Abstract
Background
The higher prevalence of smoking among psychiatric patients is well established. However, gender-specific associations have rarely been the focus of studies among patients with various psychiatric disorders. The aim of this study was to estimate the gender-specific prevalence of current smoking by psychiatric patients and its association with various psychiatric disorders and the use of psychotropic medications.
Methods
A cross-sectional observational study was performed between July 2012 and June 2014. Patients were recruited from six hospitals located in the five regions of Saudi Arabia.
Results
Of the 1193 patients, 402 (33.7%) were current smokers. The incidence of current smoking was much higher among males than females (58.3% versus 6.7%, p < 0.001). In one or both genders, current smoking was associated with marital status, education, family income, residence, obesity, physical activity, substance abuse, inpatient status, previous psychiatric hospitalization, and age at onset of psychiatric illness. In both gender, smoking was higher in patients who had a secondary psychiatric disorder (66.7% versus 37.5%, respectively), those who had a primary psychotic disorder (63.7% versus 12.3%), and those taking antipsychotic medication (64.1% versus 8.3%) but lower in patients who had a primary depressive disorder (40.3% versus 4.3%), those who had a primary anxiety disorder (45.8% versus 0.0%), and those taking antidepressant medications (53.7% versus 3.6%). In a multivariate analysis adjusted for demographic/clinical characteristics and psychiatric disorders, current smoking was independently associated with primary psychotic disorders in females (OR = 3.47, 1.45–8.27, p = 0.005) but not in males. In a multivariate analysis adjusted for demographic/clinical characteristics and psychotropic medications, current smoking was independently associated with antipsychotic medication use in males (OR = 1.79, 1.10–2.93, p = 0.020). Current smoking was strongly associated with substance abuse in both univariate and multivariate analyses.
Conclusion
The prevalence of current smoking is high with marked gender difference in a large sample of mixed psychiatric patients in Saudi Arabia. Smoking-cessation programs may be urgently needed for these vulnerable patients.
Similar content being viewed by others
Background
Smoking is a global health risk with a well-established serious morbidity and mortality profile. In 2015, the World Health Organization (WHO) estimated that more than 1 billion people smoke tobacco worldwide, resulting in approximately 6 million deaths per year [1]. In Saudi Arabia, the average prevalence of current tobacco smoking among adults was estimated at 22.6%, with a wide range (11.6–52.3%) reported by studies targeting diverse populations [2]. Interestingly, there is a striking difference in the smoking rates between males (26%) and females (3–9%) in Saudi Arabia [2, 3]. This may partially explain the higher smoking rates found in several studies that included only males, for example, 35% in a military population [4] and 34–52% among male patients at primary care centers [5, 6].
Systematic reviews and other types of reviews have found a positive association between smoking and psychiatric disorders [7, 8], especially among females and in younger population [9]. For example, the prevalence of smoking has been reported to be two- to threefold higher among psychiatric patients than in the general population [10,11,12,13]. In addition, smokers have been found to have two- to threefold higher risk of developing psychiatric illness and substance use disorders later in life [14]. Moreover, smoking by psychiatric patients is associated with greater disability and poorer quality of life [15]. The impact of smoking on mortality among psychiatric patients is believed to be even greater than that in the general population, probably because of the excess mortality from cardiovascular diseases, stroke, and respiratory cancers among these patients [16]. The impact on mortality is complicated by the effects of smoking on some psychiatric symptoms, which makes cessation more challenging in these patients [17].
Although a higher smoking prevalence among psychiatric patients is well established, the overall impact is probably affected by several patient factors, including sociodemographic profile, type, and number of psychiatric disorders, pharmacological therapies, and concomitant substance abuse [8, 18,19,20,21]. The complex interplay of these factors in different populations complicates comparisons between studies. The objective of the current study was to estimate the prevalence of current smoking in a mixed psychiatric population in Saudi Arabia and examine the effect of the above factors on smoking rates. Suitable data from Saudi Arabia are very limited and outdated, and they lack adjustment for several confounders [22]. In addition, the impact of gender, which has received little attention in Western research, cannot be ignored in our population because of the substantial gender-specific difference in smoking prevalence. Therefore, we examined gender-specific associations between smoking and psychiatric disorders.
