Abstract
Background
Long-acting β2-adrenoceptor agonists have been shown to increase the risk of atrial arrhythmias in patients with stable chronic obstructive pulmonary disease. The aim of this study was to investigate whether perioperative long-acting β2-adrenoceptor agonists treatment would increase the risk of postoperative atrial arrhythmias after lung cancer surgery in chronic obstructive pulmonary disease patients.
Methods
We retrospectively analyzed 174 consecutive chronic obstructive pulmonary disease patients with non-small-cell lung cancer who underwent lobectomy or segmentectomy. The subjects were divided into those with or without perioperative long-acting β2-adrenoceptor agonists treatment. Postoperative cardiopulmonary complications were compared between the two groups.
Results
There were no statistically significant differences between the perioperative long-acting β2-adrenoceptor agonists treatment group and the control group in the incidence of postoperative atrial arrhythmias (P = 0.629). In 134 propensity-score–matched pairs, including variables such as age, gender, comorbidities, smoking history, operation procedure, lung-cancer staging, and respiratory function, there were no significant differences between the two groups in the incidence of postoperative cardiopulmonary complications, including atrial arrhythmias.
Conclusions
Perioperative administration of long-acting β2-adrenoceptor agonists might not increase the incidence of postoperative atrial arrhythmias after surgical resection for non-small-cell lung cancer in chronic obstructive pulmonary disease patients.
Similar content being viewed by others
Background
Chronic obstructive pulmonary disease (COPD) is primarily characterized by the presence of airflow limitation resulting from parenchymal destruction (emphysema) and airway remodeling [1]. Therefore, the mainstay of pharmacological treatment in stable COPD are bronchodilators, such as long-acting β2-adrenoceptor agonists (β2-agonists) and long-acting muscarinic antagonists [2]. These bronchodilators have been shown to improve symptoms, quality-of-life, pulmonary function and mortality in patients with COPD.
COPD cases are often complicated by lung cancer, because both conditions are strongly associated with cigarette smoking [3]. With the improvement in mortality from COPD itself due to bronchodilators, lung cancer has come to be one of the most important problems in COPD. Surgical operation is the first-choice treatment in COPD patients with resectable lung cancer. However, atrial arrhythmias often occur as a postoperative complication following thoracic surgery [4] and may be associated with an increased risk of cerebral embolism, since the administration of anticoagulation therapy must be balanced against the risk of bleeding. Therefore, postoperative atrial arrhythmias should be avoided in COPD patients with lung cancer who undergo surgical resection.
There are several reasons why atrial arrhythmias often occur after surgical operation for lung cancer in COPD patients. One is that COPD itself is a risk factor for postoperative atrial arrhythmias [5]. Another reason is that lung cancer surgery also entails a risk of postoperative atrial arrhythmias. According to recent studies, the arrhythmias result from the synergic action of increased vagal tone, atrial inflammation, pulmonary hypertension, right heart strain, hypoxemia, and anatomical substrate, such as surgical damage to the cardiac plexus or to the proximal trunks of the pulmonary veins [6, 7]. Moreover, several reports have shown that β2-agonists increase the risk of atrial arrhythmias in COPD patients who do not undergo surgery [8, 9]. However, the effects of β2-agonists treatment during the perioperative period on postoperative atrial arrhythmias after lung cancer surgery have not been elucidated.
The aim of this study was to investigate whether perioperative β2-agonists treatment would increase the risk of postoperative atrial arrhythmias after pulmonary resection for non-small-cell lung cancer (NSCLC) in chronic obstructive pulmonary disease patients.
