Abstract
Background
Depression is the leading cause of disability at a population level and globally 350 million people are suffering from depression. Despite a high prevalence and serious consequences, people with depression are reluctant to seek help and a large proportion remains untreated. The aim of this study was to assess intention to seek help for depression and associated factors among residents of Aykel town, Northwest Ethiopia.
Methods
This cross-sectional population based study included 832 participants. We used a major depressive disorder case vignette and general help-seeking questionnaire (GHSQ) to assess intention. Study participants selected by multistage cluster sampling technique. Face-to-face interview used to collect data. We performed adjusted multiple linear regression analyses to identify factors for intention to seek help.
Results
The mean score on intention to seek help from any health professionals was 3.72 (SD = 1.23) with a range of (1 “very unlikely” to 5 “very likely”). Majority of the respondents had an intention to visit health professionals to get a remedy for their illness depicted in the vignette. The proportion of those who had an intention to seek help from any health professionals if they were having depression was 71.2%. Favorable attitude towards seeking professional help for depression positively associated with an intention to seek help with (unstandardized β = 0.03, 95% CI (0.01, 0.05), p-value < 0.001). Other factors positively associated with an intention to seek help for depression were age (β = 0.02, CI (0.01, 0.03) p < 0.001), and perceived need of treatment for depression (β = 0.19, CI (0.01, 0.38), p < 0.05). Poor social support was negatively associated with an intention to seek help for depression (β = − 0.39 CI − 0.68, − 0.10, p < 0.05).
Conclusions
The results suggest that over two-third of the respondents reported that they were likely or very likely to seek help from health professionals if they were having depression. Increased age, favorable attitude to depression, and perceived need for treatment were factors for intention to seek help. Interventions focusing on awareness creation and attitude change towards depression are necessary.
Similar content being viewed by others
Background
Mental health remains a neglected issue in most developing countries, especially in rural areas [1]. Mental disorders were the leading cause of years lived with disability worldwide. Depressive disorder accounted for 40.5% of DALYs caused by mental disorders [2]. Depression affects people in all communities worldwide [3]. One of the most tragic result of depression is suicide [4]. Over 350 million people affected globally with depression. While depression is present in both gender, it is more common in women than men [5]. Depression decreases as people get older [6]. In Ethiopia, depression contributed 7% of the total disease burden [7].
Negative beliefs and attitude, social norm and past treatment behavior predict low perceived depression treatment need [8]. Most people believed vitamins and special diets were more often rated as helpful and dealing with the problem alone would be helpful [1]. Perceived stigma toward depression also has an impact upon the intention of people to seek professional help [9]. Despite mental disorders are prevalent in worldwide, people have understood depressive symptoms as less serious and not requiring treatment and therefore those suffering from depression are unwilling to seek professional help [10, 11]. So caring for these individuals, particularly in the rural areas left to the families and local healers. Regarding to gender, women exhibited more favourable intention to seek help from mental health professionals than men, likely because of their positive attitudes concerning psychological openness [3]. Access to mental health care in low income countries like Ethiopia remains poor. Currently, in Ethiopia ministry of health is practicing community based mental health services including integration of mental health service at primary health care (PHC) level. Social acceptability in relation to ignorance and belief systems is an impediment to mental health care services in Ethiopia. According to most Ethiopians’ perception, mental illness believed to be affliction by psychosocial stressors and supernatural forces (like demon possessions, bewitchments by an evil spirit, ancestor’s sprit, or evil eye) rated more important causes of mental than physical illnesses [12]. Prayer and home/family care suggested more strongly for treating mental than physical illnesses [12, 13]. Attitude towards mental illness affect people to seek help from health professionals [14, 15]. Most people in Ethiopia use traditional methods for treating mental illness and those who look for a modern treatment do so having tried the local means [16, 17]. Affected individuals or their families often seek help from religious and traditional healers rather than health facilities [7]. Understanding intention of people to seek help is important for early intervention of the burden of depression since intention is a predictor of behavior [15, 18]. However, to the best of my knowledge there is a limited information regarding communities’ intention for depressive symptoms in Ethiopia. Therefore, this study focus on help seek intention and identify associated factors for depressive symptoms among residents of Aykel town.
Objective
This study aimed to assess intention to seek help for depression and associated factors among residents of Aykel town, North West, Ethiopia.
