Abstract
Background
In our previous SMC NB-2004 study of patients with high-risk neuroblastomas, which incorporated total-body irradiation (TBI) with second high-dose chemotherapy and autologous stem cell transplantation (HDCT/auto-SCT), the survival rate was encouraging; however, short- and long-term toxicities were significant. In the present SMC NB-2009 study, only TBI was replaced with 131I-meta-iodobenzylguanidine (MIBG) treatment in order to reduce toxicities.
Methods
From January 2009 to December 2013, 54 consecutive patients were assigned to receive tandem HDCT/auto-SCT after nine cycles of induction chemotherapy. The CEC (carboplatin + etoposide + cyclophosphamide) regimen and the TM (thiotepa + melphalan) regimen with (for metastatic MIBG avid tumors) or without (for localized or MIBG non-avid tumors) 131I-MIBG treatment (18 or 12 mCi/kg) were used for tandem HDCT/auto-SCT. Local radiotherapy, differentiation therapy with 13-cis-retinoic acid, and immunotherapy with interleukin-2 were administered after tandem HDCT/auto-SCT.
Results
Fifty-two patients underwent the first HDCT/auto-SCT and 47 patients completed tandem HDCT/auto-SCT. There was no significant immediate toxicity during the 131I-MIBG infusion. Acute toxicities during the tandem HDCT/auto-SCT were less severe in the NB-2009 study than in the NB-2004 study. Late effects such as growth hormone deficiency, cataracts, and glomerulopathy evaluated at 3 years after the second HDCT/auto-SCT were also less significant in the NB-2009 study than in NB-2004 study. There was no difference in the 5-year event-free survival (EFS) between the two studies (67.5 ± 6.7% versus 58.3 ± 6.9%, P = 0.340).
Conclusions
Incorporation of high-dose 131I-MIBG treatment into tandem HDCT/auto-SCT could reduce short- and long-term toxicities associated with TBI, without jeopardizing the survival rate.
Trial registration
ClinicalTrials.gov NCT03061656
Similar content being viewed by others
Background
Although the outcome of high-risk neuroblastoma has improved after the introduction of high-dose chemotherapy and autologous stem cell transplantation (HDCT/auto-SCT), the outcome was still unsatisfactory [1,2,3,4]. In recent multicenter clinical trials of HDCT/auto-SCT, the 3- or 5-year event-free survival (EFS) was reported to be 40–50% [5, 6]. The main cause of treatment failure after HDCT/auto-SCT is relapse or tumor progression rather than treatment-related mortality (TRM). In this context, the role of tandem HDCT/auto-SCT has been investigated with the hypothesis that a sequential course of HDCT/auto-SCT might further improve the survival of high-risk neuroblastoma and encouraging survival rates have been reported [7,8,9]. However, further dose escalation and the addition of more drugs during tandem HDCT/auto-SCT might be associated with more significant short- and long-term toxicities than single HDCT/auto-SCT. Therefore, a strategy to minimize toxicities during or after tandem HDCT/auto-SCT is important for better outcomes.
We previously reported the results of a single-arm prospective trial (SMC NB-2004 study) using tandem HDCT/auto-SCT for high-risk neuroblastoma [10], which was designed based on the results of retrospective analysis of our early experience between the late 1990s and early 2000s [7]. In the NB-2004 study, nine cycles of induction chemotherapy were administered before tandem HDCT/auto-SCT, and total-body irradiation (TBI) was incorporated into the second HDCT/auto-SCT. As a result, survival rates were very encouraging; however, short- and long-term toxicities associated with tandem HDCT/auto-SCT, particularly TBI, were severe.
Around 90% of neuroblastomas express the norepinephrine transporter that facilitates uptake of radiolabeled metaiodobenzylguanidine (MIBG), suggesting a rationale for employing radiolabeled MIBG as a targeted radiotherapy [11, 12]. The safety and efficacy of 131I-MIBG treatment has been reported in previous studies that were performed mainly on relapsed or refractory neuroblastoma patients [13,14,15,16,17]. Therefore, we conducted a new prospective trial (SMC NB-2009 study), in which only TBI in the second HDCT/auto-SCT of NB-2004 study was replaced with high-dose 131I-MIBG treatment to reduce short- and long-term toxicities, without jeopardizing the survival rate. Otherwise, all treatments including induction treatment, the first HDCT and the post-HDCT/auto-SCT treatment in the NB-2009 study were the same as those in the NB-2004 study.
Methods
Patients
From January 2009 to December 2013, patients who were newly diagnosed with high-risk neuroblastoma were enrolled. Patients older than 1 year with International Neuroblastoma Staging System (INSS) stage 4 and patients with MYCN proto-oncogene bHLH transcription factor (MYCN) amplified tumors regardless of stage were both categorized as high-risk patients. Tumor extent was evaluated using computed tomography/magnetic resonance imaging, a technetium-99 (99Tc) bone scan, bilateral bone marrow examination, an 123I-MIBG scan, and 18F-fluorodeoxy-d-glucose positron emission tomography (PET)/computed tomography. Tumor staging was determined according to the INSS [18]. The International Neuroblastoma Pathology Classification (INPC) system was used in the pathologic classification of tumors [19], and MYCN amplification was determined using interphase fluorescence in situ hybridization on tumor tissues. MYCN amplification was defined as a greater than fourfold increase of the MYCN signal number relative to the number of control probe signals [20].
