Abstract
Background
Ipsilateral femoral shaft and neck fractures are rare injuries, affecting mostly young patients who sustained high-energy traumas. In 19–50% of cases, the femoral fracture is misdiagnosed or overlooked at the initial presentation, with reportedly increased risk of complications such as non-union and avascular necrosis. We present a case of an ipsilateral femoral neck and shaft fracture, which was missed at initial presentation despite radiographic and computed tomography (CT) scan evaluation.
Case presentation
A 56-year old female was admitted to our institution following a high-energy trauma (fall from 6 m). Initial radiographic and CT scan evaluation revealed a displaced femoral shaft fracture but no other femoral fractures were detected. Closed reduction and external fixation of the femoral shaft fracture was performed in the emergency setting. Follow-up radiologic evaluations revealed an ipsilateral laterally displaced femoral neck fracture. Despite cephalomedullary nail fixation of both fractures performed on the third day from the initial injury, the patient developed a non-union of the femoral neck fracture, which led to cut-out of the lag screw with associated varus failure of the femoral neck fracture requiring surgical revision and implant of a bipolar hemiarthroplasty at one year follow up. The postoperative course was uneventful and the patient had a full long-term recovery.
Conclusion
This case report exemplifies the need to maintain the highest level of suspiciousness for the concomitant presence of an ipsilateral femoral neck fracture when treating polytraumatized patients who sustained a femoral shaft fracture as a consequence of a high-energy trauma. Furthermore, the pre-operative standardized radiological evaluation (plain x-ray and CT scan) might not always help in ruling out these fractures. It is therefore necessary to adopt additional standardized radiographic protocols not only in the pre-operative but also in the intra-operative and immediate post-operative settings.
Similar content being viewed by others
Background
Ipsilateral femoral shaft and neck fractures are uncommon injuries [1,2,3,4,5]. The incidence is approximately 0.8 to 9% of all femoral shaft fractures [2, 3, 6,7,8,9,10,11,12,13,14,15]. Most of the patients are young adults, who sustained multiple injuries caused by high-energy trauma such as traffic accidents and jumping or falling from heights [2, 4, 7,8,9,10,11,12,13, 16,17,18]. Ipsilateral shaft and neck fractures in the elderly may occur after low-energy injuries [3, 9, 13, 19,20,21,22]. We report our experience with a patient affected by femoral shaft and neck fractures and we discuss the proposed diagnostic algorithms, the treatment approaches, and the complications presented in the literature.
Case presentation
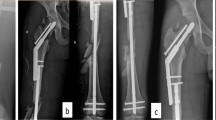
The patient was a 56-year old female, who sustained several injuries during a fall from 6 m (third floor). Glasgow Coma Scale (GCS) on admission was 6–7/15. Injury Severity Scale (ISS) score was 34 [Table 1]. She was intubated, stabilized and admitted. The initial diagnostic evaluation was performed according to Advanced Trauma Life Support (ATLS) guidelines and included Focused Assessment with Sonography in Trauma (FAST), chest x-ray and pelvic antero-posterior (AP) x-rays, CT-trauma scan and femoral x-rays. Trauma workup revealed diffuse intracerebral contusion, a small parieto-occipital subarachnoid hemorrhage on the right, bilateral mediastinum and lung contusion, maxillary-orbital and temporal bone fractures, the radiological examination revealed a femoral shaft fracture on the left. No other femoral fractures were detected upon X-ray examination [Fig. 1]. CT coronal and axial views of the pelvis (3 mm thickness) and of the proximal femur did not show clear evidence of fracture [Fig. 2]. Initial treatment, on the day of admission, consisted of closed reduction and external fixation of the femoral shaft. During surgical treatment of the maxillary fractures on post-injury day 1, it was noted that the left lower extremity was shortened and externally rotated. Plain films of the left hip, femur, and knee demonstrated a displaced femoral neck facture and an ipsilateral patellar fracture [Fig. 3]. On post-injury day 3, the left femoral shaft and neck fracture was treated with a cephalomedullary nail on a standard traction table by closed reduction. Anatomic reduction and stable fixation of the femur fractures were ascertained intra-operatively by fluoroscopic control, revealing a tip-apex-distance of 10 mm and a central position of the lag screw. The patella fracture was treated with a standard figure-of-8 tension band wire [Fig. 4]. Post-operative radiographic control confirmed the satisfactory reduction and stabilization of the left femoral neck and shaft fracture as well as of the ipsilateral patella fracture [Fig. 5]. The post-operative course was uneventful. The patient was transferred to a rehabilitation center four weeks after admission and had a physiotherapy exercise protocol with weight bearing on the left lower extremity up to max 10–15 kg (kg) for 6 weeks post-operatively. Full weight-bearing was allowed after 12 weeks. Sport activities were restricted for 6 months. At post-operative weeks 9 and 16, the patient complained of pain in the left groin and shaft, and radiographs demonstrated callous formation in the left femoral shaft. X-rays at post-operative week 28 demonstrated lag-screw cut-out with displacement of the femoral neck fracture [Fig. 6]. The patient was offered surgical revision but she refused at this time. One year after injury, the patient agreed to revision surgery and on week 52 (1 year) post-injury she underwent removal of the cephalomedullary implant and placement of a bipolar hemiarthroplasty after being offered a total hip replacement, which she refused. Post-operative clinical and radiological controls were unremarkable [Fig. 7]. Post-operative course was uneventful and the patient was transferred to a rehabilitation center two weeks after the surgery.