Methods
Setting
The current study was conducted among patients seeking psychiatric treatment in both inpatient and outpatient psychiatric healthcare services at several hospitals located in the Central, Eastern, Western, Northern, and Southern regions of Saudi Arabia. We aimed to select the largest mental hospital in each of these five major regions. However, because of logistical difficulties, not all the included hospitals were the largest in their region. To compensate, two hospitals were selected from the central region. The final hospitals were King Saud University Medical City in Riyadh and Zulfi General Hospital (Central region), Jeddah Mental Health Hospital (Western region), Al Amal Complex for Mental Health—Dammam (Eastern region), Aljouf Mental Health Hospital (Northern region), and Abha Mental Health Hospital (Southern region). King Saud University Medical City is a university-affiliated governmental hospital, whereas the other hospitals are service based and operate under the authority of the Ministry of Health. All included hospitals provide free psychiatric inpatient and outpatient healthcare services.
Study design
A cross-sectional observational study was performed between July 2012 and June 2014.
Population
Consecutive male and female patients seeking psychiatric treatment from the included hospitals over the study period were asked to join the study. Those who provided informed consent were included, irrespective of the type or duration of their psychiatric disorder or recent use of psychotropic medications. Patients whose records and interviews indicated an absence of psychiatric illness (n = 59) or lack of smoking status (N = 15) were excluded. Therefore, 1193 of the 1264 initial patients were included in the analysis.
Data collection
A mini-interview form was developed that included sociodemographic characteristics, medical history, current psychiatric disorders, and recent use of psychotropic medications. Data were obtained primarily by reviewing the patients’ charts. The diagnosis of psychiatric disorders in this study was based on routine clinical interviews. The psychiatric consultants in-charge in each study site made psychiatric diagnoses of their patients using the Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision (DSM-IV-TR) criteria. The psychiatric diagnoses were confirmed by the treating teams, primarily following longitudinal evaluation and follow-up in the psychiatric setting. Unclear or missing information was clarified or obtained by interviewing the patient and/or his or her family. Trained psychiatric residents/staff were in charge for reviewing the chart and conducting the mini-interviews with the patients and/or their families. The purpose of these mini-interviews was to gather any unclear or missing information except for the major clinical data like psychiatric diagnoses and treatments which are certainly documented in the patients’ charts.
The smoking status was determined during the mini-interview using face-to-face questions in Arabic language. Patients were asked to define their cigarette smoking status as a current smoker, a previous smoker (i.e., someone who has smoked greater than 100 cigarettes in their lifetime but has not smoked at least in the last month), or a never-smoker [23].
Classification of psychiatric disorders
To analyze the data, the psychiatric diagnoses made by the primary psychiatrist for each patient using DSM-IV-TR criteria were classified into 8 categories [24, 25]: Primary psychotic disorders included schizophrenia, schizoaffective disorder, delusional disorder, and brief psychotic disorder. Primary bipolar disorders included bipolar disorder types I and II. Primary depressive disorders included major depressive disorder and dysthymic disorder. Primary anxiety disorders included generalized anxiety disorder, obsessive–compulsive disorder, social anxiety disorder, specific phobia, panic disorder, post-traumatic stress disorder, and acute stress disorder. Personality disorders included personality disorder not otherwise specified (mixed personality disorder), paranoid personality disorder, antisocial personality disorder, and borderline personality disorder. Secondary psychiatric disorders included psychotic disorder due to another medical condition, depression due to another medical condition, dementia, substance abuse, and substance-induced depressive disorder. Other disorders included undifferentiated somatoform disorder, conversion disorder, mental retardation, attention deficit hyperactivity disorder, dissociative disorder, primary insomnia, adjustment disorder, enuresis disorder, trichotillomania, and anorexia nervosa. Multiple disorders included two or more of the psychiatric illnesses listed above.
Classification of psychotropic medications
Both individual psychotropic medications and pharmacologic groups were used in the analysis. These included antipsychotics (low potency first generation, high potency first generation, and second generation), antidepressants (e.g., selective serotonin reuptake inhibitors (SSRIs) and tricyclics), mood stabilizers, and antianxiety medications.
