Abstract
Background
IVF cycles which result in only one good quality embryo, and a second poor quality embryo present a dilemma when the decision involves transferring two embryos. The aim of this study was to evaluate whether a poor quality embryo has a negative effect on a good quality embryo when transferred along with a good quality embryo.
Methods
We retrospectively evaluated in vitro fertilization (IVF) cycles involving single embryo transfers (SET) and double embryo transfers (DET). Embryo quality was divided into poor “P” and good “G” quality. The main outcome measures were: live birth, implantation rate, miscarriage rate, clinical pregnancy rate and multiple pregnancy ratio.
Results
Six hundred three women were included. The study group consisted of 180 (29.9%) patients who had a double embryo transfer (DET) with one poor quality embryo and one good quality embryo (P + G). Control 1 group included 303 (50.2%) patients who had DET with two good quality embryos (G + G), and control 2 group consisted of 120 (19.9%) patients who had a single embryo transfer (SET) with one good quality embryo (G). Live birth rates were not significantly different when compared between study groups: 30.8% in the SET group (G), 27.2% in the (G + P) group and 33.7% in the (G + G) group. The SET group had the highest implantation rate (33.9%) compared to the DET groups (21.8% (G + P), 25.4% (G + G)) (P =0.022). The clinical pregnancy rate was 33.3% in the SET group (G), 33.3% in the (G + P) group, and 39.3% in the (G + G) group (P =0.39). The miscarriage rate was comparable in all groups.
Conclusion
A poor quality embryo does not negatively affect a good quality embryo, when transferred together in a double embryo transfer.
Similar content being viewed by others
Background
Embryo quality is one of the main predictors of success in IVF cycles [1, 2]. Many studies have shown a strong association between embryo morphology, implantation, and clinical pregnancy rates. In theory, the poor quality embryo has potential for a successful pregnancy. On the other hand, the poor quality embryo may lead to higher spontaneous abortions and overall decreased clinical pregnancies and live birth rates. A study done by Oron et al. [1] found that clinical pregnancy and live birth rates per transfer were nearly 2-fold higher with the transfer of a single good quality embryo than with the transfer of a poor quality embryo. However, once a clinical pregnancy was achieved, it had a similar chance of reaching live birth as a high quality embryo.
Additionally, it has been shown that double embryo transfers [DET] are associated with higher clinical pregnancy and live birth rates [3, 4], compared to single embryo transfers [SET]. Roberts et al. [3] reported that SETs have a one-third lower live birth rate then DETs in fresh cycles. Baruffi et al. [4] reported that fresh DET cycles have higher ongoing pregnancy and live births rates than SET.
Many IVF centers, therefore, increase the number of embryos transferred when the quality of embryos is decreased at cleavage stage. The potential situation of having only one good quality embryo with the second poor quality embryo presents a dilemma when the decision involves transferring two embryos. Should the poor quality embryo be transferred with the good quality embryo or does it have the potential to harm the implantation and pregnancy rate of the good embryo? A potential interaction exists between preimplantation embryos via paracrine factors, which affect the development and growth of the neighboring embryos [5]. In addition, it has been shown that the presence of poor quality embryos in the same culture decreases the overall blastulation rate of all embryos [6].
The aim of this study was to evaluate whether a poor quality embryo has a negative effect on a good quality embryo when transferred along with a good quality embryo.
Methods
This is a retrospective cohort study encompassing all IVF and IVF ICSI cycles performed in a single university affiliated ART center between 2010-2015. Only cycles involving SET or DET of fresh non-donor oocytes were included. The study was approved by the local ethics committee.
