Abstract
Background
Alzheimer’s disease (AD) is ranked as the most prevalent neurodegenerative disease. However, the exact molecular mechanisms underlying pathophysiological alterations in AD remain unclear, especially at the prodromal stage. The decreased proteolytic degradation of Aβ, blood–brain barrier (BBB) disruption, and neuroinflammation are considered to play key roles in the course of AD.
Methods
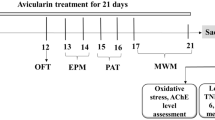
Male APPswe/PS1dE9 C57BL/6 J double-transgenic (APP/PS1) mice in the age range from 1 month to 6 months and age-matched wild type mice were used in this study, intending to investigate the expression profiles of Aβ-degrading enzymes for Aβ degradation activities and zonula occludens-1 (zo-1) for BBB integrity at the prodromal stage.
Results
Our results showed that there were no significant genotype-related alterations in mRNA expression levels of 4 well-characterized Aβ-degrading enzymes in APP/PS1 mice within the ages of 6 months. Interestingly, a significant decrease in zo-1 expression was observed in APP/PS1 mice starting from the age of 5 months, suggesting that BBB disrupt occurs at an early stage. Moreover, treatment of fish oil (FO) for 4 weeks remarkably increased zo-1 expression and significantly inhibited the glial activation and NF-κB activation in APP/PS1 mice.
Conclusion
The results of our study suggest that FO supplement could be a potential therapeutic early intervention for AD through protecting the BBB integrity and suppressing glial and NF-κB activation.
Similar content being viewed by others
Background
Alzheimer’s disease (AD) is the most common neurodegenerative disorder among older population worldwide. Pathological hallmarks of AD include extracellular amyloid plaques and intracellular neurofibrillary tangles in brain regions [1, 2]. A large body of studies suggest that amyloid plaques result from an imbalance between production and clearance of amyloid beta (Aβ) [3, 4]. Aβ can be cleared by a number of pathways in the brain such as enzymatic degradation and recirculation into the blood stream via the blood–brain barrier (BBB) [5]. In the past decades, a series of degrading enzymes have been identified to be able to cleave Aβ either in vitro or in vivo, including cathepsin B (CatB), neprilysin (NEP), insulin-degrading enzyme (IDE), and myelin basic protein (MBP). CatB is specifically implicated as a proteolytic enzyme in degradation of Aβ in vivo [6]. NEP is reported to degrade both monomeric and oligomeric Aβ [7], IDE is concentrated on soluble monomeric clearance [8], and MBP can degrade both monomeric and fibrillary forms of Aβ [9]. Aβ deposit is found not just in AD patients but even in cognitively normal elderly [10], suggesting that Aβ enzymatic degradation might be impaired at the early disease stage. Therefore, it is of interest to investigate the expression profiles of Aβ-degrading enzymes at the prodromal stage of AD.
The BBB acts to limit the molecules exchange between brain and periphery regions mainly relying on tight junction (TJ) structure in BBB endothelial cells, of which destruction could alter brain homeostasis, and lead to brain edema, neuroinflammation, neuron injury, and so on [11]. Zonula occludens-1 (zo-1), as a TJ periphery membrane protein, belongs to the membrane-associated guanylate kinase (MAGUK) family. Zo-1 is a tight junction (TJ) protein, which is essential for maintaining and stabilizing the TJ structure. Decrease of zo-1 could result in BBB integrity injury, which could disturb Aβ clearance via Aβ transporters on BBB and alter brain homeostasis that leads to brain-wide neuroinflammation and neuronal injury [12,13,14,15]. Previous studies reported that the damage of BBB integrity participated in AD pathology [16, 17]. The studies by Kook et al. and Wan et al. suggested that oligomeric Aβ1–42 could trigger the decrease of tight junctions and result in barrier integrity injury [18, 19]. Indeed, BBB integrity alterations were detected in the quite early stage even before amyloid plaques deposit and cognitive deficits in AD transgenic mice [20, 21]. Several attempts focusing on protecting BBB function have shown positive effects on AD pathology, suggesting that the BBB could be a potential therapeutic target for AD.
Many studies have demonstrated that omega-3 polyunsaturated fatty acids (ω3-PUFAs) confer benefits in a variety of neurological disorders due to their anti-inflammatory, anti-oxidant, anti-apoptotic and neuroprotective effects [22,23,24,25,26,27,28]. Evidence from a preclinical study suggested that dietary intervention with ω3-PUFAs could reduce AD risk [29]. Moreover, Docosahexaenoic acid (DHA), a major member of long-chain ω3-PUFAs, was found to reduce Aβ deposit in an aged AD mouse model [30]. Very recently, we have reported that ω3-PUFAs could promote glymphatic function to enhance Aβ clearance from the brain [31]. However, clinical research suggested that DHA supplement improved cognition in patients with mild cognition impairment but not AD patients with severe cognition impairment [32], which indicates the importance of an early intervention.