Methods
Patient selection
We conducted a retrospective analysis of the COPD patients diagnosed with NSCLC who underwent surgery at the Tazuke Kofukai Medical Research Institute, Kitano Hospital, between January 2007 and December 2014. The exclusion criteria were as follows: no pathological confirmation of NSCLC, lesser resection (wedge resection), repeated pulmonary resection, pneumonectomy, chronic atrial arrhythmias before surgery, evidence of infection such as pneumonia before surgery, thyroid dysfunction, and renal failure requiring hemodialysis [10,11,12]. COPD was diagnosed on the basis of the Global Initiative for Chronic Obstructive Lung Disease (GOLD) [13]. The results of the perioperative β2-agonists treatment group (β2-agonists group) and non-β2-agonists treatment group (control group) were compared and analyzed regarding postoperative cardiopulmonary complications. The patients were on continuous electrocardiogram monitoring from surgery day to a week after surgery. After a week, we evaluate postoperative cardiopulmonary complications by intermittent monitoring and examinations. In the perioperative β2-agonists treatment group, the subjects received tulobuterol tape (2 mg/day), inhaled indacaterol (150 μg/day), or inhaled salmeterol (100 μg/day) from more than 2 weeks before surgery until at least a month after surgery, without interruption. The data from the respiratory function tests performed before and after perioperative β2-agonists treatment were compared in the few cases where such data were tracked.
Study approval was granted by the ethics committee of the Tazuke Kofukai Medical Research Institute, Kitano Hospital, in accordance with the Declaration of Helsinki.
Surgical procedure
All patients underwent lobectomies or segmentectomies with anterolateral thoracotomy, posterolateral thoracotomy, or video-assisted thoracic surgery (VATS). For VATS, three access ports were placed through 2–3 cm axillary skin incisions. One of these incisions was extended by 4–5 cm, and the resected lung was removed in a plastic bag without using a rib spreader. Patients requiring conversion from VATS to thoracotomy were classified as open thoracotomy patients.
Postoperative cardiopulmonary complications
All patients were followed-up after surgery, and complications occurring during the same hospitalization as the index procedure were recorded. Cardiopulmonary complications were defined as previously described [10] and included cardiovascular complications, such as arrhythmias (atrial fibrillation [AF], paroxysmal supraventricular tachycardia [PSVT], ventricular tachycardia [VT]), angina pectoris, acute myocardial infarction (AMI), congestive heart failure (CHF), thromboembolic events; and respiratory complications such as pneumonia (fever >38 °C, purulent sputum, abnormal findings on chest X-ray), atelectasis with bronchoscopic therapy, acute respiratory distress syndrome (ARDS) (partial pressure of oxygen in arterial blood-fraction of inspired oxygen <300 mmHg), respiratory insufficiency requiring tracheostomy, and respiratory failure requiring mechanical ventilation. As prolonged air leak and bronchopleural fistulas are considered surgical factors, they were excluded.
Endpoints
The primary endpoint was the incidence of postoperative atrial arrhythmias (AF and PSVT) after surgical resection. Secondary endpoint was the incidence of the other cardiopulmonary complications after surgical resection.
Statistical analysis
The data are presented as mean ± standard deviation. Categorical variables are shown as percentages of the sample. Continuous variables were compared using the Welch’s t test and categorical variables using the Fisher’s exact test or chi-squared test. Propensity score matching was applied to balance the assignment of patients for correct evaluation of the effects of β2-agonists treatment during the perioperative period. The variables were age, gender, comorbidities, smoking history, operation procedure, lung-cancer staging, and respiratory function. Univariate logistic regression analyses were performed for postoperative atrial arrhythmias to observe Type 1 error. We assessed the time free of postoperative atrial arrhythmias using Kaplan–Meier analysis. Differences between term curves were tested for statistical significance using the two-tailed log-rank test. All data were processed and analyzed using SPSS version 20.0 (SPSS, Chicago, IL, USA) or the statistical software R version 3.0.3 (R Foundation for statistical computing, Vienna, Austria). All P-values are 2-sided, and P-values < 0.1 were considered statistically significant.