Statistical analysis
Categorical data are presented using frequencies and percentages, and continuous data are presented using means and standard deviations (SD). Because of the marked difference in smoking prevalence by gender, analysis was completed separately for males and females. As there were very few differences between previous and never-smokers as regards psychiatric disorders and use of psychotropic medications, patients were categorized as either current smokers or non-current smokers (including previous and never-smokers) to simplify data interpretation. Significant differences between current and non-current smokers with regard to demographics, clinical characteristics, disorders, and medications were tested. Categorical data were tested using the χ2 test or Fisher’s exact test (as appropriate), and continuous data were tested using Student’s t test or the Mann–Whitney U test (as appropriate). Independent associations of current smoking status with different psychiatric disorders and psychotropic medications, after adjusting for relevant demographic and clinical characteristics, were evaluated using multivariate logistic regression models with stepwise backward elimination. Smoking in small-sized groups with sample size < 20 or with zero smoking prevalence (as those with hypothyroidism) were excluded from the model to avoid instability (very huge or zero odds ratio). All p values were two-tailed. p < 0.05 was considered significant. SPSS software (release 20.3, Armonk, NY: IBM Corp) was used for all statistical analyses.
Results
Prevalence of current smoking
A total of 1193 patients (624 males and 569 females) were included in the analysis; 799 (67.0%) outpatients and 394 (33.0%) inpatients. Of the total group, 402 (33.7%) patients were current smokers, 137 (11.5%) were previous smokers, and 654 (54.8%) were never-smokers. The prevalence of smoking, either currently or previously, was much higher among males (58.3 and 17.6%, respectively) than females (6.7 and 4.7%, respectively), and the difference was statistically significant (p < 0.001). In addition, the prevalence of current smokers was significantly higher among inpatients than among outpatients (44.2% versus 28.5%, p < 0.001, Fig. 1).
Demographic characteristics and smoking
The average age was 38.0 ± 13.0 years, and more than half (54.3%) of the patients were unmarried (Table 1). The majority were either illiterate or had less than a secondary education (87.1%), were non-working (71.2%), had a monthly family income of 6000 SR or less (62.0%), and were living in urban communities (80.4%). Approximately 37.9% of the patients were obese, and the majority (87.3%) were physically inactive. The sociodemographic characteristics associated with current smoking varied by gender. In males, higher rates of current smoking (average 58.3%) were significantly associated with being unmarried (p < 0.001), having a secondary education or less (p < 0.001), having lower family income (p = 0.009), living in a village (p = 0.004), and being non-obese (p = 0.010). In females, higher rates of current smoking (average 6.7%) were significantly associated with having a secondary education or less (p = 0.010) and being physically active (p = 0.017, Table 1).
Clinical characteristics and smoking
The average age at onset of psychiatric illness was 28.3 ± 12.0 years, with average illness duration of 9.7 ± 9.3 years (Table 2). Approximately 24.4% of the patients have substance abuse disorder. Almost half (46.0%) had had an average of 3.8 ± 4.4 previous psychiatric hospitalizations. Common comorbidities included diabetes and hypertension. In both males and females, higher rates of current smoking were significantly associated with substance abuse (p < 0.001 each), inpatient status (p = 0.001 and p = 0.041, respectively), and previous psychiatric hospitalization (p < 0.001 and p = 0.004, respectively), as well as—in females only—a younger age at onset of psychiatric illness (p = 0.039, Table 2).
Psychiatric disorders/medications and smoking
The majority of patients had a single psychiatric disorder (90.4%): mainly primary psychotic disorders (41.2%), primary depressive disorders (16.8%), and primary bipolar disorders (15.3%, Table 3). The majority of patients were using two or more psychotropic medications (66.5%): primarily antipsychotics (76.7%), antidepressants (41.6%), and mood stabilizers (27.8%). For both males and females, higher rates of current smoking were positively associated with primary psychotic disorders (p = 0.004 and p = 0.001, respectively) and antipsychotic medications (p < 0.001 and p = 0.004, respectively) but negatively associated with primary anxiety disorders (p = 0.040 and p = 0.009, respectively) and antidepressant medications (p = 0.021 and p = 0.012, respectively). In addition, higher rates of current smoking were positively associated with the use of multiple psychotropic medications in males (p = 0.004) and secondary psychiatric disorders in females (p = 0.012) but negatively associated with primary depressive disorders in males (p = 0.002, Table 3).
