. J Biol Chem. 2005;280(42):35458–68.
Mantell DJ, Owens PE, Bundred NJ, Mawer EB, Canfield AE. 1 ,25-dihydroxyvitamin D3 inhibits angiogenesis in vitro and in vivo. Circ Res. 2000;87(3):214–20.
Pendas-Franco N, Garcia JM, Pena C, Valle N, Palmer HG, Heinaniemi M, et al. DICKKOPF-4 is induced by TCF/beta-catenin and upregulated in human colon cancer, promotes tumour cell invasion and angiogenesis and is repressed by 1alpha,25-dihydroxyvitamin D3. Oncogene. 2008;27(32):4467–77.
Maj E, Filip-Psurska B, Milczarek M, Psurski M, Kutner A, Wietrzyk J. Vitamin D derivatives potentiate the anticancer and anti-angiogenic activity of tyrosine kinase inhibitors in combination with cytostatic drugs in an A549 non-small cell lung cancer model. Int J Oncol. 2018;52(2):337–66.
Bao BY, Yao J, Lee YF. 1alpha, 25-dihydroxyvitamin D3 suppresses interleukin-8-mediated prostate cancer cell angiogenesis. Carcinogenesis. 2006;27(9):1883–93.
Ben-Shoshan M, Amir S, Dang DT, Dang LH, Weisman Y, Mabjeesh NJ. 1alpha,25-dihydroxyvitamin D3 (Calcitriol) inhibits hypoxia-inducible factor-1/vascular endothelial growth factor pathway in human cancer cells. Mol Cancer Ther. 2007;6(4):1433–9.
Chung I, Han G, Seshadri M, Gillard BM, Yu WD, Foster BA, et al. Role of vitamin D receptor in the antiproliferative effects of calcitriol in tumor-derived endothelial cells and tumor angiogenesis in vivo. Cancer Res. 2009;69(3):967–75.
Lungchukiet P, Sun Y, Kasiappan R, Quarni W, Nicosia SV, Zhang X, et al. Suppression of epithelial ovarian cancer invasion into the omentum by 1alpha,25-dihydroxyvitamin D3 and its receptor. J Steroid Biochem Mol Biol. 2015;148:138–47.
Liu L, Hu Z, Zhang H, Hou Y, Zhang Z, Zhou G, et al. Vitamin D postpones the progression of epithelial ovarian cancer induced by 7, 12-dimethylbenz [a] anthracene both in vitro and in vivo. Onco Targets Ther. 2016;9:2365–75.
Allavena P, Garlanda C, Borrello MG, Sica A, Mantovani A. Pathways connecting inflammation and cancer. Curr Opin Genet Dev. 2008;18(1):3–10.
Mantovani A, Allavena P, Sica A, Balkwill F. Cancer-related inflammation. Nature. 2008;454(7203):436–44.
Autier P, Boniol M, Pizot C, Mullie P. Vitamin D status and ill health: a systematic review. Lancet Diabetes Endocrinol. 2014;2(1):76–89.
Lee JY, Myung SK, Song YS. Prognostic role of cyclooxygenase-2 in epithelial ovarian cancer: a meta-analysis of observational studies. Gynecol Oncol. 2013;129(3):613–9.
Thill M, Woeste A, Reichert K, Fischer D, Rody A, Friedrich M, et al. Vitamin D inhibits ovarian Cancer cell line proliferation in combination with celecoxib and suppresses cyclooxygenase-2 expression. Anticancer Res. 2015;35(2):1197–203.
Santos JM, Khan ZS, Munir MT, Tarafdar K, Rahman SM, Hussain F. Vitamin D3 decreases glycolysis and invasiveness, and increases cellular stiffness in breast cancer cells. J Nutr Biochem. 2017;53:111–20.
Wilmanski T, Buhman K, Donkin SS, Burgess JR, Teegarden D. 1alpha,25-dihydroxyvitamin D inhibits de novo fatty acid synthesis and lipid accumulation in metastatic breast cancer cells through down-regulation of pyruvate carboxylase. J Nutr Biochem. 2017;40:194–200.
Abu El Maaty MA, Alborzinia H, Khan SJ, Buttner M, Wolfl S. 1,25(OH)2D3 disrupts glucose metabolism in prostate cancer cells leading to a truncation of the TCA cycle and inhibition of TXNIP expression. Biochim Biophys Acta. 2017;1864(10):1618–30.
Zhou X, Zheng W, Nagana Gowda GA, Raftery D, Donkin SS, Bequette B, et al. 1,25-Dihydroxyvitamin D inhibits glutamine metabolism in Harvey-ras transformed MCF10A human breast epithelial cell. J Steroid Biochem Mol Biol. 2016;163:147–56.
Li HX, Gao JM, Liang JQ, Xi JM, Fu M, Wu YJ. Vitamin D3 potentiates the growth inhibitory effects of metformin in DU145 human prostate cancer cells mediated by AMPK/mTOR signalling pathway. Clin Exp Pharmacol Physiol. 2015;42(6):711–7.
Bothwell KD, Shaurova T, Merzianu M, Suresh A, Kuriakose MA, Johnson CS, et al. Impact of short-term 1,25-dihydroxyvitamin D3 on the chemopreventive efficacy of erlotinib against oral cancer. Cancer Prev Res. 2015;8(9):765–76.