In the present study, we firstly investigated the expression profiles of Aβ-degrading enzymes for Aβ degradation activities and zo-1 for BBB permeability in APP/PS1 transgenic mice at the prodromal stage (prior to the age of 6 months). Our results showed that there were no significant genotype-related alterations in mRNA expression of 4 well-characterized Aβ-degrading enzymes in APP/PS1 mice within the ages of 6 months while there was a significant decrease in zo-1 expression starting from the age of 5 months. We further demonstrated that treatment of fish oil (FO) for 4 weeks remarkably increased zo-1 expression and significantly inhibited the glial activation and NF-κB activation in APP/PS1 mice.
Methods
Animal
APPswe/PS1dE9 C57BL/6 J double-transgenic (APP/PS1) mice at different ages ranging from 1-month to 6-month old and age-match wild type (WT) mice were used in the present study. Male heterozygous APP/PS1 mice were obtained from Jackson Laboratory (Bar Harbor, ME, USA) and used to mate with female C57BL/6 mice to generate heterozygous mice and WT littermates for this research. The genotypes of APP/PS1 animals were identified by standard polymerase chain reaction (PCR) analysis of genomic DNA isolated from mouse tails. All mice were housed in groups and accessed to food and water ad libitum in a 12:12 h light–dark (light on at 8: 00 am) cycle, provided with controlled temperature and humidity.
FO administration
APP/PS1 mice at 4-month and 5-month old received daily intragastrical administration of FO. Each animal received 50 μL FO (containing 13 μM Eicosapentaenoic Acid (EPA) and 99 μM DHA; the purity of EPA + DHA = 80.27%; Wuhan Shengtianyu Biotech Ltd., China) per day lasting for 4 weeks. EPA and DHA were suspended in corn oil which is free from contaminants. The main constituents of corn oil are oleic acid and linoleic acid, which are essential dietary elements for humans. Corn oil is widely used as a safe vehicle in the study of omega-3 polyunsaturated fatty acids. APP/PS1 mice in the control group received daily intragastrical administration of equivoluminal isocaloric corn oil (CO). Age-matched WT mice which received a normal diet served as a normal control.
Fatty acid analysis
To evaluate the effects of the dietary regime on the PUFA composition in the brain, the hippocampal and cortical tissue samples of APP/PS1 mice from fish oil-and corn oil-treated groups (n = 3 per group) were processed for fatty acid analysis by gas chromatography-mass spectrometry (GC–MS) as described previously [33]. Quantifications were performed by an investigator who was blind to the animal grouping and carried out by normalizing individual peak areas as the percentage of total fatty acids.
Tissue preparation
APP/PS1 and WT mice at the age of 1, 2, 3, 4, 5, and 6 months were sacrificed under overdose anesthetic (n = 3 at each time point). After transcardially perfused with ice-cold normal saline, the animal brains were quickly moved out to be placed on ice and then divided into two halves along the middle sagittal sulcus. The cortex and hippocampus of the right half were used to detect the expression of Aβ degrading enzymes by using real-time PCR (RT-PCR), and the cortex and hippocampus of the left half were used to measure the expression of zo-1 by western blot. APP/PS1 mice aged 5 months which received either FO or CO administration for 4 weeks were sacrificed and their brains were isolated for immunohistochemistry (5 mice each group) and western blot analysis (5 mice each group).
Real-time PCR analysis
For isolating RNA from the cortex and hippocampus, TRIzol reagents (Catlog No: RN 190, Thermo Fisher Scientific, USA) were used under the manufacturer’s instructions, followed by RNA quality evaluation with a microplate reader (Thermo Fisher Scientific, USA). Two micrograms of RNA were reversely transcribed using a reverse transcription system kit under the manufacturer’s protocol. RT-PCR was performed in a 20 μL reaction system containing 10 μL TB Green Mix (RR820Q, TB GreenTM premix Ex TaqTM, Kapa Biosystems, USA), 2 μL of cDNA (diluted 20 times with de-enzyme water), 6.6 μL ddH2O, and 0.4 μL 500 nM of each specific primer. The cycling parameters were as follows: 95 °C, 300 s; 95 °C, 10 s; 60 °C, 40 s; 95 °C,10 s; 60 °C, 30 s; and 95 °C, 30 s. The primers used for PCR were shown as follows: CatB, forward: 5′-AAATCAGGAGTATACAAGCATGA-3′, reverse: 5′-GCCCAGGGATGCGGATGG-3′; NEP, forward: 5′- TCCTGACTATCATAGCGGTGAC-3′, reverse: 5′- GACGTTGCGTTTCAACCAGC-3′; IDE, forward: 5′-ACTAACCTGGTGGTGAAG-3′, reverse: 5′- GGTCTGGTATGGGAAATG -3′; MBP, forward:5′-CGGACCCAAGATGAAAACCC-3′, reverse: 5′-AAAGGAAGCCTGGACCACACAG-3′; GADPH, forward: 5′ AACGACCCCTTCATTGAC -3′; reverse:5′- TCCACGACATACTCAGCAC -3′.