Methods
Study design and setting
We conducted a population based cross-sectional study among adults in Aykel town, Chilga district, Northwest Ethiopia between April and May, 2015. The town has a total population of 18,507.
Sampling
A multi stage cluster sampling technique was used to sample the community members. Simple random sampling technique was used to select one kebele (an administrative unit of Ethiopia, similar to a ward and consists 5000 people) from total of two kebeles since population is large. Each kebele has ketenas (cluster), which is subdivision of kebele. Ketenas were selected randomly and we were selecting 12 ketenas. From the selected 12 ketenas, every eligible individuals/adults/living in these ketena were interviewed by data collectors until the determined sample size full.
Measurement
General help seeking questionnaire (GHSQ) adapted from previously used research among young people’s help-seeking for mental health problems in Australia [19].
We used general help seeking questionnaire with case vignette for major depressive disorder to measure intention to seek help. GHSQ is measured with likert type scale ranging from (1) “very unlikely” to (5) “very likely”. “If they were feeling like symptoms described in the vignette how likely is it, they would seek help from health professionals?.” High scores for professional help show a person had a good intention.
Depression vignette
A 28-year-old man has been feeling unusually sad and down-hearted for most of the day for over 2 weeks. He doesn’t feel like eating and has lost weight. He can’t keep his mind on his work and his financial income has dropped. He has put off deciding and feels that even day-to-day tasks are too much for him. To him, life feels meaningless, and he doesn’t feel he is worth much as a person. If you were feeling like above case how likely it is, you would seek help from the following people? Please show your response by putting a line through the number that best describes your intention to seek help from each help source.
We used Short Explanatory Model Interview (SEMI) to measure perceived severity, cause and need for treatment. We adapted the instrument from previously used research in London [20]. To examine perceived severity, we asked respondents: “How sever do you think is the illness presented in the vignette?” and the response were mild, moderate, severe and very severe. We assessed perceived need for treatment by questioned:” Do you think this illness requires treatment?” and the response were yes/no.
We used Attitudes Toward Seeking Professional Psychological Help (ATSPPH) to assess attitude towards depression. We adapted from research conducted in Turkey among college students [21]. This instrument has 10 items with a likert scale response which ranges from (1) “strongly disagree” to (5) “strongly agree”. Higher scores reflect more attitudes that are positive.
We measured social support using Oslo 3-items, social support scale and with scores ranging between 3 and 14: 3–8 = poor social support; 9–11 = intermediate social support; and 12–14 = strong social support [22].
Family history of mental illness
To examine the family history of mental illness, we asked: “Do you know a family member who had experienced a similar situation, or whether they had ever felt this way to that described in the vignette?”
Items on socio-demographic factors (age, sex, ethnicity, religion, marital status, educational status and occupational status) were adopted from different literatures.
Data collection
We collected data by four trained data collectors (public health professionals) using the Amharic version of the questionnaire for a month. We designed the questionnaire in English and translated to Amharic, the official language of Ethiopia and back to English, forward and backward translation. The training was on introduction to depression and research methods, interviewing skills, sampling and recruitment and ethical aspects of research.
Data processing and analysis
We checked all the collected data for completeness and consistency and entered to EPI INFO version 3.5.3 and then exported to SPSS for windows version 20 for analysis. We computed descriptive and simple linear regression analyses to see frequency distribution and to test whether there was an association between the independent and dependent (help seeking intention) variables, respectively. In the current study, the internal consistency for intention to seek help for depression was measured by cronbach’s alpha which was α = 0.79.
We selected factors associated with help seeking intention during simple linear regression analysis with a value of p ≤ 0.2 for further analysis in multivariable regression analysis. We considered variables with p-value as statistically significant.
Ethical consideration and consent
We obtained ethical clearance from the University of Gondar institutional review board and Amanuel Mental specialized Hospital. Formal letter of permission obtained from Aykel town administration. After explaining the aim of the study and the confidentiality issue, we invite them to take part in the project. We obtained verbal consent from participants after asking” are you voluntary to take part in the study?” and if they were voluntary, they would put their signature for that idea was their own. Confidentiality was maintained by omitting their personal identification.
Results
About 832 participants took part in the study, with a response rate of 98.3%. The mean age of respondents was 28.7 (SD = 9.5) years and 489 (58.8%) of the respondents were male. Concerning educational status, about one in five either had attended primary education or hadn’t attended any formal education. From the total of participants 407 (48.9%) were single (see Table 1).