Bakhshalizadeh S, Amidi F, Shirazi R, Shabani Nashtaei M. Vitamin D3 regulates steroidogenesis in granulosa cells through AMP-activated protein kinase (AMPK) activation in a mouse model of polycystic ovary syndrome. Cell Biochem Funct. 2018;36(4):183–93.
Wang H, Wang JM, Qu H, Wei HL, Ji BL, Yang ZS, et al. In vitro and in vivo inhibition of mTOR by 1,25- dihydroxyvitamin D3 to improve early diabetic nephropathy via the DDIT4/TSC2/mTOR pathway. Endocrine. 2016;54(2):348–59.
Hoyer-Hansen M, Bastholm L, Szyniarowski P, Campanella M, Szabadkai G, Farkas T, et al. Control of macroautophagy by calcium, calmodulin-dependent kinase kinase-beta, and Bcl-2. Mol Cell. 2007;25(2):193–205.
Jia W, Chang B, Sun L, Zhu H, Pang L, Tao L, et al. REDD1 and p-AKT over-expression may predict poor prognosis in ovarian cancer. Int J Clin Exp Pathol. 2014;7(9):5940–9.
Sofer A, Lei K, Johannessen CM, Ellisen LW. Regulation of mTOR and cell growth in response to energy stress by REDD1. Mol Cell Biol. 2005;25(14):5834–45.
Lisse TS, Liu T, Irmler M, Beckers J, Chen H, Adams JS, et al. Gene targeting by the vitamin D response element binding protein reveals a role for vitamin D in osteoblast mTOR signaling. FASEB J. 2011;25(3):937–47.
Jorde R, Sneve M, Emaus N, Figenschau Y, Grimnes G. Cross-sectional and longitudinal relation between serum 25-hydroxyvitamin D and body mass index: the Tromso study. Eur J Nutr. 2010;49(7):401–7.
Kim JH, Kang S, Jung YN, Choi HS. Cholecalciferol inhibits lipid accumulation by regulating early adipogenesis in cultured adipocytes and zebrafish. Biochem Biophys Res Commun. 2016;469(3):646–53.
Tworoger SS, Lee IM, Buring JE, Rosner B, Hollis BW, Hankinson SE. Plasma 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D and risk of incident ovarian cancer. Cancer Epidemiol Biomark Prev. 2007;16(4):783–8.
Zheng W, Danforth KN, Tworoger SS, Goodman MT, Arslan AA, Patel AV, et al. Circulating 25-hydroxyvitamin D and risk of epithelial ovarian cancer: cohort consortium vitamin D pooling project of rarer cancers. Am J Epidemiol. 2010;172(1):70–80.
Horowitz NS, Wright AA. Impact of obesity on chemotherapy management and outcomes in women with gynecologic malignancies. Gynecol Oncol. 2015;138(1):201–6.
Uddin S, Bu R, Ahmed M, Abubaker J, Al-Dayel F, Bavi P, et al. Overexpression of leptin receptor predicts an unfavorable outcome in middle eastern ovarian cancer. Mol Cancer. 2009;8:74.
Kasiappan R, Sun Y, Lungchukiet P, Quarni W, Zhang X, Bai W. Vitamin D suppresses leptin stimulation of cancer growth through microRNA. Cancer Res. 2014;74(21):6194–204.
Zhang Z, Zhang H, Hu Z, Wang P, Wan J, Li B. Synergy of 1,25-dihydroxyvitamin D3 and carboplatin in growth suppression of SKOV-3 cells. Oncol Lett. 2014;8(3):1348–54.
Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, Heaney RP, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911–30.
Qin B, Moorman PG, Alberg AJ, Barnholtz-Sloan JS, Bondy M, Cote ML, et al. Dairy, calcium, vitamin D and ovarian cancer risk in African-American women. Br J Cancer. 2016;115(9):1122–30.
Trivedi DP, Doll R, Khaw KT. Effect of four monthly oral vitamin D3 (cholecalciferol) supplementation on fractures and mortality in men and women living in the community: randomised double blind controlled trial. BMJ. 2003;326(7387):469.
Lappe JM, Travers-Gustafson D, Davies KM, Recher RR, Heaney RP. Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin Nutr. 2007;85(6):1586–91.
Moukayed M, Grant WB. Molecular link between vitamin D and cancer prevention. Nutrients. 2013;5(10):3993–4021.
Bolland MJ, Grey A, Gamble GD, Reid IR. Calcium and vitamin D supplements and health outcomes: a reanalysis of the Women's Health Initiative (WHI) limited-access data set. Am J Clin Nutr. 2011;94(4):1144–9.
Lappe J, Watson P, Travers-Gustafson D, Recker R, Garland C, Gorham E, et al. Effect of vitamin D and calcium supplementation on cancer incidence in older women: a randomized clinical trial. JAMA. 2017;317(12):1234–43.
Funding
This work was supported by the National Natural Science Fundation of China to Dr. Xiugui Sheng(No.81672591).
Author information
Authors and Affiliations
Contributions
GH and GJ performed literature review and wrote the manuscript. XW contributed critical discussion about the study. YL and SX designed the review. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors agree to the submission of this article for publication.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Supplemental Methods. (DOCX 85 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Guo, H., Guo, J., Xie, W. et al. The role of vitamin D in ovarian cancer: epidemiology, molecular mechanism and prevention. J Ovarian Res 11, 71 (2018). https://doi.org/10.1186/s13048-018-0443-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13048-018-0443-7