Western blot analysis
Proteins of cortex and hippocampus were extracted with lysis buffer containing a protease inhibitor, and a BCA protein assay kit (Catlog No: 23225, Thermo scientific, USA) was used for protein concentration analysis. After separated by electrophoresis on SDS-PAGE gel, sample proteins were transferred onto polyvinylidene fluoride membranes (Catlog No: 1621077, BIO-RAD, USA). The membranes were then incubated with primary and secondary antibodies, followed by incubation with enhanced chemiluminescence solution (Catlog No: RPN2235, GE Healthcare, Sweden) and autoradiography. Primary antibodies included anti-zo-1 (Catlog No: AB2272, EMD Millipore, USA), anti-NFκB-p65 (Catlog No: 8242, cell signaling technology, USA), anti-phosphorylated p65 (p-p65) (Ser536, Catlog No: 3303, cell signaling technology, USA), anti-tubulin (Catlog No: RM2007, Ray Antibody, China), and anti-actin (Catlog No: SC69879, Santa Cruz Biotechnology, USA). All results from chemiluminescence exposure were analyzed with software Image Pro plus 6.0.
Immunofluorescence
Brain tissues post-fixed in 4% PFA were transferred into 20–30% sucrose buffer for 2 days at 4 °C, and were cut into 15 μm coronal sections. Selected coronal sections were incubated with primary antibodies anti-GFAP (Catlog No: 60190, sigma, USA) and anti-Iba-1 (Catlog No: 019-19741, Wako, Japan) overnight after blocked with 10% normal donkey serum (Beyotime technology) at room temperature for 1 h. Species-specific secondary antibodies were then added to the brain sections for 1 h at 37 °C in dark after washed with 0.01 M PBS 3 times. Following washing with 0.01 mol/l PBS, the sections were mounted using Fluoroshield Mounting Medium with DAPI (Catlog No: F6057, Sigma-Aldrich; Merck KGaA, Darmstadt, Germany). The expression of Iba-1 and GFAP was examined using the Olympus fluorescence microscope (20× magnification). Quantification of GFAP labelled astrocytes and Iba-1 labelled microglia was performed using the image analysis programme ImageJ (ImageJ 1.39u, National Institute of Health). For evaluating the average fluorescent density, 3 measuring frames of 1360 × 1024 pixels per section and a total of 5 randomly selected sections per animal were analyzed in a blinded manner by two investigators. The level of immunoreactivity was manifested as the ROI per view that contained immunoreactivity. The image acquirements and data quantifications were performed by an investigator who was blind to the experiment.
Statistical analysis
All data were presented as mean ± SEM, and the graphs were made using GraphPad Prism 6.0. Two-tail student’s t test and one-way ANOVA followed by Turkey post hoc test were used for two-group and multiple-group comparisons respectively. The significant difference level was set 0.05 in all comparisons with SPSS 24.0.
Results
Aβ-degrading enzymes showed no declines before AD onset in APP/PS1 mice
RT-PCR analysis was performed to assess whether there were alterations in mRNA expression of 4 well-identified Aβ-degrading enzymes including CatB, NEP, IDE, and MBP in APP/PS1 mice at the prodromal stage. No continuous alterations in the expression of CatB, NEP, IDE, and MBP were detected in both the hippocampus and the cortex of APP/PS1 mice within the early 6 months (Fig. 1a–d). Furthermore, no alterations on the mRNA expression level of CatB, NEP, IDE, and MBP were found in APP/PS1 mice compared to age-matched WT mice at the age of 1, 2, 3, 4, 5, or 6 months, in both the hippocampus and the cortex (Fig. 1a–d), except for a transient decrease in the expression of IDE in the hippocampus of APP/PS1 mice compared to WT mice at the age of 5 months (Fig. 1c).
No alterations in mRNA expression of Aβ-degrading enzymes before AD onset in APP/PS1 mice. a–d Real-time PCR analysis revealed that no differences in mRNA expression level of were observed in the hippocampus and cortex in APP/PS1 mice aged from 1 to 6 months old compared to aged matched WT mice except for a decreased expression of IDE in the hippocampus of APP/PS1 mice compared to WT mice at the age of 5 months. A: CatB; B: NEP; C: IDE; and D: MBP. (*P < 0.05; n = 3 per group)
FO treatment reversed the declined expression of zo-1 before AD onset in APP/PS1 mice
Changes of zo-1 level in both the hippocampus and cortex in APP/PS1 mice before disease onset were evaluated with Western blot analysis. There was no difference in the expression level of zo-1 between APP/PS1 and WT mice at the age of 1 month (Fig. 2a, b). An unexpected increase in the expression level of zo-1 in 2- and 3-month APP/PS1 mice was found as compared to their age-match WT mice (Fig. 2a, b). A significant decrease in zo-1 expression level was found in both the hippocampus and cortex of APP/PS1 mice at the age of 5 and 6 months compared to their age-matched WT mice (Fig. 2a, b).