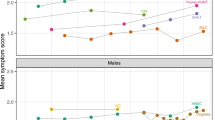
In both males and females, the prevalence of current smoking was higher among patients using antipsychotic medications alone or combined with antidepressant medications and was the lowest among those not using any psychotropic medication or using antidepressant medications alone (p = 0.001 and p = 0.015, respectively, Fig. 2). At least two-thirds of male patients using mirtazapine, carbamazepine, risperidone, paliperidone, or venlafaxine were current smokers. Moreover, risperidone and olanzapine were associated with a higher prevalence of current smoking in females.
Independent associations of smoking
Multivariate logistic regression analysis models tested the association of current smoking with different psychiatric disorders and the use of different psychotropic medications after adjusting for significant gender-specific demographic, clinical, and behavioral characteristics (Tables 1 and 2). They included marital status, educational level, family income, type of residential area, obesity, physical activity, hospitalization status, previous psychiatric hospitalization, and substance abuse (Table 4). In models additionally adjusted for psychiatric disorders, but not for psychotropic medications, current smoking was independently associated with primary psychotic disorders in females (OR = 3.47, 1.45–8.27, p = 0.005), but not in males, and with substance abuse in both males (OR = 5.28, 3.52–7.93, p < 0.001) and females (OR = 10.56, 3.78–29.53, p < 0.001). In addition, education and lower family income were independently associated with current smoking in males. In models additionally adjusted for psychotropic medications but not psychiatric disorders, current smoking was independently associated with antipsychotic medications in males (OR = 1.79, 1.10–2.93, p = 0.020) and marginally associated in females (OR = 4.68, 0.95–22.95, p = 0.057) and with substance abuse in both males (OR = 5.18, 3.39–7.92, p < 0.001) and females (OR = 14.15, 4.32–46.35, p < 0.001). In addition, lower family income was independently associated with current smoking in females (Table 4).
Discussion
We found a high prevalence of current smoking in a large sample of psychiatric outpatients and inpatients in Saudi Arabia. As in the general Saudi population—although at a higher rate—smoking prevalence was much higher among males than females (58% versus 7%). This was almost double the rate of current smoking recently reported by the WHO for the general Saudi population (26% in males and 3% in females) [3]. However, the prevalence we found was almost identical to the current smoking rates (58%) reported among 505 male outpatients recruited from five hospitals in Saudi Arabia in 1996 and 1997 [22]. Unfortunately, females were not included in the previous study, which reported the only published data regarding smoking by psychiatric patients in Saudi Arabia [22]. Several hypotheses have been suggested to explain the higher smoking rates among psychiatric patients [8, 26]. The most widely accepted hypothesis is self-medication; that is, patients smoke to reduce the impact of specific psychiatric disorders and medications [8, 17, 20, 26]. Other hypotheses include shared genetic factors that control the susceptibility for both smoking and psychiatric disorders and shared environmental factors, such as stress, that can increase the incidence of both smoking and psychiatric illness [8, 26].
Higher rates of current smoking among male psychiatric patients is consistent with the findings of nearly all Western and Eastern studies [20, 27,28,29,30,31,32]. For example, male versus female rates have been reported as 66% versus 56% in the US [32], 69% versus 48% in France [20], 32% versus 21% in Japan [29], 59% versus 41% in Brazil [28], and 78.4% versus 36.2% in Iran [30]. However, a very large male–female difference, as found in the current study, has been reported in only a few Eastern countries, such as India (53% versus 9%) [31] and Bahrain (47% versus 4%) [27]. This reflects the variability in gender-specific rates of current smoking in the general population of Western and Eastern countries [33]. Smoking among females in a conservative society such as Saudi Arabia could be perceived as impairing the feminine Islamic image of women [2, 34]. Another explanation is that it is more inconvenient for females to obtain cigarettes and find a place to smoke [34]. However, we cannot exclude the possibility that current smoking by female patients is under-reported as a consequence of its social stigma [2]. Interestingly, the persistence of a marked gender difference in smoking rates among our patients, after stratifying by psychiatric disorder and psychotropic medication, might indicate that the gender effect is independent of the psychiatric impact. In addition, the persistence of sociodemographic risk factors for smoking (such as low education, low income, and being unmarried) in a multivariate analysis, especially in men, is more evidence that the motivations for smoking in the general population [4, 35] are the same as those in psychiatric patients [5, 36, 37]. The disappearance/attenuation of sociodemographic risk factors for smoking in multivariate analysis among females could be related to the low prevalence of smoking among this group rather than real lack of associations.