Induction treatment
Induction treatments were the same as those in the SMC NB-2004 study [10]. Briefly, nine cycles of chemotherapy were administered during induction treatment. The CEDC (cisplatin + etoposide + doxorubicin + cyclophosphamide) and ICE (ifosfamide + carboplatin + etoposide) regimens were used alternatively (Table 1). Each cycle of induction chemotherapy was performed at 4-week intervals, and delays were permitted to allow the absolute neutrophil count to recover to 1.0 × 109/L and the platelet count to 100 × 109/L. Surgery was usually performed after six cycles of chemotherapy, except when complete excision was possible at diagnosis. The extent of surgery was resection of the primary tumor along with accessible regional lymph nodes. Peripheral blood stem cells (PBSCs) were collected during the recovery phase of the seventh chemotherapy cycle. The minimum target number of CD34+ cells was 2.0 × 106/kg.
Tandem HDCT/auto-SCT
HDCT regimens were also the same as in the NB-2004 study [10], except that TBI (3.33 Gy/day on days −3, −2, −1) in the second HDCT/auto-SCT was replaced with 131I-MIBG treatment in the NB-2009 study (Table 1). CEC (carboplatin + etoposide + cyclophosphamide) and TM (thiotepa + melphalan) with 131I-MIBG treatment were used as the first and second HDCT regimen, respectively. During the first year of the study, the dose of 131I-MIBG treatment was 18 mCi/kg (maximum 500 mCi), but it was reduced to 12 mCi/kg (maximum 500 mCi) during the remaining study period in fear of late adverse effects of high-dose 131I-MIBG treatment. 131I-MIBG was infused on day −21 of the second HDCT/auto-SCT. For patients with MIBG non-avid or localized tumors, 131I-MIBG treatment was not administered; instead, the dose of thiotepa was increased to 300 mg/m2/day. The interval between the first and second HDCT/auto-SCT was set to be 12 ± 1 weeks in order to reduce toxicities in the second HDCT/auto-SCT. However, some delay was allowed when there was a problem in the 131I-MIBG supply or scheduling the transplantation unit. Approximately half of the PBSCs collected were infused for bone marrow rescue at each HDCT/auto-SCT session, and the minimum number of CD34+ cells was 1.0 × 106/kg.
Post-HDCT/auto-SCT treatment
Treatments after tandem HDCT/auto-SCT were also the same in the NB-2004 study [10]. Briefly, local radiotherapy (RT) to the site of the primary tumor (15 Gy/1.5 Gy for complete resection of the primary tumor and 21.6 Gy/1.8 Gy or 30.6 Gy/1.8 Gy for incomplete resection according to the residual 123I-MIBG or PET uptake) was administered to all patients approximately 6 weeks after the second HDCT/auto-SCT. RT was not administered to the residual metastatic sites. Differentiation therapy with 13-cis-retinoic acid (125 mg/m2/day for 14 days every 4 weeks) and immunotherapy with IL-2 (2 × 106 U/m2/day, subcutaneous injection for five consecutive days every 4 weeks) were started at approximately 9 weeks after the second HDCT/auto-SCT and continued until a year after the second HDCT/auto-SCT.
Response criteria
Response was evaluated every three cycles of induction chemotherapy, before the first and second HDCT/auto-SCT, every 3 months for the first year after the second HDCT/auto-SCT, every 4 months for the second year, every 6 months for the third year, and every year thereafter. Basically, International response criteria for neuroblastoma were used to evaluate the treatment response [18]. CT/MRI, 99Tc- bone scan, 123I-MIBG scan, and bilateral bone marrow examinations were routinely performed to determine the response at primary and metastatic sites. The results of the 123I-MIBG scan and bone marrow examination were also integrated into the response assessment of metastatic sites according to the international response criteria. Briefly, a complete response (CR) was defined as no identifiable tumor with normal catecholamine. A very good partial response (VGPR) was defined as a reduction of the primary tumor by 90–99% with normal catecholamine with or without any residual 99Tc bone changes. A partial response (PR) was defined as a reduction of the primary tumor and metastatic tumor by >50%. A mixed response (MR) was defined as a reduction of any measurable lesion by >50% with a reduction of any other lesion by <50%. Stable disease (SD) was defined as no new lesion and an increase in any existing lesion by <25%. Progressive disease (PD) was defined as any new lesion or increase of any measurable lesion by >25%.