Changes of zo-1 level enzymes before AD onset in APP/PS1 mice. a Western blot revealed that zo-1 level was enhanced in the hippocampus of APP/PS1 mice compared to WT at 2- and 3-month old, whereas zo-1 expression level decreased in 5- and 6-month old APP/PS1 mice compared to age-match WT mice *P < 0.05; n = 3 per group). b Western blot revealed that zo-1 level was enhanced in the cortex of APP/PS1 mice compared to WT at 2- and 3-month old, whereas zo-1 expression level decreased in 5- and 6-month old APP/PS1 mice compared to age-match WT mice (*P < 0.05, **P < 0.01; n = 3 per group)
There is evidence suggesting that ω3-PUFAs play an active role in the maintenance of biological membranes integrity and homeostasis [34]. To investigate whether treatment with FO (rich in ω3-PUFAs) could protect BBB integrity and permeability, we treated 4- and 5-month old APP/PS1 mice for 4 weeks. GC–MS showed that the expression level of ω-3 docosahexaenoic acid (DHA) and docosapentaenoic acid (DPA) in the hippocampus and cortex of APP/PS1 mice treated with fish oil for 4 weeks was significantly higher than that in the control group treated with corn oil (Tables 1, 2; n = 3 per group). Accordingly, the ratio of ω-6/ω-3 PUFAs was significantly lower in the fish oil-treated group compared with the corn oil-treated group (Tables 1, 2; n = 3 per group). Western blot analysis showed that FO treatment significantly increased the expression levels of zo-1 in both the hippocampus and cortex of APP/PS1 mice at the age of 5 and 6 months compared with CO-treated APP/PS1 mice (Fig. 3a, b).
FO treatment reversed the declined expression of zo-1 in APP/PS1 mice. a Western blot analysis showed that FO treatment for 4 weeks significantly increased the expression levels of zo-1 in both the hippocampus and cortex of 4-month old APP/PS1 mice compared to CO-treated control animals (**P < 0.01; n = 3 per group). b Western blot analysis showed that FO treatment for 4 weeks significantly increased the expression levels of zo-1 in both the hippocampus and cortex of 5-month old APP/PS1 mice compared to CO-treated control animals (**P < 0.01; n = 3 per group)
FO treatment inhibited glial activation and NF-κB activation in APP/PS1 mice
It is widely considered that neuroinflammation is implicated in AD pathology. For example, microglial activation triggered by Aβ could be observed in early AD [35, 36]. As results, pro-inflammation factors released from activated microglia then triggered complicated cascade reactions, contributing to the disease development. We treated 5-month old APP/PS1 mice with either FO or CO for 4 weeks. FO treatment significantly inhibited glial activation of the cortex region, which was demonstrated by lower relative optical intensity (ROI) of GFAP and Iba-1 staining found in the cortex of FO-treated APP/PS1 mice compared to the CO-treated APP/PS1 mice (Fig. 4a, b).
FO treatment inhiited the glial activation in APP/PS1 mice. a Representative images of GFAP expression in the cortex of the 5-month old APP/PS1 mice treated with FO or CO for 4 weeks and the age-matched WT mice (normal control). Higher relative optical intensity (ROI) of GFAP staining was observed in the cortex of APP/PS1 mice treated with CO compared to the WT mice, whereas FO treatment significantly suppressed astroglial activation in APP/PS1 mice compared to CO treatment (***P < 0.001; n = 5 per group). b Representative images of Iba-1 expression in the cortex of the 5-month old APP/PS1 mice treated with FO or CO for 4 weeks and the age-matched WT mice (normal control). Higher relative optical intensity (ROI) of Iba-1 staining was observed in the cortex of APP/PS1 mice treated with CO compared to the WT mice, whereas FO treatment significantly suppressed microglial activation in APP/PS1 mice compared to CO treatment (*P < 0.05; n = 5 per group). Scale bar: 75 µm
NF-κB activation is a key regulator for stimulating pro-inflammatory gene transcription [37]. Normally p65 combines with p50 as heterodimers in the cytoplasm, and its activity is inhibited by IκB. When IκB is activated and phosphorylated, it will stop suppressing the p65:p50 dimers. The released p65 will be phosphorylated and translocated into the nucleus where it binds with the target DNA and triggers a series of inflammatory genes transcription such as IL-1β, TNF-α, and NLRP3 [38, 39]. As the results showed, a significant elevation in the expression of phosphorylated p65 was observed in both the hippocampus and cortex of the APP/PS1 mice treated with CO compared to WT mice, suggesting that the NF-κB signaling pathway was activated in APP/PS1 mice (Fig. 5a–c). FO treatment significantly suppressed NF-κB activation in APP/PS1 mice as compared to the CO-treated group (Fig. 5a–c).
FO treatment inhibited NF-κB activation in both the hippocampus and cortex region of the APP/PS1 mice. a Representative images of Western blot analysis on the expression of phosphorylated p65 (p-p65, Ser536) and total p65 in the hippocampus region of the 5-month old APP/PS1 mice treated with FO or CO for 4 weeks and the age-matched WT mice (normal control). b Representative images of Western blot analysis on the expression of phosphorylated p65 (p-p65, Ser536) and total p65 in the cortex region of the 5-month old APP/PS1 mice treated with FO or CO for 4 weeks and the age-matched WT mice (normal control). c Quantification analysis revealed that FO treatment significantly suppressed the NF-κB activation found in APP/PS1 mice (*P < 0.05, **P < 0.01; n = 5 per group)
Discussion
During the last decade, failure of clinical trials for AD was announced in succession [40,41,42]. Most of these clinical trials have focused on strategies for treating AD patients with developed symptoms. The failure of these clinical trials suggests that it might be too late to treat AD and an effective treatment for AD might need an early intervention. Exact molecular mechanisms underlying pathophysiological alterations in AD still remain unclear. The amyloid cascade hypothesis is one of the most well-known molecular mechanisms underlying pathophysiological alterations in AD [43]. This hypothesis proposes that Aβ deposits trigger neuronal dysfunction and death in AD.