As found in previous studies, smoking rates in the current study were highest among patients with substance abuse disorder [26, 29]. In addition, current smoking and substance abuse were strongly and independently associated, even after adjusting for psychiatric disorder or psychotropic medication [36, 37]. This may further explain the high smoking prevalence among those with secondary psychiatric disorders in the current and previous studies [20, 22, 28]. A large twin study showed that shared genetic and, to a lesser extent, environmental risk factors predispose individuals to lifetime comorbidity of common psychiatric and substance abuse disorders [38].
Although attenuated in multivariate analyses, smoking in the current study was strongly associated with primary psychotic disorders and/or use of antipsychotic medications. High smoking rates among patients with schizophrenia/schizoaffective disorders have been consistently reported in previous studies: 66–74% in previous studies [12, 18, 20, 22, 32, 36] compared to 64% in the current study. Higher smoking rates were also reported among patients using antipsychotic medications [20]. It has been suggested that smoking reduces the intensity of some psychiatric symptoms and improves cognitive and concentration functions in patients with schizophrenia [8, 39, 40]. However, smoking is also associated with an increased risk of psychosis and an earlier age at onset of psychotic illness [41]. In addition, smoking was reported to reduce the side effects of antipsychotic medications, especially extrapyramidal manifestations [40, 42]. Yet, smoking can have effects on the metabolism of antipsychotic medications, especially clozapine and olanzapine, such as decreasing their blood levels and increasing the clinically effective dose [43]. Therefore, it has been suggested that doses of clozapine and olanzapine be increased by 50 and 30%, respectively, for smokers to attain an equivalent clozapine or olanzapine blood concentration [44]. The complex association between smoking and schizophrenia, as well as antipsychotic medications, can make smoking cessation challenging and cause sudden withdrawal symptoms [17, 43]. Interestingly, the lower smoking rates among patients with primary depressive disorders and/or those using antidepressant medications, which were determined in univariate analysis in the current study, have been previously reported [20, 30, 31, 36]. Although it may be difficult to explain, the fact that the majority of our patients who were not using antidepressants were using antipsychotics may partially explain the relatively lower smoking rates among patients using antidepressant medications. In addition, the apparently beneficial effects of smoking observed in patients treated with antipsychotics are lacking among patients treated with antidepressants. In the other hand, except of bupropion and nortriptyline, evidence suggests that most antidepressants has no antismoking effect [45].
Several clinical guidelines recommend giving higher priority to providing smoking-cessation advice in everyday clinical practice to patients with a mental health diagnosis [46,47,48]. A recent systematic review found that people with severe mental illness receive smoking-cessation advice about as often as people without mental illness do, whereas those with non-severe mental illness are slightly more likely to receive smoking-cessation advice compared with people without mental illness [48]. In addition to the benefits of smoking cessation in decreasing morbidity and mortality in people with psychiatric disorders [46], smoking cessation is also associated with reduced depression, anxiety, and stress, and improved positive mood and quality of life to the same extent for those with psychiatric disorders as for those without [49]. The big positive effect-size after smoking cessation in both those with or without psychiatric disorders may indicate the common personal and social motives of smoking in both groups [49]. However, traditional smoking-cessation programs may need to be tailored to fit the neuropsychological profile of psychiatric patients [50]. The European Psychiatric Association provides seven recommendations regarding the core components of the diagnostics and treatment of tobacco dependence in adults with mental illness [46]: (1) the process for recording smoking status, (2) the timing of the intervention, (3) counseling, (4) drug treatment using a first-line product (e.g., nicotine replacement therapy, varenicline, bupropion), (5) contacting the patient soon after cessation, (6) follow-up visits, and (7) relapse prevention and management [46].
The current study makes several important contributions. It is the first study in Saudi Arabia to estimate the gender-specific prevalence of current smoking and to determine its independent risk factors among male and female psychiatric patients. The mixed population and the relatively large sample size enabled us to examine the association of current smoking with a wide variety of psychiatric disorders and psychotropic medications. Previous studies focused primarily on antipsychotics and rarely on the variability of smoking rates among patients taking different groups of psychotropic medications. However, we acknowledge several limitations. First, the use of convenience sampling may limit the generalizability of our findings to psychiatric patients in Saudi Arabia. The cross-sectional design did not enable us to ascertain causality between psychiatric disorders or psychotropic medications and current smoking. Finally, although cigarette smoking is by far the most common type of smoking in Saudi Arabia, the findings of the current study do not reflect other types of tobacco smoking.