Results
Subjects
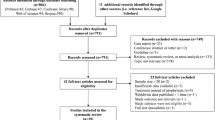
Data from the 191 COPD patients diagnosed with NSCLC who underwent surgery at our hospital between January 2007 and December 2014 were obtained from the hospital’s database. Seventeen patients were excluded because of lesser resection (wedge resection) (n = 4), pneumonectomy (n = 8), and chronic atrial arrhythmias before surgery (n = 5). Thus, 174 patients were included in this study. The clinicopathological characteristics of patients are shown in Table 1. There were no significant differences in age, gender, comorbidities, smoking history, surgical procedure, or lung cancer staging between the perioperative β2-agonists group and the control group. However, there were statistically significant differences between the two groups in forced expiratory volume in 1 s (FEV1) and the ratio of FEV1 to forced vital capacity (FVC). Furthermore, %FEV1 after administration of β2-agonists was significantly increased compared with %FEV1 before administration of β2-agonists (Fig. 1).
Postoperative cardiopulmonary complications
Postoperative cardiopulmonary complications are shown in Table 2. Atrial arrhythmias (AF and PSVT) were the most frequent complication. There were no events of VT, angina pectoris, CHF, or ARDS. There were no statistically significant differences between the two groups in the incidence of cardiovascular complications, AF, PSVT, AMI, thromboembolic events, respiratory complications, pneumonia, atelectasis, respiratory insufficiency, or respiratory failure.
Evaluation of postoperative atrial arrhythmias between perioperative β2-agonists treatment group and control group using propensity score-matched analysis
Propensity score matching was used and variables such as age, gender, comorbidities, smoking history, operation procedure, lung cancer staging, and respiratory function were included, because it was possible that these factors affected the incidence of postoperative cardiopulmonary complications [11]. The perioperative β2-agonists treatment group and control group were well matched (67 patients each), without significant differences in clinical factors (Table 3). The effect size and bias reduction were shown in Table 4. The effect sizes and the mean bias reduction were well validated. There were no statistically significant differences between the two groups in the limited analysis of patients with cardiopulmonary complications including atrial arrhythmias (Table 5). Univariate logistic regression analyses showed there were no statistically significant associations between atrial arrhythmias and other cardiopulmonary complications (Additional file 1: Table S1). Kaplan–Meier analysis was performed to determine whether perioperative β2-agonists treatment had an effect on postoperative atrial arrhythmias after lung cancer surgery in the COPD patients. There were no statistically significant differences between the two groups in the time free of postoperative atrial arrhythmias (P = 0.573; Fig. 2).
Kaplan–Meier analyses of the incidence of postoperative atrial arrhythmias in the patients after propensity score matching, stratified by perioperative treatment with long-acting β2-adrenoceptor agonists (β2-agonists). There were no statistically significant differences between the two groups in the time free of postoperative atrial arrhythmias (P = 0.573)
Power calculation
We calculated that a two-tailed t test with a 10% significance level and 80% power would require 2095 patients for the primary endpoint of the present study. Therefore, 174 patients (β2-agonists group: 71 and control group: 103, and incidence of atrial arrhythmias of the subjects β2-agonists group: 7 and control group: 8) in the present study were considered low power.
Discussion
In this retrospective observational study, the perioperative administration of β2-agonists did not increase the incidence of postoperative atrial arrhythmias (AF and PSVT) after surgical resection for NSCLC in patients with COPD. The incidence of other postoperative cardiopulmonary complications such as VT, angina pectoris, AMI, CHF, thromboembolic events, pneumonia, atelectasis, ARDS, respiratory insufficiency and respiratory failure was also not increased by the perioperative administration of β2-agonists.
β2-agonists are among the first-choice drugs for the treatment of patients with stable COPD [2]. Several reports have shown that treatment with β2-agonists increased the risk of atrial arrhythmias in stable COPD patients [8, 9]. The mechanism involves β2-agonists’s stimulation of the β1-adrenoceptor of the cardiac conduction system. β2-agonists are usually administered using inhaler devices and have high selectivity for the β2-adrenoceptor [14]. However, they can cause adverse systemic effects, such as atrial arrhythmias, by migrating from lung to blood and stimulating the β1-adrenoceptor of the cardiac conduction system.