Out of the total respondents, 123 (14.8%) said, they have a family member with mental illness similar to the situation presented in the vignette. About 363 (43.5% reported poor social support), 389 (46.8%) moderate social support and 81 (9.7%) had strong social support of the respondents.
Regard to perception about depression, only 75 (9%) understand depression was a severe illness and about 668 (80.3%) thought psychosocial factors cause it. Slightly less than half 391 (47.0%) of the respondents perceived that depression requires treatment (see Table 2). The mean score of participants’ attitude towards depression was 38.87 (SD = 4.39) (see Table 3).
Intention to seek help for depression
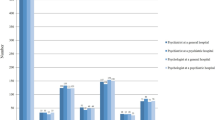
Mean score of intention to seek help from any health professionals was 3.72 (SD = 1.23). Implying that the majority of the respondents had an intention to visit health professionals to get a remedy for their illness depicted in the vignette. A close look into each item of the scale also shows that many respondents intended to visit health professionals soon. For instance, the proportion of respondents who said, they were likely or very likely to seek help from any health professional if they were having symptoms described in the vignette was 592 (71.2%). After presenting the depressive vignette we were asking:
“If you were feeling like symptoms described in the vignette how likely is it, you would seek help from health professionals?”. The response were likert type scale ranging from (1) “very unlikely” to (5) “very likely”. High scores show good intention (see Fig. 1).
Factors associated with an intention to seek help for depression
Simple linear regression analysis of help seeking intention found age, educational status, marital status, social support, perception to the illness (depression) and attitude were significant factors of intention to seek help at a p-value less than or equal to 0.2. We did not enter educational status, gender, ethnicity, religion, perceived severity of depression to the multiple linear regression since p value greater than 0.2. In the multiple linear regression model age, the participant attitude towards seeking professional help, perceiving depression needs treatment, married individuals and moderate and poor social support significantly associated with an intention to seek help for depression (Table 4).
Discussion
This case vignette based assessment of intention to seek help showed that 592 (71.2%) of the respondents had an intention to seek professional help if they were having depression. Of the 832 participants’ mean score of intention to seek help from any health professional was 3.72 (SD = 1.23) with a range of (1) very unlikely to (5) very likely. Implying that the majority of the respondents, 71.2%: 95% CI (68.3%, 74.3%) said they are likely or very likely to seek help after presenting them a vignette depicting an individual experiencing MDD and asking them to report their intention to seek care if confronted with a similar situation. This is similar to the study conducted in China which is 69.6% [23]. It is also similar to a study conducted in Botswana in which participants were likely to seek help from a health professionals for depression [24].
Attitude plays a great role in predicting help seeking intention from a health professional for depression. In this study, attitude was a statistically significant factor for intention to seek help about depression and the finding was supported by a study conducted in Botswana [24] and among Latino immigrants, Mexico [22]. Our result was also similar to New Zealand’s study, with favorable attitudes were related to higher help seeking intentions [25]. The more positive attitude of the participants to depression care, they intent to seek help from professional will be increased. It might be because of individuals with a positive attitude about depression may disclose their illness to health professionals or positive beliefs that professional help is useful which brings a positive attitude.
In this study intention to seek help predicted by age. As age increases health professionals are very important to seek help than family [26]. For young people, the main barriers to seeking help were embarrassment or concern about what others might think [27]. Older age predicted a survey study conducted in England suggest that stronger intention to seek help [28], New Zealand with older adults have a positive attitude to seek professional help for mental illness [25]. As age increase identifying, describing and managing their emotion (emotional competence) may be increased [26]. It might also be because of as age increase depression is not perceived as minor and need the help of health professionals when compared to low in an age in which parents or other adults preferred to seek treatment.
There was a negative association between moderate and poor social support and help-seeking intention. When moderate and poor social support increased, help-seeking intention decreased by 0.30, 0.40 respectively. It might be due to support close to the individual increases attitude and intention to seek help [29]. It might also be due to family members worry could be a factor or influence in whether or not someone would consider seeking help.
There was also a negative association between being married and help-seeking intention and this finding is in contrary to China’s finding [23] in which being married positively associated to seeking help from health professionals. The difference may be in this study married individuals may prefer to seek help from their couple instead of health professionals. The other explanation could be in Chinese study they include the depressed patients.