Conclusion
We found a high prevalence of current smoking among a large sample of psychiatric patients in Saudi Arabia. As in the general population, there is a striking gender difference in smoking rates. In addition to sociodemographic risk factors for smoking, substance abuse, psychotic disorders, and antipsychotic medications are strong independent associates. The current findings suggest an urgent need for smoking-cessation programs for these vulnerable patients as well as for further studies to test the effectiveness of such programs.
Abbreviations
- OR:
-
odds ratio
- WHO:
-
World Health Organization
- DSM-IV-TR:
-
Diagnostic and Statistical Manual of Mental Disorders, fourth edition, text revision
References
World Health Organization. WHO global report on trends in prevalence of tobacco smoking 2015. WHO Mag. 2015. www.who.int/about/licensing/copyright_form/en/index.html. Accessed 27 Feb 2018.
Bassiony MM. Smoking in Saudi Arabia. Saudi Med J. 2009;30:876–81.
WHO. WHO global report on trends in tobacco smoking 2000–2025. Geneva: World Health Organization; 2015.
Al-Khashan HI, Al Sabaan FS, Al Nasser HS, Al Buraidi AA, Al Awad AD, Horaib GB, et al. The prevalence of smoking and its associated factors among military personnel in Kingdom of Saudi Arabia: a national study. J Fam Community Med. 2014;21:147–53.
Al-Haddad NS, Al-Habeeb TA, Abdelgadir MH, Al-Ghamdy YS, Qureshi NA. Smoking patterns among primary health care attendees, Al-Qassim region, Saudi Arabia. East Mediterr Health J. 2003;9:911–22.
Siddiqui S, Ogbeide DO, Al Khalifa I. Smoking in a Saudi community: prevalance, influencing factors, and risk perception. Fam Med. 2001;33:367–70.
Gurillo P, Jauhar S, Murray RM, MacCabe JH. Does tobacco use cause psychosis? Systematic review and meta-analysis. Lancet Psychiatry. 2015;2:718–25.
Aubin HJ, Rollema H, Svensson TH, Winterer G. Smoking, quitting, and psychiatric disease: a review. Neurosci Biobehav Rev. 2012;36:271–84.
Lawrence D, Mitrou F, Zubrick SR. Smoking and mental illness: results from population surveys in Australia and the United States. BMC Public Health. 2009;9:285. http://bmcpublichealth.biomedcentral.com/articles/10.1186/1471-2458-9-285. Accessed 25 Feb 2017.
Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. JAMA. 2000;284:2606–10.
Ma X, Xiang YT, Cai ZJ, Li SR, Xiang YQ, Guo HL, et al. Smoking and psychiatric disorders in the rural and urban regions of Beijing, China: a community-based survey. Drug Alcohol Depend. 2009;100:146–52.
Döme P, Rihmer Z, Gonda X, Pestality P, Kovács G, Teleki Z, et al. Cigarette smoking and psychiatric disorders in Hungary. Int J Psychiatry Clin Pract. 2005;9:145–8.
Lineberry TW, Allen JD, Nash J, Galardy CW. Population-based prevalence of smoking in psychiatric inpatients: a focus on acute suicide risk and major diagnostic groups. Compr Psychiatry. 2009;50:526–32.
John U, Meyer C, Rumpf H-J, Hapke U. Smoking, nicotine dependence and psychiatric comorbidity—a population-based study including smoking cessation after three years. Drug Alcohol Depend. 2004;76:287–95.
Schmitz N, Kruse J, Kugler J. Disabilities, quality of life, and mental disorders associated with smoking and nicotine dependence. Am J Psychiatry. 2003;160:1670–6. http://www.ncbi.nlm.nih.gov/pubmed/12944344. Accessed 25 Feb 2017.
Osborn DPJ, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s General Practice Research Database. Arch Gen Psychiatry. 2007;64:242–9. http://archpsyc.jamanetwork.com/article.aspx?articleid=482163&resultClick=1. Accessed 19 Nov 2015.
Fagerström K, Aubin HJ. Management of smoking cessation in patients with psychiatric disorders. Curr Med Res Opin. 2009;25:511–8.