On the other hand, β2-agonists may have various beneficial effects on atrial arrhythmias. First, postoperative atrial arrhythmias are considered to result from right heart strain [6, 7]. β2-agonists have a strong bronchodilation effect that leads to amelioration of right heart strain by modifying the hyperinflation in patients with stable COPD [15]. Therefore, the bronchodilation of β2-agonists may reduce the risk of atrial arrhythmias in patients with stable COPD. Second, in the perioperative period, a low predicted postoperative FEV1 has been shown to be the best indicator of patients at high risk for pulmonary resection surgery [16]. Suzuki et al. showed that significant FEV1 improvement was observed after the use of perioperative bronchodilator treatment in lung cancer patients with COPD [17]. In the present study, %FEV1 improved significantly after perioperative β2-agonists treatment in the few cases whose data was tracked (P < 0.001; Fig. 1). Therefore, perioperative β2-agonists treatment might improve FEV1, resulting in a protective effect against postoperative cardiopulmonary complications such as atrial arrhythmias. These harmful and beneficial effects of β2-agonists on atrial arrhythmias might cancel each other out. In the present study, the perioperative administration of β2-agonists did not increase the incidence of postoperative atrial arrhythmias after surgical resection for NSCLC in patients with COPD.
The incidence rate of atrial arrhythmias after pulmonary resection in the present study was about 9%. Compared with other studies (10–12%) [18, 19], this rate was a little low. Because the patients having risk factors of atrial arrhythmias were excluded in the criteria, low incidence rate of atrial fibrillation might be found.
We acknowledge limitations of the present study. First, the present study was retrospective. Second, the present study was limited by being merely a small sample size and low power to investigate the effect of β2-agonists on atrial arrhythmias, rather than a randomized controlled interventional trial. To compensate for these limitations, we performed a propensity score matching analysis. These analyses indicated that perioperative β2-agonists treatment was not correlated with the risk of postoperative atrial arrhythmias in COPD patients with NSCLC.
Conclusions
This study showed that the association between perioperative β2-agonists treatment and the risk of postoperative atrial arrhythmias after pulmonary resection for NSCLC in COPD patients. Perioperative administration of β2-agonists might not increase the incidence of postoperative atrial arrhythmias after surgical resection for NSCLC in COPD patients. Further prospective studies with a larger number of patients from multiple institutions will be required to confirm the present findings.
Abbreviations
- AF:
-
Atrial fibrillation
- AMI:
-
Acute myocardial infarction
- ARDS:
-
Acute respiratory distress syndrome
- CHF:
-
Congestive heart failure
- COPD:
-
Chronic obstructive pulmonary disease
- FEV1 :
-
Forced expiratory volume in 1 s
- FVC:
-
Forced vital capacity
- GOLD:
-
Global Initiative for Chronic Obstructive Lung Disease
- NSCLC:
-
Non-small-cell lung cancer
- PSVT:
-
Paroxysmal supraventricular tachycardia
- VATS:
-
Video-assisted thoracoscopic surgery
- VT:
-
ventricular tachycardia
References
Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Respir J. 2009;33:1165–85.
Calverley PM, Anderson JA, Celli B, Ferguson GT, Jenkins C, Jones PW, et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007;356:775–89.
Young RP, Hopkins RJ, Christmas T, Black PN, Metcalf P, Gamble GD. COPD prevalence is increased in lung cancer, independent of age, sex and smoking history. Eur Respir J. 2009;34:380–6.
Curtis JJ, Parker BM, McKenney CA, Wagner-Mann CC, Walls JT, Demmy TL, et al. Incidence and predictors of supraventricular dysrhythmias after pulmonary resection. Ann Thorac Surg. 1998;66:1766–71.
Sekine Y, Kesler KA, Behnia M, Brooks-Brunn J, Sekine E, Brown JW. COPD may increase the incidence of refractory supraventricular arrhythmias following pulmonary resection for non-small cell lung cancer. Chest. 2001;120:1783–90.
Ritchie AJ, Bowe P, Gibbons JR. Prophylactic digitalization for thoracotomy: a reassessment. Ann Thorac Surg. 1990;50:86–8.
Rena O, Papalia E, Oliaro A, Casadio C, Ruffini E, Filosso PL, et al. Supraventricular arrhythmias after resection surgery of the lung. Eur J Cardiothorac Surg. 2001;20:688–93.