Embryo quality
Cleavage embryos were graded from one to four, based on percent fragmentation and cell counts: grade 4, equal-sized symmetrical cells with no fragmentation and 6-8 cells; grade 3, equal-sized symmetrical cells with less than 10% fragmentation and/or 4-5 cells; grade 2, non-symmetrical blastomers with 10-50% fragmentation, less than 4 cells; and grade 1 more than 50% fragmentation. Embryo quality grading was determined on the day of embryo transfer (day 3 or 5) : embryo quality was divided into poor quality “P” [grade 1 and 2] and good quality “G” [grade 3 and 4]. The study group consisted of patients who had DET with one “G” and one “P” embryos [group 1]. The control groups included; DET with two “G” embryos [control 1] and SET with one “G” embryo [control 2].
On Day 5, embryos were scored for blastocyst formation. Blastocysts were graded according to the size of the blastocyst, the assessment of the ICM and trophectoderm development [≥3BB] [7]. Good quality embryos [Grade 3-4] were defined as those where at least: [3] the blastocele completely fills the embryo (grade 3); the ICM is loosely grouped with several cells (grade B); and the trophoectoderm has very few cells forming a loose epithelium (grade B). Lower than 3BB quality embryos on Day 5 were defined as poor quality embryos [Grade 1 or 2]. The allocation to blastocyst versus cleavage transfer was based on the number and quality of cleavage embryos available on day 3. Blastocyst grading was performed by two trained embryologists, each with over 15 years of experience.
Pregnancy diagnosis; A quantitative pregnancy test [serum β-HCG] was taken 14 days after HCG administration. In case of a positive pregnancy test, a transvaginal ultrasound was performed 28-32 days after the embryo transfer and repeated as required. Clinical pregnancy was confirmed if a fetal heartbeat was observed by transvaginal ultrasound.
Statistical analysis
Primary outcome measure was defined as live birth. Secondary outcome measures of the study were implantation rate, miscarriage rate, clinical pregnancy rate and multiple pregnancy ratio.
Analysis of data was performed using the SPSS 23.0 computer package [SPSS Inc., Chicago, IL]. Normally distributed data were analyzed by ANOVA. χ 2 or Fisher’s exact test were used for comparisons of rates and proportions. All P values were tested as two-sided and considered significant at less than 0.05.
A multivariate logistic regression model for clinical pregnancy was performed using the following variables: maternal age, paternal age, BMI, day 3 baseline FSH levels, E2 [estradiol] level on HCG day, embryo transfer day, cycle sequential number, and treatment group.
Results
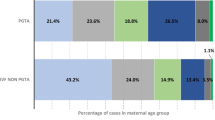
A total of 603 women were included in the study. 180 women had DET with one poor quality embryo and one good quality embryo [group 1(G + P)], 303 women had DET with two good quality embryos [control 1(G + G)], and 120 women had SET with one good quality embryo [control 2(G)]. The demographic characteristics are presented in Table 1. The patients in the SET group (control 2) were significantly younger and presented a significantly lower BMI compared to those of DET (group 1 and control 1; Table 1). Baseline FSH values showed a difference when compared across the groups (Table 1) though not clinically significant. The groups were comparable in gravity, parity, and etiology of infertility (Table 1). The cycle characteristics are presented in Table 2. E2 level on the day of hCG, number of oocytes retrieved, and fertilization rates were significantly higher in control 1 (G + G). The treatment outcome of all three groups is shown in Table 3. The implantation rates were significantly different between the three treatment groups; both control groups had a higher implantation rate compared to the study group. Despite this difference, the other main outcome measures (live birth, and clinical pregnancy rates, as well as the other outcome variables) were comparable between these groups. No difference in twinning rates was identified when comparing the two double transfer groups, while no cases of twins were registered in the SET group.
Due to the mentioned demographic and cycle dynamic differences between the groups, and in order to treat possible confounders, we designed a multivariate logistic regression model for live birth incorporating the following variables: maternal age, paternal age, BMI, day 3 baseline FSH levels, E2 level on HCG day, embryo transfer day [cleavage versus blastocyst], and treatment group (the number of picked ova was not included due to co-linearity with the maximal E2 levels). The treatment group was not found to be significantly related to the main outcome measure (OR 0.915, 95% CI 0.64-1.307, P value 0.625), neither was any of the other tested variables in the model (Additional file 1).