Discussion
Overlooked or delayed diagnoses are commonly reported in literature when treating polytraumatized patients (1.3 to 39%) [23, 24]. In case of ipsilateral femoral neck and shaft fractures, the delayed diagnosis of the femoral neck fracture occurs in 19 to 50% of patients during the initial examination [2, 7, 8, 11, 12, 19, 25,26,27,28]. According to the literature, several factors may account for the pre-operative mis- or delayed diagnosis of ipsilateral femoral shaft and neck fractures. Among others, the main factor includes the type of fracture (nondisplaced or minimally displaced in 26 to 59% of cases) [2, 29], as in our case. The pre-operative hip and pelvic radiographic exams were initially deemed negative for a femoral neck fracture since no displacement was evident. As the patient was already intubated upon arrival, collection of symptoms supporting suspicion of a femoral neck fracture was minimal during early clinical examination. The treatment was focused on life-threatening and obvious injuries. The particularities of the treatment of a multiply injured patient, in addition, may play a role in the delayed diagnosis [11, 12, 27]. Several studies show that an insufficient radiological protocol seems to affect the incidence of mis- or delayed diagnosis [2, 4, 11,12,13,14, 18, 26, 28, 30,31,32,33].
In our case the patient was evaluated with a pre-operative AP pelvis, which was negative. It is unclear whether a lateral view of the hip could have been more sensitive in detecting the femoral neck fracture. Nonetheless, we tend to agree with the statement that a dedicated antero-posterior internal rotation hip radiograph, performed intra-operatively or immediately after the reduction and stabilization of the femoral shaft fracture, could have improved the likelihood of detecting the fracture of the femoral neck, by minimally displacing the femoral neck fracture and making the diagnosis less difficult [28].
The diagnostic value of the preoperative CT scan is still controversial. Some authors claim that its use helps reducing the delay in diagnosis of femoral neck fracture (from 57 to 6.3%) [26, 28, 29, 34, 35]. Others claim that the significance of CT is equivalent of that of the plain radiography (sensitivity of only 56% to 64) [29, 36, 37]. In our case the emergency CT scan available offered coronal and axial views with thickness of 3 mm. Perhaps using thin-cut computer tomography CT scan (thickness 1–2 mm) could have improved the ability to detect the non-displaced femoral neck fractures. Combining different preoperative (thin-cut computed tomography CT scan and dedicated antero-posterior internal rotation radiographs of the femoral neck, including 2D CT reconstructions), intraoperative (lateral hip fluoroscopic view by angulation of the radiographic beam before reducing the shaft fracture or plain radiograph view centered at the hip with 10° to 15° of hip internal rotation following fixation) and postoperative (dedicated AP internal rotation views of the hip) clinical and radiological measures should help reduce the incidence of a missed femoral neck fracture.
In our case a pre-operative CT was performed according to the protocol and no evidence of femoral neck fracture was found. We agree with other authors that CT scan even when associated with plain radiographs should not be considered as an unreserved assessment tool [36, 37] and that intra-operative maneuvers and radiographs should be used to rule out concomitant femoral neck fractures.