Evaluation of late adverse effects
Cardiac, renal, respiratory, endocrine, auditory, and ophthalmologic functions were evaluated 1, 3, and 5 years after the second HDCT/auto-SCT. Respiratory function was assessed by clinical signs and symptoms in all patients, and a pulmonary function test was performed if the patient could cooperate with the test. Neurocognitive functions were evaluated 3 years after the second HDCT/auto-SCT using the Korean-Wechsler Preschool and Primary Scale of Intelligence (<6 years of age) or the Korean version of the Wechsler Intelligence Scale for children-III (≥6 years of age). Toxicities were recorded according to the Common Terminology Criteria for Adverse Events (version 4.0) of the US National Cancer Institute.
Survival analysis and statistics
Differences in categorical variables were measured by the chi-square test or Fisher’s exact test, and differences in continuous variables were calculated with the Mann-Whitney U test. EFS was calculated from the date of diagnosis until the date of relapse, progression, secondary malignancy, or death, whichever occurred first. Overall survival (OS) was calculated from the date of diagnosis until death from any cause. Survival rates and standard errors were estimated using the Kaplan-Meier method. Differences in survival rates between the two groups were compared using the log-rank test. P values <0.05 were considered significant.
Results
Patient characteristics
A total of 54 consecutive patients were enrolled, and the patient’s characteristics are summarized in Table 2. The median age at diagnosis was 30.5 (range, 1–231) months, and 45 (83.3%) of patients were older than 18 months. Fifty-two (96.3%) patients had metastatic tumors and 25 (48.1%) patients had MYCN-amplified tumors. While two patients with stage 4, MYCN non-amplified tumors in the NB-2004 study who were aged between 12 and 18 months were not classified in the high-risk group according to the International Neuroblastoma Risk Group classification [21], there was no such patient in the NB-2009 study. Otherwise, there was no significant difference in the clinical and biological characteristics of the patients between the NB-2004 and NB-2009 studies.
Induction treatment
Neutropenic fever was experienced by all patients during induction treatment; however, non-hematologic toxicity was not significant (Table 3). Surgery was performed before initiation of induction chemotherapy in eight patients; however, in 42 patients, it was deferred until after six (n = 40) or more (n = 2) cycles of induction chemotherapy. In the remaining four patients, surgery was not performed because the tumor disappeared during induction treatment (n = 1), was still unresectable after induction treatment (n = 2), or progressed before surgery (n = 1). Two patients experienced PD during induction treatment and died despite salvage treatment.
Tandem HDCT/auto-SCT
Fifty-two patients proceeded to the first HDCT/auto-SCT, and their tumor statuses at the first HDCT/auto-SCT were CR in 29 (53.7%), VGPR in 10 (18.5%), PR in 11 (20.4%), MR in one (1.9%), and SD in one (1.9%).
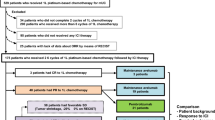
Figure 1 shows the patient flow. Five of 52 patients who underwent the first HDCT/auto-SCT died from TRM (myocarditis in three, hepatic veno-occlusive disease in one, and intracranial hemorrhage in one) during the first HDCT/auto-SCT. Therefore, 47 patients could proceed to the second HDCT/auto-SCT. Forty-three patients received 131I-MIBG treatment (18 mCi/kg in five patients and 12 mCi/kg in 38 patients), and the remaining four patients with a localized tumor (n = 2) or a MIBG non-avid tumor (n = 2) underwent the second HDCT/auto-SCT without 131I-MIBG treatment. The median interval from day 0 of the first HDCT/auto-SCT to initiation of the second HDCT/auto-SCT was 87 days (range 79–139). The interval was within 12 ± 1 weeks in 36 (76.6%) patients and was less than 14 weeks in 45 (95.7%) patients.
Table 4 lists hematologic and non-hematologic toxicities of grade ≥3 that developed within 1 month of each HDCT/auto-SCT. Hematologic recovery was rapid in both the first and second HDCT/auto-SCT, although platelet recovery was delayed in the second HDCT/auto-SCT compared to the first (P = 0.004). The grade ≥3 non-hematologic toxicities that developed in more than 30% of patients were diarrhea, an elevation of liver enzymes and hypokalemia in the first HDCT/auto-SCT, and stomatitis and diarrhea in the second HDCT/auto-SCT. No acute complications occurred during or shortly after the infusion of 131I-MIBG. In the comparison of toxicities during the second HDCT/auto-SCT between the TM-TBI regimen in the NB-2004 study (n = 42) and the 131I-MIBG-TM regimen in the NB-2009 study (n = 43), hematologic recovery was faster and duration of fever was shorter in the NB-2009 study than in the NB-2004 study (P = 0.038 for ANC recovery and P = 0.041 for platelet recovery). In addition, the frequency of stomatitis, elevation of liver enzymes, and hypokalemia was lower in the NB-2009 study than in the NB-2004 study (P = 0.003, 0.030, and <0.001, respectively). Acute toxicities that occurred more than 1 month after HDCT/auto-SCT were cytomegalovirus disease in two patients and Pneumocystis jirovecii pneumonia in one patient, but they all improved after treatment.