Discussion
Our study was designed to question a common issue in the clinical practice of physicians dealing with IVF. What should we do with a poor quality embryo? If the decision is SET, than a good quality embryo has a higher chance to achieve pregnancy, though the poor quality embryo still has a chance for pregnancy [1]. If the decision is DET, and the option is combining a good quality embryo with a poor quality embryo, the concern is that the poor quality embryo can potentially harm the good one. Our cohort demonstrated, that the live birth rates were similar when a poor quality embryo was transferred along with a good quality embryo, when compared to both a single good quality embryo transferred on its own or to two good quality embryos transferred together. Therefore, the decision to transfer a poor quality embryo with a good quality embryo did not lower the chances for women to conceive and importantly, did not affect her chances for live birth. Conversely, it did not increase the chance either. The twin pregnancy rate of 9.5% in the study group shows that at least some of the embryos which were classified as poor were implanted and lead to a viable pregnancy. Interestingly, the implantation rate of the SET was higher compared to both DET groups. This may be due to the significantly younger age and lower BMI in the SET group vs the DET groups, yet the results did not change even after adjusting for these confounding factors.
Our results contradict a recent study performed by El-danasouri et al. [8], who found that transferring an impaired quality embryo along with a good quality embryo significantly lowered both the pregnancy and implantation rates, than transferring the good quality embryo alone.
Our findings did not change, even after adjusting for confounding factors such as maternal age, paternal age, BMI, day 3 baseline FSH levels, E2 level on HCG day and stage of the embryo. Additionally, miscarriage rates were similar in all groups. This is similar to other studies [1] which have shown that once a clinical pregnancy was achieved with poor quality embryo, it had a similar chance of reaching live birth as a high quality embryo. When choosing end-points for future studies, clinical pregnancy should be sufficient as we showed.
The crude live birth rate, and twin gestation rate were highest in the DET with two good quality embryos. Overall the twin live birth rate was 10.6% (G + G) vs 9.5% (G + P) vs 0% (G). Multiple pregnancies are high-risk pregnancies, and should be avoided if possible [9]. Based on our results, embryo transfers with one good and one poor quality embryo yielded higher multiple pregnancy rates than one good quality SET. In a case when a single embryo pregnancy is mandatory, the G + P option should also be avoided.
Our study results are somewhat limited by the way the embryos were graded. Despite technological advances, current morphological assessment of the embryo, even when performed by experienced embryologists, is subjective. This might partially explain our result regarding the pregnancy rate with poor quality embryos. Perhaps more advanced methods to evaluate embryos, such as time lapse and genetic screening or pre-gestational screening (PGS) [10, 11] will provide a better definition of good and poor quality embryos and help to better predict viable pregnancies.
Other limitations include the retrospective design. Ideally, a prospective randomized trial, which includes only patients who are candidates for DET and have only one good quality and one poor quality embryo, should be performed. However, this study would take a long time and would be very difficult to recruit patients who are undergoing DET to instead perform SET with only one good quality embryo. Given that, as far as we know, there is no clear data in the literature studied, we tried to reduce biases by creating two control groups.
According to our results, single embryo transfers (SET) should be the initial recommendation for patients. When good quality embryos are transferred, the implantation rate is higher and there is no difference in pregnancy rate. Double embryo transfers should be limited to patients with repeated implantation failure or repeated pregnancy loss. Yet, when two embryos are transferred, women can be reassured that the quality of the second embryo does not seem to affect the pregnancy rate or the risk of twin pregnancy.
Conclusion
Based on our findings, a poor quality embryo does not negatively affect a good quality embryo, when transferred together in a double embryo transfer.
Abbreviations
- DET:
-
Double embryo transfers
- SET:
-
Single embryo transfers
- IVF:
-
In vitro fertilization
- “P”:
-
Poor quality embryo
- “G”:
-
Good quality embryo
References
Oron G, Son WY, Buckett W, Tulandi T, Holzner H. The association between embryo quality and perinatal outcome of singletons born after single embryo transfers: a pilot study. Hum Reprod. 2014;29:1444–51.