Accumulating evidence suggests that abnormal Aβ deposits result from an imbalance between production and clearance of Aβ [3, 4]. While pharmacologic inhibition targeted at Aβ production could be effective in reducing Aβ accumulation, Aβ clearance is another effective way to reduce Aβ levels in the brains of AD. A series of Aβ-degrading enzymes have been identified which play key roles in determining cerebral Aβ levels under either physiological or pathophysiological conditions. NEP is one of the principal Aβ-degrading proteases and is the first one identified to be able to efficiently degrade Aβ in animal models [44]. NEP and IDE levels were aberrantly decreased at the dementia stage of AD patients, but not in the preclinical stage of AD patients, and the same results were also found in the APP/PS1 mice [45,46,47], suggesting that Aβ-degrading activities are gradually reduced after disease onset in AD. Interestingly, plaques burden decrease was obviously observed in 14-month APP transgenic mice which genetically overexpressed NEP or IDE [48]. In our study, the expression levels of 4 well-characterized Aβ-degrading enzymes did not decrease at the prodromal stage of AD mice. It was reported that APPSwe/PSEN1(dE9) mice showed contextual memory deficit at the early age of 6 months, while spatial memory impairment occurred at 8–10 months old [49,50,51]. Our results indicated that therapeutic approaches based on Aβ degradation could be designed for reducing cerebral Aβ levels after disease onset.
Several studies have reported that BBB disruption is identified as one of AD pathogeneses [52, 53]. Zo-1, one of the most important tight junctions of BBB, plays an important role in BBB integrity maintenance [54]. Our study demonstrated that the decrease of zo-1 expression in APP/PS1 mice started from 5-month-old, suggesting that the integrity of BBB alters at a quite early stage. Remarkably, FO treatment could counteract the decreased expression of zo-1 when applied to APP/PS1 mice, which provides evidence that ω3-PUFAs could be used as an early intervention agent for protecting BBB integrity in AD. An unexpected elevation of zo-1 expression in 2- and 3- month APP/PS1 mice was observed, but the exact mechanism for this temporary increase remains unknown. We propose that the abnormal production of Aβ in APP/PS1 mice at such an early stage may stimulate the expression level of zo-1 to compensate the dynamic of BBB as previously reported [55].
Neuroinflammation has been well defined in AD and considered as one of crucial AD pathogeneses [56,57,58]. Aβ deposition and Tau fragment could trigger a cascade inflammation [59, 60]. Our study showed that NF-κB was activated APP/PS1 mice at the age of 5 and 6 months. The activated NF-κB is essential for both acute and chronic inflammatory responses. It is widely accepted that ω3-PUFAs and their metabolites such as Resolvin D1 and Neuroprotectin D1 could function as potent anti-inflammatory molecules that suppresses inflammation and helps in the resolution of inflammatory events. Our findings demonstrated that FO supplement could be an early intervention for AD through significantly suppressing glial activation and NF-κB activation. In the pathogenesis of AD, Aβ accumulation induces the glial cell activation and impairs the BBB integrity. Interestingly, the impairment of BBB integrity activates glial cells to secret inflammatory factors, which in turn induces Aβ deposition in the brain of AD [61, 62]. Fish oil shows effects on protecting the BBB integrity and suppressing glial and NF-κB activation, suggesting that fish oil supplement is a promising therapeutic early intervention for AD.
Conclusions
In summary, our study investigated Aβ enzymatic degradation activities and BBB integrity in APP/PS1 mice at the prodromal stage. No significant genotype-related alterations in mRNA expression of Aβ-degrading enzymes were found in APP/PS1 transgenic mice within the ages of 6 months, whereas the protein expression level of zo-1 decreased in 5- and 6-month APP/PS1 transgenic mice compared to their age-matched WT mice. Our study provides evidence that FO supplement could be a potential therapeutic early intervention for AD through protecting the BBB integrity and significantly suppressing glial activation and NF-κB activation.
Availability of data and materials
Please contact corresponding authors for data requests.
Abbreviations
- AD:
-
Alzheimer’s disease
- Aβ:
-
Amyloid beta
- BBB:
-
Blood–brain barrier
- CatB:
-
Cathepsin B
- CO:
-
Corn oil
- DHA:
-
Docosahexaenoic acid
- EPA:
-
Eicosapentaenoic acid
- FO:
-
Fish oil
- IDE:
-
Insulin-degrading enzyme
- MBP:
-
Myelin basic protein
- NEP:
-
Neprilysin
- ω3-PUFAs:
-
Omega-3 polyunsaturated fatty acids
- PCR:
-
Polymerase chain reaction
- RT-PCR:
-
Real-time PCR
- TJ:
-
Tight junction
- WT:
-
Wild type
- zo-1:
-
Zonula occludens-1
References
Karran E, Mercken M, De SB. The amyloid cascade hypothesis for Alzheimer’s disease: an appraisal for the development of therapeutics. Nat Rev Drug Discov. 2011;10(9):698–712.
Martin L, Latypova X, Wilson CM, Magnaudeix A, Perrin M-L, Yardin C, et al. Tau protein kinases: involvement in Alzheimer’s disease. Ageing Res Rev. 2013;12(1):289–309.