Relapse and survival
Tumor relapse or progression occurred in 15 (27.8%) patients (two during induction treatment and 13 after the second HDCT/auto-SCT), and eight (14.8%) of them died despite salvage treatment. All 13 relapse/progressions after tandem HDCT/auto-SCT occurred at metastatic sites (bone in seven, brain/dura in five, bone marrow in four, and lymph node in two) with (n = 2) or without (n = 11) primary site relapse. Seven patients experienced relapse at multiple sites, and six patients experienced relapse at a single site.
TRM occurred in eight (14.8%) patients: five (9.3%) from acute toxicities, two (3.7%) from chronic lung disease, and one (1.9%) from secondary malignancy. Five patients died from acute toxicities during the first HDCT/auto-SCT as described above. Two of five patients who received 18 mCi/kg of 131I-MIBG treatment died from chronic lung disease at 40 and 79 months from diagnosis, respectively. These two patients were in a CR prior to tandem HDCT/auto-SCT. One patient was diagnosed with myelodysplastic syndrome at 19 months after diagnosis and died. Therefore, 31 out of 54 patients remained event-free with a median follow-up of 65 months (range, 38–96) from diagnosis, and 38 of 54 patients remained alive with a median follow-up of 63 months (range, 38–96) from diagnosis. The 5-year OS and EFS rates after diagnosis were 72.4 ± 6.4% and 58.3 ± 6.9%, respectively (Fig. 2a). There was no difference in EFS between the NB-2004 and NB-2009 studies (P = 0.340, Fig. 2b). When the analysis was confined only to 38 patients with metastatic MIBG avid tumors who received 12 mCi/kg of 131I-MIBG treatments, survival rates were not different from those in the 42 patients who underwent the second HDCT/auto-SCT with the TM-TBI regimen in the NB-2004 study (P = 0.735, Fig. 2c). The EFS rates of patients with CR or VGPR at the first HDCT/auto-SCT were higher than that of patients with PR or worse (5-year EFS, 73.6 ± 7.2% versus 25.0 ± 10.8%, P = 0.004, Fig. 2d).
Survival rates. The 5-year OS and EFS rates after diagnosis were 72.4 ± 6.4% and 58.3 ± 6.9%, respectively (a). There was no difference in EFS between the NB-2004 and NB-2009 studies (b). There was no difference in EFS between the TM-TBI regimen in the NB-2004 study and 12 mCi/kg of 131I-MIBG-TM in the NB-2009 study (c). EFS of patients in CR or VGPR at the first HDCT/auto-SCT was higher than in those patients with PR or worse (d)
Late adverse effects
All 27 patients who remained event-free 3 years after the second HDCT/auto-SCT were evaluated for the presence of various late adverse effects (Table 5). Twenty-three patients had at least 1, 18 had ≥2, and eight had ≥3 late adverse effects. Sensory neural hearing loss, renal tubulopathy, and hypothyroidism were common late adverse effects. Among the 27 patients, 16 patients underwent a pulmonary function test for screening for chronic lung disease. The FEV1 of the patients ranged from 70 to 132% (median 91%) of the expected normal value, and grade 3/4 FEV1 reduction was not observed in any patients. All late adverse effects were grades 1 or 2 except in two patients with sensorineural hearing loss requiring hearing aids. The frequency of growth hormone deficiency, cataracts, and renal glomerulopathy was lower in the NB-2009 study than in the NB-2004 study. The median number of late effects in each patient was 2 (range 0–4), and it was lower than that in the NB-2004 study.
Vertical growth retardation and poor weight gain were less significant in the NB-2009 study than in the NB-2004 study (Fig. 3a, b). Body mass index was not different between the two studies (Fig. 3c). The full-scale intelligence quotient was 86 (range 57–112), and there was no difference between the NB-2004 and NB-2009 studies (Fig. 3d).
Long-term sequelae after tandem HDCT. Vertical growth retardation (a) and poor weight gain (b) was less significant in the NB-2009 study compared to the NB-2004 study. Body mass index was not different between the two studies (c). There was no difference in full-scale intelligence quotient (FSIQ) between the NB-2004 and NB-2009 studies (d)
Discussion
Our previous prospective study (NB-2004 study), which incorporated TBI into the second HDCT/auto-SCT, showed very encouraging survival rates. However, we found that late adverse effects, particularly from TBI, occurred in all long-term survivors. Therefore, we conducted a new prospective trial, which incorporated high-dose 131I-MIBG treatments into the second HDCT/auto-SCT instead of TBI. The survival rates were comparable to those in the NB-2004 study; however, the short- and long-term toxicities were significantly less than in the NB-2009 study.