A unit increase in an intention to seek help from the health professional when participants perceived depression needs treatment. It might be due to people may understand and perceive the illness is very severe and health professionals more helpful than other options. It might be also due to illness causal belief variation. People with physical illness causal beliefs may intent to seek help from health professionals because they may think the problem could not improve by itself spontaneously. As a result, a variety of treatment may need including consulting modern health professionals. This is supported by North-western Ethiopia study on perceptions of mental and physical illnesses [12].
The limitation to this study was that participants did not consider whether or not they have depression. Because participants’ intention to seek help from health professionals might be different when they have depression or do not have depression. The other limitation was the study does not considered perceived stigma and previous help seeking behavior.
The strength of the study was including a relatively large sample size and sampling methods.
Conclusion
Intention to seek professional help for depression was fairly high considering the socio-cultural characteristics and the belief systems of the community in the study area. Increasing age, holding a favorable attitude towards depression and perceived need for biomedical treatment were the driving forces for intention to seek professional help. On the other hand the perception that one receives poor social support is a barrier to help-seeking persuasive communication to change the attitude of younger adults towards depression may improve help-seeking. For future researchers we recommend that comparative study on intention to seek help among non-depressed and depressed individuals to see their intention to seek help from health professionals. Further increase awareness about depression to community is better to seek help from health institution.
Abbreviations
- CI:
-
confidence interval
- DALY:
-
disability adjusted life year
- EPI Info:
-
epidemiological information
- GBD:
-
Global Burden of Disease
- GHSQ:
-
general help seeking questionnaire
- GP:
-
general practitioner
- ICCMH:
-
Integrated Clinical and Community Mental Health
- IPQ:
-
Illness Perception Questionnaire
- MDD:
-
major depressive disorder
- SD:
-
standard deviation
- SPSS:
-
statistical package for social science
- UoG:
-
University of Gondar
- YLDs:
-
years lived with disability
- WHO:
-
World Health Organization
References
Kermode M, Bowen K, Arole S, Joag K, Jorm AF. Community beliefs about treatments and outcomes of mental disorders: a mental health literacy survey in a rural area of Maharashtra, India. Public Health. 2009;123(7):476–83.
Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet. 2013;382(9904):1575–86.
World Health Organization. Mental health facing the challenges bsrfWEmc. In: Mental health facing the challenges, building solutions report from WHO European ministerial conference. Copenhagen, Denmark. 2005.
World Health Organization. The World Health Report 2001: Mental health: new understanding, new hope: World Health Organization; 2001.
Marcus M, Yasamy T, Van Ommeren M, Chisholm D, Saxena S. Depression—a global public health concern 2012. World Health Organization. 2014. http://www.who.int/mental_health/management/depression/who_paper_depression_wfmh_2012.pdf.
Jorm AF. Does old age reduce the risk of anxiety and depression? A review of epidemiological studies across the adult life span. Psychol Med. 2000;30(1):11–22.
Abdulahi H, Mariam D, Kebede D. Burden of disease analysis in rural Ethiopia. Ethiop Med J. 2001;39:271–81.
Van Voorhees BW, Fogel J, Houston TK, Cooper LA, Wang N-Y, Ford DE. Attitudes and illness factors associated with low perceived need for depression treatment among young adults. Soc Psychiatry Psychiatr Epidemiol. 2006;41(9):746–54.
Coppens E, Van Audenhove C, Scheerder G, Arensman E, Coffey C, Costa S, et al. Public attitudes toward depression and help-seeking in four European countries baseline survey prior to the OSPI-Europe intervention. J Affect Disord. 2013;150(2):320–9.
Martínez-Hernáez A, DiGiacomo S, Carceller-Maicas N, Correa-Urquiza M, Martorell-Poveda MA. Non-professional-help-seeking among young people with depression: a qualitative study. BMC Psychiatry. 2014;14:124.
Barney LJ, Griffiths KM, Jorm AF, Christensen H. Stigma about depression and its impact on help-seeking intentions. Aust N Z J Psychiatry. 2006;40(1):51–4.
Mesfin Samuel Mulatu. Perceptions of mental and physical illnesses in North-western Ethiopia: causes, treatments, and attitudes. J Health Psychol. 1999;4(4):531–49.