Variable rates of complications and results have been reported in patients suffering from ipsilateral femoral neck and shaft fracture [3, 9, 13, 16, 38]. Common complications (incidence 4 to 22%) of the femoral head are aseptic necrosis [5, 11, 12, 31] and nonunion [11, 12, 31, 39,40,41]. Complications of the shaft fractures are nonunion caused by an open fracture, inadequate implant (nail diameter too small), no reaming and prolonged delay to weight bearing [2, 3]. Clear evidence that a delayed diagnosis of femoral neck fracture in these complex injuries affects the incidence of complications such as non-union and avascular necrosis [2, 3, 7, 8, 19] is still lacking. According to some authors, the delayed diagnosis of femoral neck fracture in these complex injuries does not seem to affect the incidence of complications such as non-union and avascular necrosis [2, 19]. Conversely others report that the risk of healing complications is higher in late surgery compared to early surgery and in combined shaft and neck fractures compared to one-level-injuries [3]. In the present case report the delay between diagnosis and treatment of the ipsilateral femoral neck and shaft fracture was 2 days, making it impossible to state with certainty whether or not the delay in diagnosis is responsible for the non-union. Timely recognition and early surgical treatment of ipsilateral femoral shaft and neck fractures are crucial for early mobilization and rehabilitation, allowing overall good functional outcomes [6, 17] and reduces mortality and morbidity [25]. Deciding on the appropriate therapy remains challenging [3]. Different strategies for the treatment of ipsilateral femoral neck and shaft fractures have been proposed: cannulated screws for the femoral neck and a retrograde locking nail for the femoral shaft [4, 35, 42], cephalomedullary implant [7,8,9, 20, 43], antegrade nail with one neck screw [6, 13, 20, 22, 44, 45], long proximal femoral nail [46, 47]. At the present time, however, there is still no consensus on the superiority of a treatment protocol [17, 48, 49]. In the present case, we opted to treat both fractures with antegrade nail with one neck screw and the timing for the surgery was within one week from the traumatic event. The intra- and post-operative radiographs excluded the presence of a reduction in varus and implant placement was deemed satisfactory, although a smaller tip-apex distance could have provided a better purchase in subchondral bone and therefore possibly reduce the risk of early cut-out [28].
Conclusion
In polytraumatized patients with injuries caused by high-energy trauma one must expect and rule out combined injuries of the femur at different levels. Despite the uncommon presentation of this complex fracture pattern, the knowledge and awareness of this complex injury pattern should be increased in every Trauma Center. The use of specific standardized protocols for the correct diagnosis and treatment of such fractures in order to decrease the incidence of devastating complications should be implemented. The present case clearly shows that even the use of a preoperative CT scan in addition to routine pelvic and hip joint radiograph might sometimes lead to a misdiagnosis. It is therefore important to understand that, especially in polytraumatized, non-collaborating patient who present with femoral shaft fracture, the highest level of suspiciousness must be maintained for the concomitant presence of an ipsilateral femoral neck fracture. Thus the combination of specific radiographic preoperative, intraoperative and postoperative views of the femoral neck should be integrated in the ATLS algorithm of the polytraumatized patient [26] to help reduce the incidence of a missed femoral neck fracture.
Abbreviations
- 2D CT:
-
Two dimensional computerized tomography
- AIS:
-
Abbreviated injury score
- AP:
-
Antero-posterior
- ATLS:
-
Advanced trauma life support
- CT:
-
Computed tomography
- FAST:
-
Focused assessment for sonography in trauma
- GCS:
-
Glasgow coma scale
- ISS:
-
Injury severity score
References
Sadeghifar A, Saied A. Bilateral simultaneous femoral neck and shafts fractures - A case report. Arch Bone Joint Surg. 2014;2(4):268–71.
Wolinsky PR, Johnson KD. Ipsilateral femoral neck and shaft fractures. Clin Orthop Relat Res. 1995;318:81–90.
Watson JT, Moed BR. Ipsilateral femoral neck and shaft fractures: complications and their treatment. Clin Orthop. 2002;399:78–86.
Peljovich AE, Patterson BM. Ipsilateral femoral neck and shaft fractures. J Am Acad Orthop Surg. 1998;6:106–13.
Winquist RA. Locked femoral nailing. J Am Acad Orthop Surg. 1993;1(2):95–105.
Tsarouhas A, Hantes ME, Karachalios T, Bargiotas K, Malizos KN. Reconstruction nailing for ipsilateral femoral neck and shaft fractures. Strat Traum Limb Recon. 2011;6(2):69–75.
Alho A. Concurrent ipsilateral fractures of the hip and femoral shaft: a meta-analysis of 659 cases. Acta Orthop Scand. 1996;67(1):19–28.
Alho A. Concurrent ipsilateral fractures of the hip and shaft of the femur. A systematic review of 722 cases. Ann Chir Gynaecol. 1997;86(4):326–36.