Several phase I and II clinical trials using 131I-MIBG treatment were conducted in patients with relapsed or refractory neuroblastoma, and the response rates were 30–60% [13,14,15,16,17]. More recently, studies incorporating 131I-MIBG treatments as part of myeloablative therapy have been reported [22,23,24]. However, no studies to date have incorporated high-dose 131I-MIBG treatments into tandem HDCT/auto-SCT for treating newly diagnosed high-risk patients. To the best of our knowledge, the NB-2009 study is the first prospective study that incorporated high-dose 131I-MIBG treatments into tandem HDCT/auto-SCT as a front-line treatment in a substantial number of patients.
Early clinical trials showed that myelosuppression was the main dose-limiting toxicity of 131I-MIBG treatment. Matthay et al. reported that the maximum-tolerated 131I-MIBG dose was 12 mCi/kg for patients without available stem cells, while 18 mCi/kg was tolerable and feasible for patients with available stem cells [16]. The New Approaches to Neuroblastoma Therapy (NANT) consortium conducted a phase I dose escalation study to determine the maximum-tolerated dose and toxicity of 131I-MIBG treatment incorporated into the CEM (carboplatin + etoposide + melphalan) regimen in refractory neuroblastoma patients [23]. The results of the NANT study suggested that the maximal tolerable dose was 12 mCi/kg of 131I-MIBG in the normal renal function cohort. In another study, 131I-MIBG at doses up to 18 mCi/kg could be safely administered 6 weeks prior to a BM (busulfan + melphalan) regimen for refractory neuroblastoma [22]. In the present NB-2009 study, the dose of 131I-MIBG treatment was 18 mCi/kg in the first year of the study, but it was reduced to 12 mCi/kg in the remaining study period out of concern about late adverse effects of 131I-MIBG treatment coupled with tandem HDCT/auto-SCT. Short-term toxicities during the second HDCT/auto-SCT were acceptable. As compared to findings in the NB-2004 study, hematologic recovery was faster and fever duration was shorter. In addition, acute non-hematologic toxicities were tolerable, although mucositis-related toxicities were severe. The frequency of stomatitis, elevation of liver enzymes, and hypokalemia were lower than those in the NB-2004 study. No toxic death occurred during the second HDCT/auto-SCT.
Late adverse effects of the 131I-MIBG treatment were also reported in several studies. Hypothyroidism has been reported in patients who were treated with 131I-MIBG [25, 26]. A secondary malignancy has also been reported after 131I-MIBG treatment [27]. However, the long-term adverse effects could not be evaluated properly because 131I-MIBG treatments were usually used as salvage treatments for patients with relapsed or refractory tumors, and therefore, sufficient follow-up was not possible in most patients. Late adverse effects in the NB-2009 study evaluated at 3 years after tandem HDCT/auto-SCT were generally milder than those in the NB-2004 study. However, two of five patients who received 18 mCi/kg of 131I-MIBG treatment during the first year of the study died from chronic lung disease while there was no death from late toxicities in the 38 patients who received 12 mCi/kg of 131I-MIBG treatment during the remaining study. These findings suggest that 18 mCi/kg of 131I-MIBG treatment might be beyond the maximal tolerable dose when it is coupled with tandem HDCT/auto-SCT.
Survival rates in the NB-2009 study were encouraging and were not different from those in the NB-2004 study. However, many patients still experienced tumor relapse or progression after the tandem HDCT/auto-SCT, particularly poor responders following induction therapy. There was no difference in clinical and biologic factors between the good and poor responders to induction treatment. All relapsed patients experienced metastatic relapse, and these finding suggest that further improvements in treatment need to be focused on systemic tumor control for high-risk neuroblastoma patients. Anti-GD2 treatment after tandem HDCT/auto-SCT could be one of the options to further improve the outcome for high-risk neuroblastoma patients [28–33]. In a recent phase III randomized clinical trial of tandem versus single HDCT/auto-SCT by the Children’s Oncology Group, the 3-year EFS was reported to be 73.7% in patients who received tandem HDCT/auto-SCT and post-consolidative immunotherapy [34]. Cellular immunotherapy such as adoptive transfer of chimeric antigen receptors (CAR) of T cells or NK cells could also be considered [35,36,37,38]. A combination of these immunotherapies following tandem HDCT/auto-SCT might further improve outcomes of high-risk neuroblastoma.
Five patients died from acute toxicities during the first HDCT/auto-SCT, and the tumor status before the first HDCT/auto-SCT was CR or VGPR in three of the five patients. In addition, the two patients who died from chronic lung disease after 18 mCi/kg of 131I-MIBG treatment were in a CR before the first HDCT/auto-SCT. This TRM rate is higher than in other studies. In this study, the dose of the first HDCT was same in all patients; however, the intensity of the first HDCT might be relatively higher in patients who are susceptible to the toxicity of chemotherapy, particularly in good responders to induction treatment. Similarly, the toxicity of 131I-MIBG treatment might be relatively higher in good responders than in poor responders.