Cristina LO, Carlos R, Laia M, Miguel C. Smoking in affective psychosis: review about nicotine use in bipolar and schizoaffective disorders. Adicciones. 2011;23:65–75.
Ch T, Kardaras K, Kontaxakis V. Smoking in patients with psychiatric disorders: effects on their psychopathology and quality of life. Psychiatrike. 2008;19:306–12.
Poirier MF, Canceil O, Baylé F, Millet B, Bourdel MC, Moatti C, et al. Prevalence of smoking in psychiatric patients. Prog Neuropsychopharmacol Biol Psychiatry. 2002;26:529–37.
Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: a population-based prevalence study. JAMA. 2000;284:2606–10. http://www.ncbi.nlm.nih.gov/pubmed/11086367. Accessed 25 Feb 2017.
Al-Habeeb TA, Qureshi NA. Smoking among male psychiatric outpatients in Saudi Arabia. Ann Saudi Med. 2000;20:218–23.
The Centers for Disease Control and Prevention (CDC). The national health interview survey. Adult tobacco use information. https://www.cdc.gov/nchs/nhis/tobacco/tobacco_glossary.htm. Accessed 27 Feb 2018.
Hales RE, Yudofsky SC, Gabbard GO, American Psychiatric Publishing. The American psychiatric publishing textbook of psychiatry. Washington, D.C.: American Psychiatric Publishing; 2008.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Washington, D.C.: American Psychiatric Association; 2000.
Kalman D, Morissette SB, George TP. Co-morbidity of smoking in patients with psychiatric and substance use disorders. Am J Addict. 2005;14:106–23.
Hamadeh RR, Al Ansari A, Jahrami H, Al Offi A. Cigarette and waterpipe smoking among adult patients with severe and persistent mental illness in Bahrain: a comparison with the national non-communicable diseases risk factors survey. BMC Res Notes. 2016;9:77.
Barros FCRD, Melo APS, Cournos F, Cherchiglia ML, Peixoto ERDM, Guimarães MDC. Cigarette smoking among psychiatric patients in Brazil. Cad Saude Publica. 2014;30:1195–206.
Umene-Nakano W, Yoshimura R, Hoshuyama T, Yoshii C, Hayashi K, Nakano H, et al. Current smoking rate in patients with psychiatric disorders in Japan: questionnaire survey. Psychiatry Res. 2013;210:268–73.
Milani HS, Kharaghani R, Safa M, Samadi R, Farhadi MH, Ardakani MRK, et al. Pattern of smoking and nicotine dependence in patients with psychiatric disorders. Tanaffos. 2012;11:55–60.
Chandra PS, Carey MP, Carey KB, Jairam KR, Girish NS, Rudresh HP. Prevalence and correlates of tobacco use and nicotine dependence among psychiatric patients in India. Addict Behav. 2005;30:1290–9.
Vanable PA, Carey MP, Carey KB, Maisto SA. Smoking among psychiatric outpatients: relationship to substance use, diagnosis, and illness severity. Psychol Addict Behav. 2003;17:259–65.
Hitchman SC, Fong GT. Gender empowerment and female-to-male smoking prevalence ratios. Bull World Health Organ. 89(3):195–202. https://doi.org/10.2471/BLT.10.079905.
Abdalla AM, Al-Kaabba AF, Saeed AA, Abdulrahman BM, Raat H. Gender differences in smoking behavior among adolescents in Saudi Arabia. Saudi Med J. 2007;28:1102–8.
Al-Turki KA, Al-Baghli NA, Al-Ghamdi AJ, El-Zubaier AG, Al-Ghamdi R, Alameer MM. Prevalence of current smoking in Eastern province,Saudi Arabia. East Mediterr Health J. 2010;16:671–6.
Cooper J, Mancuso SG, Borland R, Slade T, Galletly C, Castle D. Tobacco smoking among people living with a psychotic illness: the second Australian survey of psychosis. Aust N Z J Psychiatry. 2012;46:851–63.
Keizer I, Gex-Fabry M, Eytan A, Bertschy G. Smoking in psychiatric inpatients: association with working status, diagnosis, comorbid substance abuse and history of suicide attempts. Addict Behav. 2009;34:815–20.
Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Arch Gen Psychiatry. 2003;60:929.