Higuchi M, Iwata N, Saido TC. Understanding molecular mechanisms of proteolysis in Alzheimer’s disease: progress toward therapeutic interventions. BBA Proteins Proteomics. 2005;1751(1):60–7.
Wang DS, Dickson DW, Malter JS. β-amyloid degradation and Alzheimer’s Disease. J Biomed Biotechnol. 2006;2006(3):58406.
Tarasoff-Conway JM, Carare RO, Osorio RS, Glodzik L, Butler T, Fieremans E, et al. Clearance systems in the brain-implications for Alzheimer disease. Nat Rev Neurol. 2015;11(8):457–70.
Mueller-Steiner S, Zhou Y, Arai H, Roberson ED, Sun B, Chen J, et al. Antiamyloidogenic and neuroprotective functions of cathepsin B: implications for Alzheimer’s disease. Neuron. 2006;51(6):703–14.
Kanemitsu H, Tomiyama T, Mori H. Human neprilysin is capable of degrading amyloid β peptide not only in the monomeric form but also the pathological oligomeric form. Neurosci Lett. 2003;350(2):113–6.
Qiu WQ, Walsh DM, Ye Z, Vekrellis K, Zhang J, Podlisny MB, et al. Insulin-degrading enzyme regulates extracellular levels of amyloid beta-protein by degradation. J Biol Chem. 1998;273(49):32730.
Liao MC, Ahmed M, Smith SO, Van Nostrand WE. Degradation of amyloid beta protein by purified myelin basic protein. J Biol Chem. 2009;284(42):28917–25.
Funato H, Yoshimura M, Kusui K, Tamaoka A, Ishikawa K, Ohkoshi N, et al. Quantitation of amyloid beta-protein (A beta) in the cortex during aging and in Alzheimer’s disease. Am J Pathol. 1998;152(6):1633–40.
Obermeier B, Daneman R, Ransohoff RM. Development, maintenance and disruption of the blood–brain barrier. Nat Med. 2013;19(12):1584–96.
Fanning AS. Isolation and functional characterization of the actin-binding region in the tight junction protein ZO-1. FASEB J. 2002;16(13):1835–7.
Fanning AS, Jameson BJ, Jesaitis LA, Anderson JM. The tight junction protein ZO-1 establishes a link between the transmembrane protein occludin and the actin cytoskeleton. J Biol Chem. 1998;273(45):29745–53.
Umeda K, Ikenouchi J, Katahira-Tayama S, Furuse K, Sasaki H, Nakayama M, et al. ZO-1 and ZO-2 independently determine where claudins are polymerized in tight-junction strand formation. Cell. 2006;126(4):741–54.
Van Itallie CM, Fanning AS, Bridges A, Anderson JM. ZO-1 stabilizes the tight junction solute barrier through coupling to the perijunctional cytoskeleton. Mol Biol Cell. 2009;20(17):3930–40.
Luissint AC, Artus C, Glacial F, Ganeshamoorthy K, Couraud PO. Tight junctions at the blood brain barrier: physiological architecture and disease-associated dysregulation. Fluids Barriers CNS. 2012;9(1):23.
Dietrich M, Antequera D, Pascual C, Castro N, Bolos M, Carro E. Alzheimer’s disease-like impaired cognition in endothelial-specific megalin-null mice. J Alzheimers Dis Jad. 2014;39(4):711–7.
Wan W, Cao L, Liu L, Zhang C, Kalionis B, Tai X, et al. Aβ(1-42) oligomer-induced leakage in an in vitro bloo–brain barrier model is associated with up-regulation of RAGE and metalloproteinases, and down-regulation of tight junction scaffold proteins. J Neurochem. 2015;134(2):382–93.
Kook SY, Hong HS, Moon M, Chang MH, Chang S, Mook-Jung I. A beta(1-42)-RAGE interaction disrupts tight junctions of the blood–brain barrier via Ca2 + -calcineurin signaling. Intensive Care Med Exp. 2016;4(1):1–15.
Ujiie M, Dickstein DL, Carlow DA, Jefferies WA. Blood—brain barrier permeability precedes senile plaque formation in an Alzheimer Disease model. Microcirculation (New York, 1994). 2003;10(6):463–70.
Montagne A, Zhao Z, Zlokovic BV. Alzheimer’s disease: a matter of blood–brain barrier dysfunction? J Exp Med. 2017;214(11):3151–69.
Liu Q, Wu D, Ni N, Ren H, Luo C, He C, et al. Omega-3 polyunsaturated fatty acids protect neural progenitor cells against oxidative injury. Mar Drugs. 2014;12(5):2341–56.
Luo C, Ren H, Wan JB, Yao X, Zhang X, He C, et al. Enriched endogenous omega-3 fatty acids in mice protect against global ischemia injury. J Lipid Res. 2014;55(7):1288–97.
Shi Z, Ren H, Luo C, Yao X, Li P, He C, et al. Enriched endogenous Omega-3 polyunsaturated fatty acids protect cortical neurons from experimental ischemic injury. Mol Neurobiol. 2016;53(9):6482–8.
Tan Y, Ren H, Shi Z, Yao X, He C, Kang JX, et al. Endogenous docosahexaenoic acid (DHA) prevents abeta1-42 oligomer-induced neuronal injury. Mol Neurobiol. 2016;53(5):3146–53.