In our previous study evaluating the relationship between an early response during induction treatment and subsequent outcome in high-risk neuroblastoma, relapse-free survival was higher in good responders than in poor responders; however, the TRM rate during tandem HDCT/auto-SCT was also relatively higher in good responders [39]. Therefore, it may be necessary to reduce the treatment intensity to reduce the TRM in the good responders. To the contrary, it might also be necessary to intensify the treatment, such as an increase of the 131I-MIBG dose, in the poor responders to reduce the relapse rate despite a possible increase in acute and chronic toxicities. Tailoring the HDCT intensity based on the response during induction treatment might improve the survival rate by minimizing the TRM and relapse rates.
Conclusions
In summary, incorporation of high-dose 131I-MIBG treatment into tandem HDCT/auto-SCT was feasible and could reduce short- and long-term toxicities without jeopardizing survival rates. However, this study is a single-arm prospective study of a relatively small number of patients; therefore, a randomized prospective study with a larger number of patients is needed to confirm the findings of our study. In addition, further improvements in treatment are still needed in order to improve patient outcomes. Combinations of immunotherapeutics and/or tailored therapy according to prior tumor response are possible options needing further investigation.
Abbreviations
- 99Tc:
-
Technetium-99
- auto-SCT:
-
Autologous stem cell transplantation
- BM:
-
Busulfan + melphalan
- CAR:
-
Chimeric antigen receptors
- CEC:
-
Carboplatin + etoposide + cyclophosphamide
- CEDC:
-
Cisplatin + etoposide + doxorubicin + cyclophosphamide
- CEM:
-
Carboplatin + etoposide + melphalan
- CR:
-
Complete response
- EFS:
-
Event-free survival
- HDCT:
-
High-dose chemotherapy
- ICE:
-
Ifosfamide + carboplatin + etoposide
- INPC:
-
International Neuroblastoma Pathology Classification
- INSS:
-
International Neuroblastoma Staging System
- MIBG:
-
Metaiodobenzylguanidine
- MR:
-
Mixed response
- MYCN:
-
MYCN proto-oncogene, bHLH transcription factor
- NANT:
-
New Approaches to Neuroblastoma Therapy
- OS:
-
Overall survival
- PBSCs:
-
Peripheral blood stem cells
- PD:
-
Progressive disease
- PR:
-
Partial response
- RT:
-
Radiotherapy
- SD:
-
Stable disease
- TBI:
-
Total-body irradiation
- TM:
-
Thiotepa + melphalan
- TRM:
-
Treatment-related mortality
- VGPR:
-
Very good partial response
References
Pritchard J, Cotterill SJ, Germond SM, Imeson J, de Kraker J, Jones DR. High dose melphalan in the treatment of advanced neuroblastoma: results of a randomised trial (ENSG-1) by the European Neuroblastoma Study Group. Pediatr Blood Cancer. 2005;44:348–57.
Berthold F, Boos J, Burdach S, Erttmann R, Henze G, Hermann J, et al. Myeloablative megatherapy with autologous stem-cell rescue versus oral maintenance chemotherapy as consolidation treatment in patients with high-risk neuroblastoma: a randomised controlled trial. Lancet Oncol. 2005;6:649–58.
Matthay KK, Villablanca JG, Seeger RC, Stram DO, Harris RE, Ramsay NK, et al. Treatment of high-risk neuroblastoma with intensive chemotherapy, radiotherapy, autologous bone marrow transplantation, and 13-cis-retinoic acid. Children’s Cancer Group. N Engl J Med. 1999;341:1165–73.
Philip T, Ladenstein R, Lasset C, Hartmann O, Zucker JM, Pinkerton R, et al. 1070 myeloablative megatherapy procedures followed by stem cell rescue for neuroblastoma: 17 years of European experience and conclusions. European Group for Blood and Marrow Transplant Registry Solid Tumour Working Party. Eur J Cancer. 1997;33:2130–5.
Ladenstein R, Potschger U, Pearson AD, Brock P, Luksch R, Castel V, et al. Busulfan and melphalan versus carboplatin, etoposide, and melphalan as high-dose chemotherapy for high-risk neuroblastoma (HR-NBL1/SIOPEN): an international, randomised, multi-arm, open-label, phase 3 trial. Lancet Oncol. 2017;18:500–14.
Kreissman SG, Seeger RC, Matthay KK, London WB, Sposto R, Grupp SA, et al. Purged versus non-purged peripheral blood stem-cell transplantation for high-risk neuroblastoma (COG A3973): a randomised phase 3 trial. Lancet Oncol. 2013;14:999–1008.
Sung KW, Lee SH, Yoo KH, Jung HL, Cho EJ, Koo HH, et al. Tandem high-dose chemotherapy and autologous stem cell rescue in patients over 1 year of age with stage 4 neuroblastoma. Bone Marrow Transplant. 2007;40:37–45.