Morisano D, Wing VC, Sacco KA, Arenovich T, George TP. Effects of tobacco smoking on neuropsychological function in schizophrenia in comparison to other psychiatric disorders and non-psychiatric controls. Am J Addict. 2013;22:46–53.
Winterer G. Why do patients with schizophrenia smoke? Curr Opin Psychiatry. 2010;23:112–9. http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00001504-201003000-00007. Accessed 25 Feb 2017.
Gurillo P, Jauhar S, Murray RM, MacCabe JH. Does tobacco use cause psychosis? Systematic review and meta-analysis. Lancet Psychiatry. 2015;2:718–25. http://www.ncbi.nlm.nih.gov/pubmed/26249303. Accessed 28 Feb 2017.
Barnes M, Lawford BR, Burton SC, Heslop KR, Noble EP, Hausdorf K, et al. Smoking and schizophrenia: is symptom profile related to smoking and which antipsychotic medication is of benefit in reducing cigarette use? Aust N Z J Psychiatry. 2006;40:575–80.
Lowe EJ, Ackman ML. Impact of tobacco smoking cessation on stable clozapine or olanzapine treatment. Ann Pharmacother. 2010;44:727–32.
Tsuda Y, Saruwatari J, Yasui-Furukori N. Meta-analysis: the effects of smoking on the disposition of two commonly used antipsychotic agents, olanzapine and clozapine. BMJ Open. 2014;4:e004216. http://www.ncbi.nlm.nih.gov/pubmed/24595134. Accessed 28 Feb 2017.
Hughes JR, Stead LF, Hartmann-Boyce J, Cahill K, Lancaster T. Antidepressants for smoking cessation. In: Hughes JR, editor. Cochrane database system review. Chichester: Wiley; 2014:CD000031. http://doi.wiley.com/10.1002/14651858.CD000031.pub4. Accessed 19 Mar 2017.
Rüther T, Bobes J, De Hert M, Svensson TH, Mann K, Batra A, et al. EPA guidance on tobacco dependence and strategies for smoking cessation in people with mental illness. Eur Psychiatry. 2014;29:65–82. http://www.ncbi.nlm.nih.gov/pubmed/24485753. Accessed 28 Feb 2017.
Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, Aveyard P. Change in mental health after smoking cessation: systematic review and meta-analysis. BMJ. 2014;348:g1151. http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emed12&NEWS=N&AN=24524926. Accessed 28 Feb 2017.
Mitchell AJ, Vancampfort D, De Hert M, Stubbs B. Do people with mental illness receive adequate smoking cessation advice? A systematic review and meta-analysis. Gen Hosp Psychiatry. 2015;37:14–23.
Taylor G, McNeill A, Girling A, Farley A, Lindson-Hawley N, Aveyard P. Change in mental health after smoking cessation: systematic review and meta-analysis. BMJ. 2014;348:g1151. http://www.ncbi.nlm.nih.gov/pubmed/24524926. Accessed 27 Feb 2018.
Fagerström K, Aubin HJ. Management of smoking cessation in patients with psychiatric disorders. Curr Med Res Opin. 2009;25:511–8. http://www.ncbi.nlm.nih.gov/pubmed/19192999. Accessed 27 Feb 2018.
Authors’ contributions
FA designed the study; supervised the data collection, entry and statistical analysis; and co-wrote the final draft of the manuscript. All other authors participated effectively in most of the stages of this research. All authors read and approved the final manuscript.
Acknowledgements
The authors extend their sincere appreciation and gratefully acknowledge the support they received from the College of Medicine Research Center, Deanship of Scientific Research, King Saud University. Furthermore, the authors express their gratitude to Dr. Nada AlQattan, Ms. Fatima Jama, and Dr. Aiman El-Saed for their assistance in data collection, entry, and analysis respectively.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study received all the required ethical approvals from the institutional review board at the Faculty of Medicine at King Saud University in Riyadh, as well as administrative approvals from the respective hospitals. Written informed consent was given by all patients or their family members, whenever the patient is in a state that does not allow him/her to give consent.
Funding
None.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Alosaimi, F.D., Abalhassan, M., Alhaddad, B. et al. Gender differences and risk factors for smoking among patients with various psychiatric disorders in Saudi Arabia: a cross-sectional study. Int J Ment Health Syst 12, 21 (2018). https://doi.org/10.1186/s13033-018-0201-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13033-018-0201-7