Jain P, Maini L, Mishra P, Upadhyay A, Agarwal A. Cephalomedullary interlocked nail for ipsilateral hip and femoral shaft fractures. Injury. 2004;35(10):1031–8.
Zettas JP, Zettas P. Ipsilateral fractures of the femoral neck and shaft. Clin Orthop Relat Res. 1981;160:63–73.
Swiontkowski MF, Hansen ST, Kellam J. Ipsilateral fractures of the femoral neck and shaft. A treatment protocol. J Bone Joint Surg Am. 1984;66(2):260–8.
Swiontkowski MF. Ipsilateral femoral shaft and hip fractures. Orthop Clin N Am. 1987;18:73–84.
Wu CC, Tai CL. Reconstruction interlocking nails for ipsilateral femoral neck and shaft fractures: biomechanical analysis of effect of supplementary cannulated screw on intracapsular femoral neck fracture. Clin Biomech. 2009;24(8):642–7.
Riemer BL, Butterfield SL, Ray RL, Daffner RH. Clandestine femoral neck fractures with ipsilateral diaphyseal fractures. J Orthop Trauma. 1993;7:443–9.
Schatzker J, Barrington TW. Fractures of the femoral neck associated with fractures of the same femoral shaft. Can J Surg. 1968;11(3):297–305.
Hung SH, Hsu CY, Hsu SF, Huang PJ, Cheng YM, Chang JK, et al. Surgical treatment for ipsilateral fractures of the hip and femoral shaft. Injury. 2004;35:165–9.
Singh R, Rohilla R, Magu NK, Siwach R, Kadian V, Sangwan SS. Ipsilateral femoral neck and shaft fractures: a retrospective analysis of two treatment methods. J Orthop Traumatol. 2008;9(3):141–7.
Gill SS, Nagi ON, Dhillon MS. Ipsilateral fractures of femoral neck and shaft. J Orthop Trauma. 1990;4:293–8.
Bennett FS, Zinar DM, Kilgus DJ. Ipsilateral hip and shaft fractures. Clin Orthop Relat Res. 1993;296:168–77.
Hossam Elshafie M, Adel Morsey H, Emad Eid T. Ipsilateral fracture of the femoral neck and shaft, treatment by reconstruction interlocking nail. Arch Orthop Trauma Surg. 2001;121:71–4.
Kao HK, Wu CC, Lee PC, et al. Ipsilateral femoral neck and shaft fractures treated with Russell–Taylor reconstruction intramedullary nails. Chang Gung Med J. 2006;29:79–85.
Randelli P, Landi S, Fanton F, et al. Treatment of ipsilateral femoral neck and shaft fractures with the Russell–Taylor reconstructive nail. Orthopedics. 1999;22:673–6.
Pfeifer R, Pape HC. Missed injuries in trauma patients: A literature review. Patient Saf Surg. 2008;2:20.
Houshian S, Larsern MS, Holm C. Missed injuries in a level I trauma center. J Trauma. 2002;52:715–9.
Plancher KD, Donshik JD. Femoral neck and ipsilateral neck and shaft fractures in the young adult. Orthop Clin North Am. 1997;28(3):447–59.
Tornetta P, Kain MS, Creevy WR. Diagnosis of femoral neck fractures in patients with a femoral shaft fracture. Improvement with a standard protocol. J Bone Joint Surg Am. 2007;89(1):39–43.
Whittle AP, Wood GWII. Fractures of lower extremity. In: Canale ST, editor. Campbell’s operative orthopaedics. St. Louis: Mosby; 2003. p. 2725–872.
McDonald LS, Tepolt F, Leonardelli D, Hammerberg EM, Stahel PF. A cascade of preventable complications following a missed femoral neck fracture after antegrade femoral nailing. Patient Saf Surg. 2013;7:16.
Hak D, Mauffrey C, Hake M, Hammerberg E, Stahel P. Ipsilateral femoral neck and shaft fractures: current diagnostic and treatment strategies. Orthopedics. 2015;38:247–51.
Schmal H, Strohm PC, Mehlhorn AT, Hauschild O, Südkamp NP. Management of ipsilateral femoral neck and shaft fractures. Unfallchirurg. 2008;111(11):886–91.
Casey MJ, Chapman MW. Ipsilateral concomitant fractures of the hip and femoral shaft. J Bone Joint Surg Am. 1979;61:503–9.
Dencker H. Femoral shaft fracture and fracture of the neck of the same femur. Acta Chir Scand. 1965;129:597–605.