Hanrahan JP, Grogan DR, Baumgartner RA, Wilson A, Cheng H, Zimetbaum PJ, et al. Arrhythmias in patients with chronic obstructive pulmonary disease (COPD): occurrence frequency and the effect of treatment with the inhaled long-acting beta2-agonists arformoterol and salmeterol. Medicine (Baltimore). 2008;87:319–28.
Gershon A, Croxford R, Calzavara A, To T, Stanbrook MB, Upshur R, et al. Cardiovascular safety of inhaled long-acting bronchodilators in individuals with chronic obstructive pulmonary disease. JAMA Intern Med. 2013;173:1175–85.
Nojiri T, Inoue M, Yamamoto K, Maeda H, Takeuchi Y, Funakoshi Y, et al. B-type natriuretic Peptide as a predictor of postoperative cardiopulmonary complications in elderly patients undergoing pulmonary resection for lung cancer. Ann Thorac Surg. 2011;92:1051–5.
Nojiri T, Inoue M, Yamamoto K, Maeda H, Takeuchi Y, Nakagiri T, et al. Inhaled tiotropium to prevent postoperative cardiopulmonary complications in patients with newly diagnosed chronic obstructive pulmonary disease requiring lung cancer surgery. Surg Today. 2014;44:285–90.
Yamanashi K, Marumo S, Shoji T, Fukui T, Sumitomo R, Otake Y, et al. The relationship between perioperative administration of inhaled corticosteroid and postoperative respiratory complications after pulmonary resection for non-small-cell lung cancer in patients with chronic obstructive pulmonary disease. Gen Thorac Cardiovasc Surg. 2015;63:652–9.
Vestbo J, Hurd SS, Agusti AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–65.
Currie GP. Indacaterol Novartis/skyePharma. Curr Opin Investig Drugs. 2006;7:457–63.
O’Donnell DE, Casaburi R, Vincken W, Puente-Maestu L, Swales J, Lawrence D, et al. Effect of indacaterol on exercise endurance and lung hyperinflation in COPD. Respir Med. 2011;105:1030–6.
Kearney DJ, Lee TH, Reilly JJ, DeCamp MM, Sugarbaker DJ. Assessment of operative risk in patients undergoing lung resection. Importance of predicted pulmonary function. Chest. 1994;105:753–9.
Suzuki H, Sekine Y, Yoshida S, Suzuki M, Shibuya K, Takiguchi Y, et al. Efficacy of perioperative administration of long-acting bronchodilator on postoperative pulmonary function and quality of life in lung cancer patients with chronic obstructive pulmonary disease. Preliminary results of a randomized control study. Surg Today. 2010;40:923–30.
Ivanovic J, Maziak DE, Ramzan S, McGuire AL, Villeneuve PJ, Gilbert S, et al. Incidence, severity and perioperative risk factors for atrial fibrillation following pulmonary resection. Interact Cardiovasc Thorac Surg. 2014;18:340–6.
Iwata T, Nagato K, Nakajima T, Suzuki H, Yoshida S, Yoshino I. Risk factors predictive of atrial fibrillation after lung cancer surgery. Surg Today. 2016;46:877–86.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
We have one supplemental table.
Authors’ contribution
KY partecipated substantially in in conception, design, and execution of the study. SM was a major contributor in writing the manuscript. TS partecipated in data collection and in the analysis and interpretation of data. RS partecipated in data collection. MF partecipated in conception and design of the study. TK analyzed and interpreted the patient data. CH partecipated in conception of the study. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
Study approval was granted by the ethics committee of the Tazuke Kofukai Medical Research Institute, Kitano Hospital (P15-02-008).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Table S1.
Univariate logistic regression analysis for postoperative atrial arrhythmias after propensity score-matched analysis (DOCX 17 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yamanashi, K., Marumo, S., Sumitomo, R. et al. Long acting β2-adrenocepter agonists are not associated with atrial arrhythmias after pulmonary resection. J Cardiothorac Surg 12, 35 (2017). https://doi.org/10.1186/s13019-017-0606-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13019-017-0606-4