Zhu J, Lian Y, Li M, Chen L, Liu P, Qiao J. Does IVF cleavage stage embryo quality affect pregnancy complications and neonatal outcomes in singelton gestations after double embryo transfers. J Assist Reprod Genet. 2014;31:1635–41.
Roberts SA, McGowan L, Hirst WM, Vail A, Rutherford A, Lieberman BA, Brison DR. Reducing the incidence of twins from IVF treatments: Predictive modeling from a retrospective cohort. Human Reprod. 2011;26:569–75.
Baruffi RL, Mauri AL, Petersen CG, Nicoletti A, Pontes A, Oliveura JB, Franco Jr JG. Single-embryo transfer reduces clinical pregnancy rates and live births in fresh IVF and inracytoplasmic sperm injection (ICSI) cycles. A meta-analysis. Reprod Biol Endocrinol. 2009;7:36.
Paria BC, Dey SK. Preimplantation embryo development in-vitro: cooperative interactions among embryos and the role of growth factors. Proc Natl Acad Sci U S A. 1990;81:4756–60.
Tao T, Robichaud A, Mercier J, Ouellette R. Influence of group embryo culture strategies on the blastocyst developmentand pregnancy outcome. J Assist Reprod Genet. 2013;30:63–8.
Gardner DK, Surrey E, Minjarez D, Leitz A, Stevens J, Schoolcraft WB. Single blastocyst transfer: a prospective randomized trial. Fertil Steril. 2004;81:551–5.
El-danasouri I, Sterzik K, Rinaldi L, Pacchiarotti A, Desanto M, Selman H. Effect of transferring a morphologically impaired embryo with a good quality embryo on the pregnancy and implantation rates. Eur Rev Med Pharmacol Sci. 2016;20:394–8.
Guerif F, Frapsauce C, Chavez C, Cadoret V, Royere D. Treating women under 30 years old without top quality embryos on day 2: a prospective study comparing double embryo transfer with single blastocyst transfer. Hum Reprod. 2011;26:775–81.
Yanez LZ, Han J, Behr BB, Reijo Pera RA, Camarillo DB. Human oocyte developmental potential is predicted by mechanical properties within hours after fertilization. Nat Commun. 2016;Article number:10809.
Haikin Herzberger E, Ghetler Y, Tamir Yaniv R, Berkovitz A, Gonen O, Cohen I, Shulman A, Wiser A. Time lapse microscopy is useful for elective single-embryo transfer. Gynecol Endocrinol. 2016;26:1–3.
Acknowledgements
Not applicable.
Funding
This research did not receive financial support.
Availability of data and materials
Please contact author for data requests.
Authors’ contribution
EMW participation in study design, execution, analysis, manuscript drafting and final approval of version to be published. AHK participation in analysis, manuscript drafting, final approval of version to be published. KT participation in execution and interpretation of data, manuscript revising and final approval of version to be published. YG participation in execution, manuscript revising and final approval of version to be published. OG participation in execution and interpretation of data, manuscript revising and final approval of version to be published. OW participation in execution and interpretation of data, manuscript revising and final approval of version to be published. AS participation in study design, execution, manuscript revising and final approval of version to be published. AW participation in study design, execution, analysis, manuscript drafting and final approval of version to be published.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study was approved by the local ethics committee of Meir Medical Center.
Condensation
A poor quality embryo does not negatively affect a good quality embryo, when transferred together in a double embryo transfer.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Table S1.
Regression model for live birth rate. (DOC 35 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Wintner, E.M., Hershko-Klement, A., Tzadikevitch, K. et al. Does the transfer of a poor quality embryo together with a good quality embryo affect the In Vitro Fertilization (IVF) outcome?. J Ovarian Res 10, 2 (2017). https://doi.org/10.1186/s13048-016-0297-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13048-016-0297-9