Kimbrough EE. Concomitant unilateral hip and femoral-shaft fractures - a too frequently unrecognized syndrome. Report of five cases. J Bone Joint Surg Am. 1961;43:443–9.
Douša P, Bartoníček J, Pavelka T, Luňáček L. Ipsilateral fractures of the proximal femur and the femoral shaft. Acta Chir Orthop Traumatol Cechoslov. 2010;77(5):378–88.
Ostrum RF, Tornetta P, Watson JT, Christiano A, Vafek E. Ipsilateral proximal femur and shaft fractures treated with hip screws and a reamed retrograde intramedullary nail. Clin Orthop Relat Res. 2014;472(9):2751–8.
O’Toole RV, Dancy L, Dietz AR, et al. Diagnosis of femoral neck fracture associated with femoral shaft fracture: blinded comparison of computed tomography and plain radiography. J Orthop Trauma. 2013;27:325–30.
Heiney JP, Leeson MC, Vrabec GA. Delayed diagnosis of an ipsilateral femoral neck fracture with an associated femoral shaft fracture in light of a negative computed tomography scan. J Trauma. 2009;67(4):129–31.
Starr AJ, Bucholz RW. Fractures of the shaft of the femur. In: Bucholz RW, Heckman JD, editors. Rockwood and Green’s fractures in adults. Philadelphia: Lippincott Williams & Wilkins; 2001. p. 1683–730.
Friedman RJ, Wyman ET Jr. Ipsilateral hip and femoral shaft fractures. Clin Orthop Relat Res. 1986;208:188–94.
Wiss DA, Sima W, Brien WW. Ipsilateral fractures of the femoral neck and shaft. J Orthop Trauma. 1992;6:159–66.
MacKenzie D. Simultaneous ipsilateral fracture of the femoral neck and shaft: report of 8 cases. South African Med J. 1971;45:459–67.
Oh CW, Oh JK, Park BC, Jeon IH, Kyung HS, Kim SY, et al. Retrograde nailing with subsequent screw fixation for ipsilateral femoral shaft and neck fractures. Arch Orthop Trauma Surg. 2006;126(7):448–53.
Gary JL, Taksali S, Reinert CM, Starr AJ. Ipsilateral femoral shaft and neck fractures: are cephalomedullary nails appropriate? J Surg Orthop Adv. 2011;20(2):122–5.
Okcu G, Aktuglu K. Antegrade nailing of femoral shaft fractures combined with neck or distal femur fractures. A retrospective review of 25 cases, with a follow-up of 36-150 months. Arch Orthop Trauma Surg. 2003;123(10):544–50.
Wruhs O, Jenny JY, Karger C. Management of combination injuries of the femur shaft and femoral neck fractures with a locking nail. Multicenter study of 26 cases from 4 trauma clinics. Unfallchirurgie. 1986;12(4):208–14.
Wang WY, Liu L, Wang GL, Fang Y, Yang TF. Ipsilateral basicervical femoral neck and shaft fractures treated with long proximal femoral nail antirotation or various plate combinations: comparative study. J Orthop Sci. 2010;15(3):323–30.
Gadegone W, Lokhande V, Salphale Y, Ramteke A. Long proximal femoral nail in ipsilateral fractures proximal femur and shaft of femur. Indian J Orthop. 2013;47(3):272–7.
Boulton CL, Pollak AN. Special topic: ipsilateral femoral neck and shaft fractures--does evidence give us the answer? Injury. 2015;46(3):478–83.
Bedi A, Karunakar MA, Caron T, Sanders RW, Haidukewych GJ. Accuracy of reduction of ipsilateral femoral neck and shaft fractures--an analysis of various internal fixation strategies. J Orthop Trauma. 2009;23(4):24.
Acknowledgements
Not applicable.
Funding
The publication costs for this article were covered in full by a grant from the Colorado Physician Insurance Company (http://www.copic.com) to Philip F. Stahel, MD. COPIC had no influence on authorship or scientific content of this article.
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
SL and SK designed the case report. SL wrote the first draft of the manuscript. IF, BK and SK systematically edited the manuscript. All authors critically revised this paper, and read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that there is no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Labza, S., Fassola, I., Kunz, B. et al. Delayed recognition of an ipsilateral femoral neck and shaft fracture leading to preventable subsequent complications: a case report. Patient Saf Surg 11, 20 (2017). https://doi.org/10.1186/s13037-017-0134-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13037-017-0134-0