Deribew A, Tamirat YS. How are mental health problems perceived by a community in Agaro town? Ethiop J Health Dev. 2005;19(2):153–9.
Shibre T, Negash A. Perception of stigma among family members with schizophrenia and major affective disorders in rural Ethiopia social psychiatry. Psychiatry Epidemiol. 2002;36:299–303.
Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: an introduction to theory and research. Reading, MA: Addison-Wesley; 1975.
Bishaw M. Promoting traditional medicine in Ethiopia: a brief historical review of government policy. Soc Sci Med. 1991;33(2):193–200.
Alem ADM, Araya M. Mental health in Ethiopia. Ethiop J Health Dev. 1995;9:47–62.
Ajzen I. The theory of planned behavior. Organizational behavior and human decision processes. 1991;50(2):179–211.
Rickwood D, Deane F, Wilson CJ, Ciarrochi J. Young people’s help-seeking for mental health problems. Aust e-J Adv Mental Health. 2005;4(3):218–51.
Lloyd KR, Jacob K, Patel V, Louis LS, Bhugra D, Mann A. The development of the Short Explanatory Model Interview (SEMI) and its use among primary-care attenders with common mental disorders. Psychol Med. 1998;28(5):1231–7.
Seyfi F, Poudel KC, Yasuoka J, Otsuka K, Jimba M. Intention to seek professional psychological help among college students in Turkey: influence of help-seeking attitudes. BMC Res Notes. 2013;6:519.
Abiola T, Udofia O, Zakari M. Psychometric properties of the 3-item oslo social support scale among clinical students of Bayero University Kano, Nigeria. Malaysian J Psychiatry. 2013;22(2):32–41.
Chin WY, Chan KT, Lam CL, Lam TP, Wan EYF. Help-seeking intentions and subsequent 12-month mental health service use in Chinese primary care patients with depressive symptoms. BMJ Open. 2015;5(1):e006730.
Pheko MM, Chilisa R, Balogun SK, Kgathi C. Predicting intentions to seek psychological help among Botswana University Students: the role of stigma and help-seeking attitudes. SAGE Open. 2013. https://doi.org/10.1177/2158244013494655.
James SA, Buttle H. Attitudinal differences towards mental health services between younger and older New Zealand adults. N Z J Psychol. 2008;37(3):33–43.
Ciarrchi J, Wilson CJ, Deane FP, Rickwood D. Do difficulties with emotions inhibit help-seeking in adolescence? The role of age and emotional competence in predicting help-seeking intentions. Couns Psychol Q. 2003;16(2):103–20.
Jorm AF, Wright A, Morgan AJ. Where to seek help for a mental disorder? Med J Aust. 2007;187(10):556–60.
Rusch N, Evans-Lacko SE. Knowledge and attitudes as predictors of intentions to seek help for and disclose a mental illness. Psychiatr Serv. 2011;62(6):675–8.
David L, Wade NG, Wester SR, Larson L, Ashley H. Seeking help from a mental health professional: the influence of one’s social network. J Clin Psychol. 2007;63:233–45.
Authors’ contributions
SS developed the proposal, supervised the data collection, analyzed the data and wrote the draft manuscript. TA and GA revised the proposal, checked the data analysis, and revised the manuscript. DA, TA and WG revised the proposal and assist the data analysis. All authors read and approved the final manuscript.
Acknowledgements
The authors acknowledge University of Gondar and Amanuel Mental Specialized Hospital for funding the study. We extend our gratitude to data collectors, supervisors and study participants for their time and effort.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets used for current study are available from the corresponding author on reasonable request (shumetshegaye@yahoo.com).
Consent for publication
Not applicable.
Ethics approval and consent to participate
The ethical review board of the University of Gondar and Amanuel Mental Specialized Hospital initially approved the study proposal. A formal letter of permission obtained and submitted to the respective town administration. We obtained informed consent from participants after explaining the purpose of the study and if they were voluntary, they would put their signature for that idea was their own and confidentiality maintained by omitting their personal identification.
Funding
The funder has no role in collection, analysis and interpretation of data and in writing the manuscript.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Shumet, S., Azale, T., Ayano, G. et al. Intention to seek help for depression and associated factors among residents of Aykel town, Northwest Ethiopia: cross-sectional study. Int J Ment Health Syst 13, 18 (2019). https://doi.org/10.1186/s13033-019-0274-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13033-019-0274-y