Kletzel M, Katzenstein HM, Haut PR, Yu AL, Morgan E, Reynolds M, et al. Treatment of high-risk neuroblastoma with triple-tandem high-dose therapy and stem-cell rescue: results of the Chicago Pilot II Study. J Clin Oncol. 2002;20:2284–92.
George RE, Li S, Medeiros-Nancarrow C, Neuberg D, Marcus K, Shamberger RC, et al. High-risk neuroblastoma treated with tandem autologous peripheral-blood stem cell-supported transplantation: long-term survival update. J Clin Oncol. 2006;24:2891–6.
Sung KW, Son MH, Lee SH, Yoo KH, Koo HH, Kim JY, et al. Tandem high-dose chemotherapy and autologous stem cell transplantation in patients with high-risk neuroblastoma: results of SMC NB-2004 study. Bone Marrow Transplant. 2013;48:68–73.
DuBois SG, Matthay KK. 131I-Metaiodobenzylguanidine therapy in children with advanced neuroblastoma. Q J Nucl Med Mol Imaging. 2013;57:53–65.
Carlin S, Mairs RJ, McCluskey AG, Tweddle DA, Sprigg A, Estlin C, et al. Development of a real-time polymerase chain reaction assay for prediction of the uptake of meta-[(131)I]iodobenzylguanidine by neuroblastoma tumors. Clin Cancer Res. 2003;9:3338–44.
Hoefnagel CA, Voute PA, De Kraker J, Valdes Olmos RA. [131I]metaiodobenzylguanidine therapy after conventional therapy for neuroblastoma. J Nucl Biol Med. 1991;35:202–6.
Lashford LS, Lewis IJ, Fielding SL, Flower MA, Meller S, Kemshead JT, et al. Phase I/II study of iodine 131 metaiodobenzylguanidine in chemoresistant neuroblastoma: a United Kingdom Children’s Cancer Study Group investigation. J Clin Oncol. 1992;10:1889–96.
Lumbroso J, Hartmann O, Schlumberger M. Therapeutic use of [131I]metaiodobenzylguanidine in neuroblastoma: a phase II study in 26 patients. “Societe Francaise d’Oncologie Pediatrique” and Nuclear Medicine Co-investigators. J Nucl Biol Med. 1991;35:220–3.
Matthay KK, DeSantes K, Hasegawa B, Huberty J, Hattner RS, Ablin A, et al. Phase I dose escalation of 131I-metaiodobenzylguanidine with autologous bone marrow support in refractory neuroblastoma. J Clin Oncol. 1998;16:229–36.
Matthay KK, Yanik G, Messina J, Quach A, Huberty J, Cheng SC, et al. Phase II study on the effect of disease sites, age, and prior therapy on response to iodine-131-metaiodobenzylguanidine therapy in refractory neuroblastoma. J Clin Oncol. 2007;25:1054–60.
Brodeur GM, Pritchard J, Berthold F, Carlsen NL, Castel V, Castelberry RP, et al. Revisions of the international criteria for neuroblastoma diagnosis, staging and response to treatment. Prog Clin Biol Res. 1994;385:363–9.
Shimada H, Ambros IM, Dehner LP, Hata J, Joshi VV, Roald B, et al. The International Neuroblastoma Pathology Classification (the Shimada system). Cancer. 1999;86:364–72.
Ambros PF, Ambros IM, Brodeur GM, Haber M, Khan J, Nakagawara A, et al. International consensus for neuroblastoma molecular diagnostics: report from the International Neuroblastoma Risk Group (INRG) Biology Committee. Br J Cancer. 2009;100:1471–82.
Cohn SL, Pearson ADJ, London WB, Monclair T, Ambros PF, Brodeur GM, et al. The International Neuroblastoma Risk Group (INRG) classification system: an INRG Task Force report. J Clin Oncol. 2009;27:289–97.
French S, DuBois SG, Horn B, Granger M, Hawkins R, Pass A, et al. 131I-MIBG followed by consolidation with busulfan, melphalan and autologous stem cell transplantation for refractory neuroblastoma. Pediatr Blood Cancer. 2013;60:879–84.
Matthay KK, Tan JC, Villablanca JG, Yanik GA, Veatch J, Franc B, et al. Phase I dose escalation of iodine-131-metaiodobenzylguanidine with myeloablative chemotherapy and autologous stem-cell transplantation in refractory neuroblastoma: a new approaches to Neuroblastoma Therapy Consortium Study. J Clin Oncol. 2006;24:500–6.
Yanik GA, Villablanca JG, Maris JM, Weiss B, Groshen S, Marachelian A, et al. 131I-metaiodobenzylguanidine with intensive chemotherapy and autologous stem cell transplantation for high-risk neuroblastoma. A new approaches to neuroblastoma therapy (NANT) phase II study. Biol Blood Marrow Transplant. 2015;21:673–81.
Clement SC, van Eck-Smit BL, van Trotsenburg AS, Kremer LC, Tytgat GA, van Santen HM. Long-term follow-up of the thyroid gland after treatment with 131I-Metaiodobenzylguanidine in children with neuroblastoma: importance of continuous surveillance. Pediatr Blood Cancer. 2013;60:1833–8.