Ren H, Yang Z, Luo C, Zeng H, Li P, Kang JX, et al. Enriched endogenous Omega-3 fatty acids in mice ameliorate parenchymal cell death after traumatic brain injury. Mol Neurobiol. 2017;54(5):3317–26.
Shi Z, Ren H, Huang Z, Peng Y, He B, Yao X, et al. Fish oil prevents lipopolysaccharide-induced depressive-like behavior by inhibiting neuroinflammation. Mol Neurobiol. 2017;54(9):7327–34.
Luo C, Ren H, Yao X, Shi Z, Liang F, Kang JX, et al. Enriched Brain omega-3 polyunsaturated fatty acids confer neuroprotection against microinfarction. EBioMedicine. 2018;32:50–61.
Green KN, Martinez-Coria H, Khashwji H, Hall EB, Yurko-Mauro KA, Ellis L, et al. Dietary docosahexaenoic acid and docosapentaenoic acid ameliorate amyloid-beta and tau pathology via a mechanism involving presenilin 1 levels. J Neurosci. 2007;27(16):4385–95.
Hooijmans CR, Zee CEEMV, Dederen PJ, Brouwer KM, Reijmer YD, Groen TV, et al. DHA and cholesterol containing diets influence Alzheimer-like pathology, cognition and cerebral vasculature in APP swe/PS1 dE9 mice. Neurobiol Dis. 2009;33(3):482–98.
Ren H, Luo C, Feng Y, Yao X, Shi Z, Liang F, et al. Omega-3 polyunsaturated fatty acids promote amyloid-beta clearance from the brain through mediating the function of the glymphatic system. FASEB J. 2017;31(1):282–93.
Kotani S, Sakaguchi E, Warashina S, Matsukawa N, Ishikura Y, Kiso Y, et al. Dietary supplementation of arachidonic and docosahexaenoic acids improves cognitive dysfunction. Neurosci Res. 2006;56(2):159–64.
Yan L, Xie Y, Satyanarayanan SK, Zeng H, Liu Q, Huang M, et al. Omega-3 polyunsaturated fatty acids promote brain-to-blood clearance of β-Amyloid in a mouse model with Alzheimer’s disease. Brain Behav Immun. 2019;S0889-1591(18):31175–9.
Bazan NG, Molina MF, Gordon WC. Docosahexaenoic acid signalolipidomics in nutrition: significance in aging, neuroinflammation, macular degeneration, Alzheimer’s, and other neurodegenerative diseases. Annu Rev Nutr. 2011;31:321–51.
Maezawa I, Zimin PI, Wulff H, Jin L-W. Amyloid-β protein oligomer at low nanomolar concentrations activates microglia and induces microglial neurotoxicity. J Biol Chem. 2011;286(5):3693–706.
Jr JC, Knopman DS, Jagust WJ, Petersen RC, Weiner MW, Aisen PS, et al. Tracking pathophysiological processes in Alzheimer’s disease: an updated hypothetical model of dynamic biomarkers. Lancet Neurol. 2013;12(2):207–16.
Hayden MS, Ghosh S. Shared principles in NF-kappaB signaling. Cell. 2008;132(3):344–62.
Giridharan S, Srinivasan M. Mechanisms of NF-κB p65 and strategies for therapeutic manipulation. J Inflamm Res. 2018;11:407–19.
Liu T, Zhang L, Joo D, Sun SC. NF-kappaB signaling in inflammation. Signal Transduct Targeted Ther. 2017;2(1):17023.
Atri A, Frölich L, Ballard C, Tariot P, Molinuevo J, Boneva N, et al. Effect of idalopirdine as adjunct to cholinesterase inhibitors on change in cognition in patients with Alzheimer Disease: three randomized clinical trials. JAMA. 2018;319(2):130–42.
Egan M, Kost J, Tariot P, Aisen P, Cummings J, Vellas B, et al. Randomized trial of verubecestat for mild-to-moderate Alzheimer’s Disease. N Engl J Med. 2018;378(18):1691–703.
Honig L, Vellas B, Woodward M, Boada M, Bullock R, Borrie M, et al. Trial of solanezumab for mild dementia due to Alzheimer’s Disease. N Engl J Med. 2018;378(4):321–30.
Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer’s Disease: progress and problems on the road to therapeutics. Science. 2002;297(5580):353–6.
Iwata N, Tsubuki S, Takaki Y, Watanabe K, Sekiguchi M, Hosoki E, et al. Identification of the major Abeta1-42-degrading catabolic pathway in brain parenchyma: suppression leads to biochemical and pathological deposition. Nat Med. 2000;6(2):143–50.
Fukami S, Watanabe K, Iwata N, Haraoka J, Lu B, Gerard NP, et al. Abeta-degrading endopeptidase, neprilysin, in mouse brain: synaptic and axonal localization inversely correlating with Abeta pathology. Neurosci Res. 2002;43(1):39–56.
Cook DG, Leverenz JB, Mcmillan PJ, Kulstad JJ, Ericksen S, Roth RA, et al. Reduced hippocampal insulin-degrading enzyme in late-onset Alzheimer’s disease is associated with the apolipoprotein E-epsilon4 allele. Am J Pathol. 2003;162(1):313–9.