Clement SC, van Rijn RR, van Eck-Smit BL, van Trotsenburg AS, Caron HN, Tytgat GA, et al. Long-term efficacy of current thyroid prophylaxis and future perspectives on thyroid protection during 131I-metaiodobenzylguanidine treatment in children with neuroblastoma. Eur J Nucl Med Mol Imaging. 2015;42:706–15.
Garaventa A, Gambini C, Villavecchia G, Di Cataldo A, Bertolazzi L, Pizzitola MR, et al. Second malignancies in children with neuroblastoma after combined treatment with 131I-metaiodobenzylguanidine. Cancer. 2003;97:1332–8.
Kushner BH, Kramer K, Cheung NK. Phase II trial of the anti-G(D2) monoclonal antibody 3F8 and granulocyte-macrophage colony-stimulating factor for neuroblastoma. J Clin Oncol. 2001;19:4189–94.
Osenga KL, Hank JA, Albertini MR, Gan J, Sternberg AG, Eickhoff J, et al. A phase I clinical trial of the hu14.18-IL2 (EMD 273063) as a treatment for children with refractory or recurrent neuroblastoma and melanoma: a study of the Children’s Oncology Group. Clin Cancer Res. 2006;12:1750–9.
Cheung NK, Kushner BH, Kramer K. Monoclonal antibody-based therapy of neuroblastoma. Hematol Oncol Clin North Am. 2001;15:853–66.
Yu AL, Gilman AL, Ozkaynak MF, London WB, Kreissman SG, Chen HX, et al. Anti-GD2 antibody with GM-CSF, interleukin-2, and isotretinoin for neuroblastoma. N Engl J Med. 2010;363:1324–34.
Ho WL, Hsu WM, Huang MC, Kadomatsu K, Nakagawara A. Protein glycosylation in cancers and its potential therapeutic applications in neuroblastoma. J Hematol Oncol. 2016;9:100.
Maris JM. Recent advances in neuroblastoma. N Engl J Med. 2010;362:2202–11.
JR Park, SG Kreissman, WB London, A Naranjo, SL Cohn, MD Hogarty, et al. A phase III randomized clinical trial (RCT) of tandem myeloablative autologous stem cell transplant (ASCT) using peripheral blood stem cell (PBSC) as consolidation therapy for high-risk neuroblastoma (HR-NB): a Children’s Oncology Group (COG) study. J Clin Oncol. 2016;34 (suppl; abstr LBA3).
Louis CU, Savoldo B, Dotti G, Pule M, Yvon E, Myers GD, et al. Antitumor activity and long-term fate of chimeric antigen receptor-positive T cells in patients with neuroblastoma. Blood. 2011;118:6050–6.
Pule MA, Savoldo B, Myers GD, Rossig C, Russell HV, Dotti G, et al. Virus-specific T cells engineered to coexpress tumor-specific receptors: persistence and antitumor activity in individuals with neuroblastoma. Nat Med. 2008;14:1264–70.
Park JR, Digiusto DL, Slovak M, Wright C, Naranjo A, Wagner J, et al. Adoptive transfer of chimeric antigen receptor re-directed cytolytic T lymphocyte clones in patients with neuroblastoma. Mol Ther. 2007;15:825–33.
Seidel D, Shibina A, Siebert N, Wels WS, Reynolds CP, Huebener N, et al. Disialoganglioside-specific human natural killer cells are effective against drug-resistant neuroblastoma. Cancer Immunol Immunother. 2015;64:621–34.
Yoo SY, Kim JS, Sung KW, Jeon TY, Choi JY, Moon SH, et al. The degree of tumor volume reduction during the early phase of induction chemotherapy is an independent prognostic factor in patients with high-risk neuroblastoma. Cancer. 2013;119:656–64.
Acknowledgements
We would like to thank Miss So Yeon Lee for her assistance with the data collection.
Funding
This study was supported by a grant from the National R&D Program for Cancer Control, Ministry of Health and Welfare, Republic of Korea (No. 1520210).
Availability of data and materials
The datasets collected and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors’ contributions
KWS, SKL, and DHL designed and performed the study. JWL, SHL, HWC, YM, KHY, KWS, HHK, and EJC collected and analyzed the data. JWL, SHL, and KWS participated in drafting the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was approved by the Institutional Review Board of Samsung Medical Center, and written informed consent was obtained from the parents of each patient.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lee, J.W., Lee, S., Cho, H.W. et al. Incorporation of high-dose 131I-metaiodobenzylguanidine treatment into tandem high-dose chemotherapy and autologous stem cell transplantation for high-risk neuroblastoma: results of the SMC NB-2009 study. J Hematol Oncol 10, 108 (2017). https://doi.org/10.1186/s13045-017-0477-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13045-017-0477-0