Wang S, Wang R, Chen L, Bennett DA, Dickson DW, Wang DS. Expression and functional profiling of neprilysin, insulin-degrading enzyme, and endothelin-converting enzyme in prospectively studied elderly and Alzheimer’s brain. J Neurochem. 2010;115(1):47–57.
Leissring MA, Farris W, Chang AY, Walsh DM, Wu X, Sun X, et al. Enhanced proteolysis of beta-amyloid in APP transgenic mice prevents plaque formation, secondary pathology, and premature death. Neuron. 2003;40(6):1087–93.
Kilgore M, Miller CA, Fass DM, Hennig KM, Haggarty SJ, Sweatt JD, et al. Inhibitors of class 1 histone deacetylases reverse contextual memory deficits in a mouse model of Alzheimer’s disease. Neuropsychopharmacology. 2010;35(4):870–80.
Jankowsky JL, Melnikova T, Fadale DJ, Xu GM, Slunt HH, Gonzales V, et al. Environmental enrichment mitigates cognitive deficits in a mouse model of Alzheimer’s disease. J Neurosci. 2005;25(21):5217–24.
Minkeviciene R, Ihalainen J, Malm T, Matilainen O, Keksa-Goldsteine V, Goldsteins G, et al. Age-related decrease in stimulated glutamate release and vesicular glutamate transporters in APP/PS1 transgenic and wild-type mice. J Neurochem. 2008;105(3):584–94.
Kook SY, Seok Hong H, Moon M, Mook-Jung I. Disruption of blood–brain barrier in Alzheimer disease pathogenesis. Tissue Barriers. 2013;1(2):e23993.
Chan Y, Chen W, Wan W, Chen Y, Li Y, Zhang C. Abeta1-42 oligomer induces alteration of tight junction scaffold proteins via RAGE-mediated autophagy in bEnd. 3 cells. Exp Cell Res. 2018;369(2):266–74.
Wolburg H, Lippoldt A. Tight junctions of the blood brain barrier: development, composition and regulation. Vascul Pharmacol. 2002;38(6):323–37.
Keaney J, Campbell M. The dynamic blood–brain barrier. FEBS J. 2015;282(21):4067–79.
Eikelenboom P, Veerhuis R, van Exel E, Hoozemans JJ, Rozemuller AJ, van Gool WA. The early involvement of the innate immunity in the pathogenesis of late-onset Alzheimer’s disease: neuropathological, epidemiological and genetic evidence. Curr Alzheimer Res. 2011;8(2):142–50.
Sastre M, Richardson JC, Gentleman SM, Brooks DJ. Inflammatory risk factors and pathologies associated with Alzheimer’s disease. Curr Alzheimer Res. 2011;8(2):132–41.
Levit A, Allman BL, Rajakumar N, Hachinski V, Whitehead SN. Age-dependent white matter inflammation and cognitive impairment in the TgAPP21 rat model of alzheimer disease. Neurology. 2018;90:P2.184.
Kovac A, Zilkova M, Deli MA, Zilka N, Novak M. Human truncated tau is using a different mechanism from amyloid-beta to damage the blood–brain barrier. J Alzheimers Dis Jad. 2009;18(4):897–906.
Gonzalezvelasquez FJ, Kotarek JA, Moss MA. Soluble aggregates of the amyloid-beta protein selectively stimulate permeability in human brain microvascular endothelial monolayers. J Neurochem. 2010;107(2):466–77.
Erickson MA, Banks WA. Blood–brain barrier dysfunction as a cause and consequence of Alzheimer’s disease. J Cereb Blood Flow Metab. 2013;33(10):1500–13.
Marques F, Sousa JC, Sousa N, Palha JA. Blood–brain-barriers in aging and in Alzheimer’s disease. Mol Neurodegen. 2013;8:38.
Acknowledgements
Not applicable.
Funding
This study was supported by the grants from The National Key Research and Development Program of China (2017YFC0907703), the Southern China International Cooperation Base for Early Intervention and Functional Rehabilitation of Neurological Diseases (2015B050501003), Guangdong Provincial Engineering Center For Major Neurological Disease Treatment, Guangdong Provincial Translational Medicine Innovation Platform for Diagnosis and Treatment of Major Neurological Disease, Guangdong Provincial Clinical Research Center for Neurological Diseases, Macao Science and Technology Development Fund (020/2017/A1 and 039/2017/AFJ), and multi-year research grant, University of Macau MYRG2018-00242-ICMS and MYRG2019-00160-ICMS.
Author information
Authors and Affiliations
Contributions
YX, HS, and XY contributed to the conception and design of the study; YX, LY, and WC performed the experiments; JW, DW, ZC and JL organized the database and performed the statistical analysis; YX, HS and XY wrote the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All procedures in this study were approved and supervised by the animal research ethical committee of Sun Yat-Sen University, and strictly obeyed the rules of animal experiment ethic to reduced number as well as suffering of animals.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xie, Y., Yan, L., Zeng, H. et al. Fish oil protects the blood–brain barrier integrity in a mouse model of Alzheimer’s disease. Chin Med 15, 29 (2020). https://doi.org/10.1186/s13020-020-00314-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13020-020-00314-0